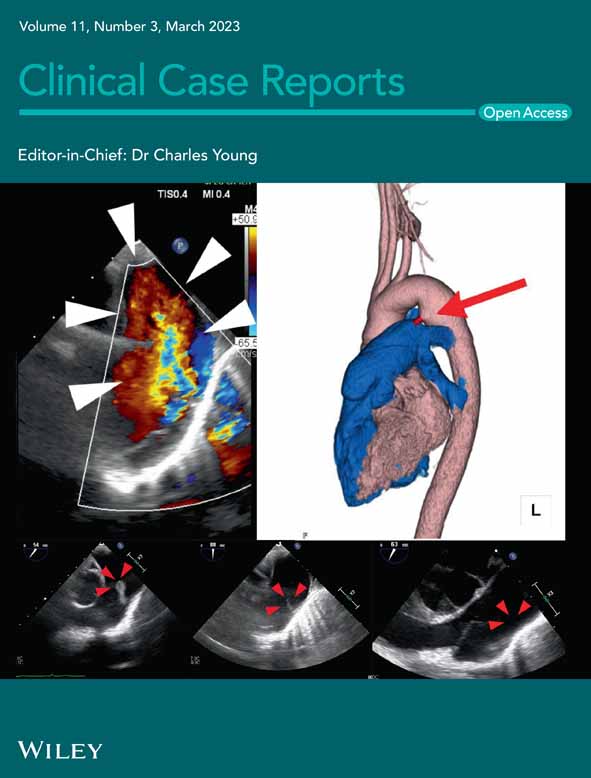
Kounis syndrome following multiple wasp stings: A case report
Abstract
This is a case of Kounis syndrome with chest tightness, lightheadedness, unconsciousness, and features of shock following multiple wasp stings. Despite cardiopulmonary resuscitation and management of allergic and cardiac symptoms, the patient died. Kounis syndrome should be suspected when a patient presents with allergic symptoms and acute coronary syndrome.
1 INTRODUCTION
The wasp is a medically important insect belonging to the Hymenoptera order and Vespidae family that injects venom via stingers and can cause multiple stings as they do not have a barbed stinger.1, 2 Wasp sting causes local inflammatory reactions in the form of pain, swelling, redness, and increased warmth mediated by histamine release from mast cells and basophils. Clinically, it can present as a localized allergic reaction to severe systemic manifestations like anaphylaxis, acute kidney injury, rhabdomyolysis, and disseminated intravascular coagulation.3, 4 Among such systemic manifestations is a rare presentation, called Kounis syndrome. It is the simultaneous occurrence of acute coronary syndrome with hypersensitivity reactions following exposure to foods, drugs, environmental, or other triggers.5, 6
Herein, we present a unique case of Kounis syndrome following multiple wasp stings in a 48-year-old male in Nepal. Kounis syndrome is hardly seen during clinical practice due to the rarity of the disorder. Thus, the message of this study is that Kounis syndrome should be suspected when a patient presents with allergic symptoms and acute coronary syndrome concurrently, which will help diagnose and manage the case early.
2 CASE PRESENTATION
A 48-year-old male from Suryabinayak, Nepal presented to the emergency department of Scheer Memorial Adventist Hospital (SMAH), Banepa, Nepal at 8:30 am on the 16th of July 2022 with the alleged history of being stung by around 40–50 wasps while he went to drink water from the tap in his garden. Immediately following the event, he complained of pain all over his body and ran into the house. He eventually complained of lightheadedness and chest tightness, patient was rushed to the hospital but lost consciousness and became unresponsive on the way to the hospital about 10 min before his arrival at the emergency department of SMAH. There was no history of seizure-like activity and no history of any known allergies or cardiac illnesses in the past.
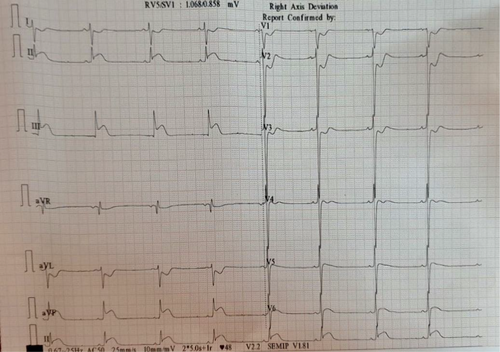
He was brought to the emergency department about 20 min following the sting. On examination at the emergency room, his Glasgow Coma Scale (GCS) was 3/15, pupils were fixed and dilated, the pulse was very feeble, blood pressure could not be recorded, and oxygen saturation (SPO2) was unrecordable. Multiple punctuated sting marks could be observed all over the body including the face. An electrocardiogram (ECG) done immediately showed ST-elevation in the inferior leads while ST depressions in leads I, aVL, V1, V2, and V3 (Figure 1). Immediately cardiopulmonary resuscitation (CPR) was initiated with adrenaline, and the patient was intubated. The CPR was continued for 3 cycles with the return of spontaneous circulation. He was also given an injection of hydrocortisone 200 mg intravenous (IV), an injection of pheniramine maleate 45.5 mg IV along with the injection of enoxaparin (low molecular weight heparin) 60 mg subcutaneous, clopidogrel tablet, and tablet of aspirin with other supportive treatment for acute ST-elevation myocardial infarction.
