The Ayurvedic Management of Fungal Sinusitis in Standalone Settings: A Case Report
Funding: The authors received no specific funding for this work.
ABSTRACT
A 42-year-old female with left nasal blockage, facial numbness, upper palate pain, and headache was diagnosed with fungal ball sinusitis via CT scan. Refusing surgery, she opted for Ayurveda. Comprehensive treatment led to complete symptom resolution and a clear CT scan at 3 months.
1 Introduction
Fungal sinusitis is inflammation of the mucosal lining of the paranasal sinuses caused by fungal infection [1]. It is differentiated into invasive and noninvasive fungal infections, with the former invading epithelial cells and the latter usually limited to superficial epithelial cells [2]. Immunocompromised and immunosuppressed individuals are vulnerable to fungal sinusitis [3, 4]. Fungal sinusitis can also be classified into four types: acute (invasive), chronic (invasive), fungal ball, and allergic fungal sinusitis. The pathological, immunological, and clinical features also vary among these subtypes. Antibiotic consumption, corticosteroid therapy, and diabetes mellitus are major predisposing factors for the development of fungal sinusitis [5-7]. Fungal balls are usually noninvasive and might become invasive if a patient is immunocompromised. The identification of this condition relies primarily on clinical symptoms, endoscopic findings, imaging studies, examination for pathogenic microorganisms, and histopathological analysis. Surgical debridement, antifungal agents, and systemic factor treatment are regarded as therapeutic strategies [8-10]. However, these treatment modalities face significant challenges. Data have established that significant disease relapse occurs even after surgical intervention [11, 12]. In certain cases, patients lose their vision even after aggressive surgical debridement [13]. There is an inconsistency of evidence supporting antifungal therapy for different subtypes of fungal sinusitis, and the risk of antifungal sinusitis outweighs the benefit in the management of chronic rhinosinusitis [14]. Current challenges in the treatment and understanding of fungal sinusitis demand the development of potential novel strategies [15-19]. In this regard, we present a case report of fungal sinusitis successfully managed with standalone Ayurveda treatment [20-22].
2 Case Report
2.1 Patient History of Illness
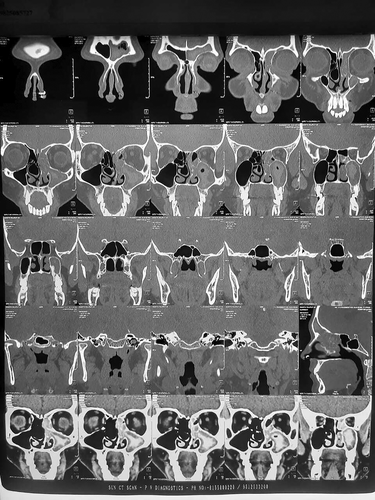
A 42-year-old female patient complained of nasal blockage on the left side, left-sided facial numbness, pain on the left side of the upper palate, and left-sided headache for 10–12 days. She consulted an ENT doctor for her concerns, where she was advised to receive a CT scan. Figure 1 shows that the PNS CT revealed Opacification of the left frontal-ethmoid-maxillary sinuses, suggesting sinusitis. Hyperdense contents within opacified sinuses suggest fungal hyphae. The findings were suggestive of noninvasive Aspergillus infection. Fungal debris accumulation and associated calcification within Sinus cavity are visible in this CT image as hyperdense areas, indicating chronic noninvasive fungal sinusitis; which leads to diagnosis of chronic noninvasive fungal ball sinusitis (Deutsch, Whittaker, and Prasad) [23].
The ENT doctor suggested FESS surgery. The patient was hesitant to undergo surgery, and since she was informed about successful fungal sinusitis cases managed by the first author through Ayurveda, she decided to approach the first author for Ayurveda treatment. Hence, she visited Agnivesh Ayurveda Hospital, Surat, for an Ayurvedic consultation.
