Non-Ophthalmological Diagnosis of Posterior Dislocation of the Intraocular Lens
Funding: The authors received no specific funding for this work.
ABSTRACT
In case of sudden unilateral vision loss, a detailed search for symptoms and causes is mandatory. Dislocation of the intraocular lens can occur even in the absence of trauma and sometimes is not easily detectable, but must be carefully investigated and treated.
1 Introduction
Reduction or loss of vision is a dramatic event, frequently related to neurological or cardiovascular comorbidities, especially when the patient is a smoker, diabetic, hypertensive, or obese. Horton's temporal arteritis and ischemic optic neuropathy are often indicated as etiopathogenetic mechanisms and are widely described in the literature. However, there are situations in which the possible cause must be sought elsewhere and is less complex than expected.
2 Discussion
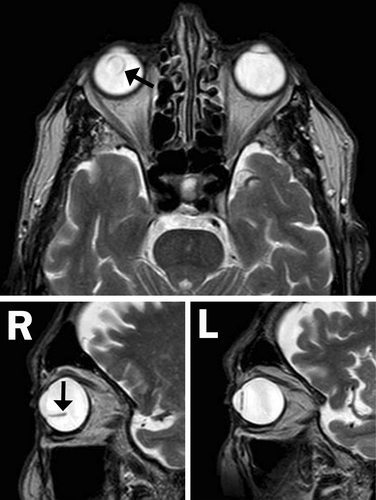
An 83-year-old male patient, previously operated on for bilateral vitrectomy and cataract, suffered a sudden loss of vision in the right eye, announced only by the shaded observation of a horizontal line. In addition, the patient reported occasional and very brief recovery of vision in the right eye during the days following the above event. The patient was in excellent clinical condition, had never smoked, and had no significant comorbidities. Repeated ophthalmological visits with slit-lamp and fundus examinations revealed no apparent alterations. Brain CT scan, supra-aortic trunks Doppler ultrasound, and blood tests, including ESR and CRP, were normal. An angio-MRI of the brain and orbits did not show neurological or circulatory abnormalities. Nevertheless, the hypothesis of ischemic optic neuropathy was formulated, also supported by neurological consultation and literature. High-dose steroids, heparin, and neuroprotectors were then administered, but the treatment was ineffective. Consequently, the patient was determined to perform further investigations. A refractometric test demonstrated partial vision recovery through a very high hyperopic correction. Following this finding, a more careful observation of the T2-weighted MRI sequences (Figure 1) showed an unexpected posterior dislocation of the right intraocular lens, with the capsular bag floating in the vitreous. This non-ophthalmological evidence allowed us to formulate the correct diagnosis with certainty [1]. Finally, the patient underwent surgical lens replacement with anterior chamber reimplantation, achieving recovery of vision and reversal of a condition initially deemed incurable.
Author Contributions
Guido Carillio: writing – original draft, writing – review and editing. Pier Paolo Arcuri: validation, visualization. Flora Carillio: validation, visualization.
Acknowledgments
Dedicated to my father.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.