The patient was admitted to the intensive care unit (ICU) and kept under ventilator support. His arterial blood gas (ABG) analysis showed severe metabolic acidosis for which he was given sodium bicarbonate. His aspartate transaminase (AST) level was 452 U/L and the alanine transaminase (ALT) level was 595 U/L while the rest of the blood investigations were within normal range. He was started on inotropes for low blood pressure but despite the maximum dose of inotropes, optimum blood pressure could not be obtained. His saturation was below 70% with maximum ventilator support, and his heart rate fluctuated between 130 and 140 beats per minute.
At 10:30 am, the patient had frank bleeding from the nose and the mouth. The low molecular heparin and antiplatelet agents were stopped. Despite all the efforts, the patient's condition gradually deteriorated and did not respond to the treatment. At 4:30 pm on the same day, the patient went into asystole and was declared dead.
3 DISCUSSION
The wasp sting is an important occupational hazard in rural Nepal. A study done in a tertiary hospital in Nepal showed 11 cases of wasp sting over a period of 21 months,7 while another study in a referral hospital in Nepal showed 18 cases of wasp sting over a period of 5 years.1
The venom of wasp sting constitutes peptides and amines (histamine, bradykinin, serotonin, leukotrienes, thromboxane) which have inflammatory, vasoactive, and thrombogenic properties. It also contains allergenic proteins like hyaluronidase, acid phosphatase, and phospholipase. These factors promote coronary vasospasm, platelet aggregation, and thrombosis which compromises the coronary blood flow.8, 9 Apart from the direct action of the venom, the wasp sting can cause an allergic response mediated by histamine released from mast cells and basophils during the allergic process, which acts on H1 and H2 receptors in the cardiac chambers and coronary arteries to cause coronary vasospasm that limits coronary blood flow.8, 10 Accounting for the role of mast cells in the pathophysiology of Kounis syndrome, mast cell stabilizers could prevent coronary and cerebrovascular events.11
The concept of allergic angina, also known as Kounis syndrome, was first described in 1991 by Kounis and Zafras when they noticed findings suggestive of allergic angina with an acute allergic reaction.8, 10 When chest pain and allergic reaction occur together with clinical and laboratory findings of classical angina pectoris, it is suggestive of Kounis syndrome.10 A patient can present with symptoms of chest discomfort, dyspnea, faintness, pruritus, and urticaria, and signs like hypotension, bradycardia, diaphoresis, and pallor.10 Our patient presented with chest tightness, lightheadedness, hypotension, and bradycardia. Electrocardiogram findings vary from ST-segment elevation or depression to arrhythmias, and conduction defects.10, 12 Our case had ST-segment elevation in inferior leads and depression in leads I, aVL, V1, V2, and V3. After a cardiology workup, an allergy workup to assess other allergies to food, drugs, and environmental agents is also important.13
A case of 15-year-old male from Turkey14 also presented with Kounis syndrome due to a wasp sting similar to our case. Apart from wasp stings, Kounis syndrome can be caused by drugs (analgesics, anesthetics, antibiotics, NSAIDs, and losartan), foods (fish, fruits, vegetables, and canned food), and environmental exposures (scorpion sting and snake bite).13 Drug intoxication like propafenone poisoning15 can present with features of shock, unconsciousness, and ECG changes, a presentation similar to our case. So drug history is also very important. However, our case had no significant drug history.
Kounis syndrome is less frequently recognized clinically and reported in scientific literature, probably due to missed, undiagnosed, and/or unrecognized patients.13
It has three variants, type I seen in patients having normal coronary arteries without predisposing factors for coronary artery disease, type II in patients with preexisting atheromatous disease, and type III in patients with stent implant and thrombus adjacent to stent show eosinophils and/or mast cells on histologic examination.16
The management of Kounis syndrome can be challenging as both cardiac and allergic symptoms need simultaneous treatment, and drugs given for allergic symptoms can aggravate the cardiac condition and vice versa.13 Type I variant patients can be treated for allergic symptoms with intravenous hydrocortisone and antihistamines. Type II variant patients can be managed with acute coronary event protocol, along with corticosteroids and antihistamines, while type III variant patients can be managed with acute coronary event protocol, and immediate aspiration of stent thrombus followed by histopathological examination. Allergic symptoms in type III variants following stent implantation can be managed with corticosteroids, antihistamines, and mast cell stabilizers. Vasodilators such as nitrates and calcium blockers may be used in type I and II variants.12, 13
4 CONCLUSION
This case features a rare presentation of acute coronary syndrome following multiple wasp stings. The study highlights that whenever a patient presents with features of acute coronary syndrome and allergic symptoms simultaneously, Kounis syndrome should be suspected. Since it is a rare cause of the acute coronary syndrome, awareness of this entity leads to early diagnosis and management of the case.
AUTHOR CONTRIBUTIONS
Angela Basnet: Conceptualization; data curation; supervision; validation; writing – original draft; writing – review and editing. Manoj Khadka: Conceptualization; validation; writing – original draft; writing – review and editing. Abdullah Alismail: Supervision; validation; writing – original draft; writing – review and editing. Dhan Bahadur Shrestha: Supervision; validation; writing – original draft; writing – review and editing. Ashok Thapa: Data curation; validation; writing – original draft; writing – review and editing.
ACKNOWLEDGMENT
None.
FUNDING INFORMATION
The authors declare that they have no known competing financial interests.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
INFORMED CONSENT
Written informed consent was taken from the patient's party for the publication of the case and images.
Open Research
DATA AVAILABILITY STATEMENT
None.