2.2 Ayurvedic Assessment
After interviewing, case taking, and examining the patient, it was found that the patient was habituated to Kapha (Kapha, doṣha responsible for cohesiveness—ITA-2.1.3.1) prakopaka (Aggravation of kapha—ITA-5.2.3.3) food and lifestyle, which also contributed to mandagni (Depressed or weak state of digestive, metabolic factors—ITA-2.6.11) and excess Kleda (moistness/soddening—SAT-D.2534) in the body, directly becoming the nidana (factors directly or indirectly implicated in the etiology of a disease—ITA-4.4.1) for this condition.
According to the Ayurvedic assessment of the disease, nasal blockage was confirmed to be sroto-avarodha due to Kahpha prakopa, facial numbness and headache due to vata and kapha prakopa, and pain in the palate due to vata prakopa. Krumjia shiroroga (headache due to kṛmi/worm infestation—ITA—5.67.7) was diagnosed, and treatment was given on the basis of the principles of krumjia shiro roga (headache due to kṛmi/worm infestation—ITA—5.67.7), kaphaja (worm or parasite arising from vitiated kapha—ITA—5.13.5), and rataja krumi (worm formed in blood and affecting blood vessels—ITA—5.13.7) lodged in the nose and dushivisha (cumulative poisoning with mild effects over time—ITA—5.72.13).
2.3 Treatment and Diet
The treatment approach was focused on reducing kleda, clearing srotas, destroying Krimi, and normalizing the movement of vata. The patient was prescribed Brihat vata chintamani rasa 1 tablet twice daily for 3 months, Krumikuthara rasa 2 tablet thrice daily for 3 months, Krumighna vatika 2 tablet thrice daily for 1 month, Serenkottai nei capsule 1 capsule thrice daily intranasally for 2 months, Rasa Gandhi mezhugu 1 capsule twice daily for 1 month, Netra sudarshan eye drops in each eye thrice daily for 3 months, Vyadhi haran rasa 5 g given over a month, Karbogi tablet 2 tablets thrice daily for 1 month, Vidang choorna consumed along with regular food and water for 3 months, a mixture of Palash choorna 400 g Bhallatak choorna 50 g and Vilwadi gulika 100 tab powder burnt and given as dhuma nasya (intranasal therapy with medicated smoke-ITA-9.2.93) twice daily for 3 months, and Boniheal tablet once in the morning for 2 months. Patients were asked to follow up after 7 days (Table 1).
| S no. | Medicine name | Particulars | Dose | Duration |
|---|---|---|---|---|
| 1 | Brihat vat chintamani rasa | Herbo mineral formulation containing purified, Rasa (Purified Mercury), Gandhaka (Purified Sulfur), Abhraka Bhasma (Calcinated Mica) {Ref: Rasa Tarangini} | 1 tab twice a day | 2 months 18 days (78 days) |
| 2 | Krumikuthar rasa | Herbo mineral Formulation containing Kajjali (Black Sulfide of Mercury), Tankana Bhasma (Borax) {Ref: Bhaishajya Ratnavali} | 2 tab thrice a day | 2 months 18 days (78 days) |
| 3 | Krumighna vatika | Herbal Formulation containing Vidanga (Embelia ribes) Ajamoda (Trachyspermum ammi) Haritaki (Terminalia chebula) {Ref: Bhaishajya Ratnavali} | 2 tab thrice a day | 1 month (30 days) |
| 4 | Serenkottai nei capsule | Herbal combination containing Shuddha Bhallataka (Semecarpus anacardium), Milk, Ghee {Ref: Siddha Vaithya Thirattu} | 1 capsule thrice a day and a nasal drop (Half capsule has to be instilled in both nostrils) | 1 month 19 days (49 days) |
| 5 | Rasa Gandhi mezugu | Herbo Mineral Formulation containing Rasa (Purified Mercury) Gandhakam (Purified Sulfur) {Ref: Siddha Pharmacopoeia of India} | 1 cap twice a day | 1 month (30 days) |
| 6 | Netra sudarshan eye drops | Herbal combination containing Triphala (Emblica officinalis, Terminalia chebula, Terminalia bellirica) {Ref: Bhava Prakash} | 2 drops in each eye thrice a day | 2 months 18 days (78 days) |
| 7 | Vyadhi haran rasa | Herbo mineral Formulation containing Rasa (Purified Mercury), Swarnamakshika Bhasma (Calx of Chalcopyrite) {Ref: Rasa Tarangini} | 5 g in 30 days | 1 month (30 days) |
| 8 | Karbogi tablet | Herbal formulation containing Chitraka (Plumbago zeylanica), Hing (Ferula asafoetida), Ajwain (Trachyspermum ammi) {Ref- Siddha Pharmacopeia} | 2 tablets twice a day | 1 month (30 days) |
| 9 | Vidang choorna | Herbal Powder contains Vidanga (Embelia ribes), Amla (Indian Gooseberry) {Ref:Bhava Prakash} | Patient has to consume food mixed with vidang choorna | 2 months 18 days (78 days) |
| 10 | Palash choorna 400 g + Bhallatak choorna 50 g + Vilwadi gulika 100 tablets | Herbal Formulations contains powder of Palash (Butea monosperma), Bhallathaka (Semecarpus anacardium), Vilwa (Aegle marmelos) {Ref: Sahasrayoga, Bhava Prakash} | Mix all the formulations together and patient has to inhale and exhale the smoke generated from it morning and in evening | 2 months 18 days (78 days) |
| 11 | Boniheal tablet | Herbo Mineral Formulation contains Ashwagandha (Withania somnifera), Guduchi (Tinospora cordifolia), Godanti Bhasma(Gypsum) {Ref-Ayurveda Proprietary Medicine} | 1 tablet in morning | 1 month 19 days (49 days) |
The patient was advised to consume garlic, red rice, raw banana, pointed gourd, neem, bitter gourd, betel leaf, honey, camel milk, and carom seeds as a part of her diet and was instructed to consume food only when she was hungry and drank water, which was boiled and reduced to half, only when she was thirsty. She was asked to refrain from sleeping during the day, drinking water immediately after work or exercise, suppressing natural urges and exposure to cold wind, and avoiding the use of milk and dairy products, jaggery, ghee, fruit and fruit juices, black grams, green leafy vegetables, sweet and sour food, raw vegetables, fermented food, sugary drinks, and food made of refined wheat flour.
2.4 Follow-Up
On the 7th day of treatment, her nasal blockage completely resolved. She was asked to continue the medicines and to follow up again 7 days later. By the second follow-up on the 14th day of treatment, her facial numbness, headache, and pain in the upper palate had gradually decreased. At her third follow-up 15 days later, her facial numbness, headache, and pain in the upper palate were further reduced. During the fourth follow-up 20 days later, her symptoms were relieved almost completely, and she was advised to receive CT-PNS at her next visit.
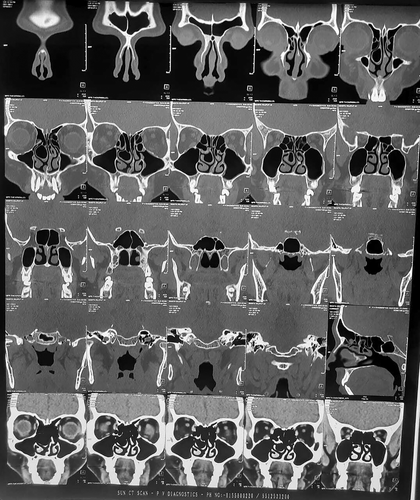
Figure 2 shows that CT revealed complete resolution of the pathology and no residual inflammation in the sinuses. The medicines were continued for another month, and after 3 months of treatment, the patient was free from all symptoms and showed no symptoms of relapse or any other concerns.
3 Discussion
Noninvasive fungal sinusitis can be categorized as fungal ball, saprophytic fungal sinusitis, or allergic rhinosinusitis. Fungal balls are considered thick accumulations of fungal hyphae without invasion. Computed tomography (CT) is regarded as the gold standard tool for the functional diagnosis of fungal balls. In this report, CT revealed the presence of hyperdense fungal hyphae with left frontal-ethmoid-maxillary sinuses. The noninvasive nature of fungal hyphae is determined by the absence of bony sinus wall erosions and the absence of intracranial or intraorbital extension in CT images. Fungal balls usually appear in unilateral sinuses, and fungal balls affecting multiple sinuses are rare. In this case, we observed that the fungal balls affected the left frontal-ethmoid-maxillary sinuses. Females are estimated to have a greater chance of being diagnosed with fungal balls. In this case, the patient was a 42-year-old female whose age group also fell under the high chance of becoming infected with fungal balls.
Earlier studies have demonstrated that nasal obstruction, rhinorrhea, postnasal drip, nasal bleeding, headache, and facial pain are the major clinical symptoms associated with fungal balls. In this case, the clinical symptoms observed are consistent with those of previous studies, as the patient had major symptoms, such as nasal obstruction on the left side, left-sided facial numbness, pain on the upper palate of the left side, and headache on the left side. In this case, though in CT image osteitis is not directly visible, it is important to consider the fungal debris and associated calcification which are visible in CT as hyperdense areas in sinus which evidently indicate toward chronic noninvasive fungal sinusitis. It is important to observe from scientific evidence that osteitis need not be mandatory to diagnose chronic noninvasive fungal sinusitis. The hyperdense fungal accumulation present in CT is also considered as the evidence for diagnosing chronic noninvasive fungal ball sinusitis (Broglie, Tinguely, and Holzman) [24]. Along with available scientific evidence, the expert observation by radiologist who has significant expertise and experience in the field and is also an author, also diagnosed the same as chronic noninvasive fungal ball. It is to be noted that expert clinical judgment too is one of the components of “Evidence based medicine.”
The fungal ball was predominantly observed in immunocompetent individuals; in this case, the patient assessment revealed the immunocompetence status of the patient. The treatment strategy for Fb is based on symptoms, and the standard treatment guideline indicated for Fb is functional endoscopic sinus surgery (FESS) if symptoms are present. In this case, the patient was suggested for FESS surgery considering the distress caused by the symptoms. Qualitative research analyzing patients' perceptions of endoscopic sinus surgery (ESS) revealed that there were significant levels of concern with patients regarding ESS before surgery. In this case, the concerns regarding FESS and patient awareness about previous successful fungal sinusitis cases treated by the First Author through Ayurveda could have led the patient to approach for an Ayurveda consultation.
FESS surgery is minimally invasive, and earlier studies have established that it is a safe and effective intervention for Fb patients. The complete clearance of fungus from the sinus through FESS requires clear visualization of the sinus. Even with angled endoscopy, sufficient visualization of the sinus is challenging. FESS intervention requires significant skill and expertise and the use of appropriate methods to achieve safe and effective clearance of fungi. The National Sino-Nasal Audit revealed adverse effects following ESS (6.6%), predominantly minor bleeding and major complications (0.4%). There is specific identification of adverse effects associated with the ophthalmic system. The adverse effects range from minor complications such as periorbital ecchymosis and orbital emphysema to major complications such as extraocular muscle injury, persistent diplopia, orbital hemorrhage, or hematoma.
In this context, the FESS is important for assessing the utility of the Ayurvedic medicinal intervention presented in this case. In this case, stand-alone Ayurveda medicine and ayurveda dietary guidelines reversed the symptoms within 20 days, and clearance from fungal balls was observed in CT images at 2 months. Recently, Aksakal [25] reported three cases in which ESS was performed for the management of fungal balls. It was observed that it took 26 weeks, 7, and 6 months for those patients to achieve relief or reversal of symptoms after ESS surgery. Alromaih et al. [26] reported a case series of four patients diagnosed with FB who were only managed with steroids and topical decongestant medications. At least 6 months are needed for patients to achieve significant symptom relief. Thus, in our case report, Ayurvedic interventions resulted in much faster symptom reversal and greater FB clearance in CT images than did ESS and medical therapy, as reported in earlier publications. The medical therapy for FBs mainly includes steroids, topical decongestants, and antibiotics. There are warnings of small but important side effects associated with systemic steroid use, and side effects such as gastric ulcers, osteoporosis, and immune suppression are observed. It is also important to reduce the use of antibiotics in the midst of increasing concerns over antibiotic resistance. In this case, the patient's follow-up revealed no side effects from the Ayurvedic intervention. Apart from effectiveness and safety, it is also important to assess the cost effectiveness of an intervention and its impact on the overall quality of life of patients. On enquiry with NABH accredited/Franchise hospitals, the rate for FESS ranges between Rs. 50,000 and Rs. 60,000. The expense is exclusive to other hospital costs and medicine costs, which can be a burden to the patient compared with Rs. 10,000–12,000, who use ayurvedic interventions. Noon and Hopkins [27] reported an unexpected trend in which a significant number of patients were delayed from undergoing surgery in the UK even after 5 years of chronic rhino sinusitis diagnosis. This is reflected in the attempt of the NHS UK to reduce costs. The median length of hospital stay after surgical intervention for Fb-affected patients according to the assessment of Garofalo et al. [28] was 3 days. It is important to analyze the loss of production days, and the overall burden can be added to a patient's quality of life. The Ayurvedic interventions documented in this case report may have advantages in this context, as they can be cost-effective and do not demand hospitalization compared with the ESS intervention.
4 Material Constituents Present in the Drugs Used
The various drugs used for clinical interventions include the following constituents: gold, silver, iron oxide, calcium oxide sulfur, mercury sulfide, mercury, sulfur, mercurous chloride, arsenic trisulfide, ferrosoferric oxide, copper sulfate, zinc carbonate, zinc sulfate, lead monoxide, arsenic trioxide, arsenic pentasulfide, arsenic trisulfide, arsenic disulfide, silver nitrate, mercuric chloride, mercuric sulfide, mercurous chloride, calcium sulfate, magnesium sulfate, calcium oxide, biogenic silica, zinc, arsenic, lead, cadmium, silver, aluminum, boron, barium, chromium, copper, iron, manganese, nickel, sodium, phosphor, potassium, magnesium, sodium, antimony, rubidium, strontium, iron, copper, silicon, and sodium borate. The patient was followed up, and no adverse drug reactions were reported. There was a drastic improvement in the clinical condition of the patient. The chemical constituents present in these drugs may contain therapeutic derivatives or nanomolecular structures of the source material, and these multifunctional nanostructures facilitate desirable biological processes as a result of their unique and peculiar structure–property relationships. Metal nanoparticles, including silver, copper, iron, and zinc, can act as sources of reactive oxygen species, and these reactive oxygen species can deactivate fungi and bacteria through various interaction mechanisms, such as lipid peroxidation pathway activation and membrane rupture through surface oxidation [29].
Metal nanoparticles and organic complex molecules present in phytochemicals can inhibit inflammation. Multiple multifunctional constituents, such as carboxylic acids, polyols, esters, aliphatics, and biopolymers, are present in plant-based aqueous drug formulations and have antifungal, antibacterial, and anti-inflammatory properties [29-31]. Recent reports also suggest that the phytochemicals present in classical ayurvedic drug sources, such as picrorhiza kurroa, emblica officinalis, and tinospora cordifolia, which contain 3,5,9-trioxa-4-phosphaheneicosan-1-aminium,4-hydroxy-N,N,N-trimethyl-10-oxo-7-([1oxododecyl]oxy)-, hydroxide, innersalt, 4-oxide, (R)-, 3-(octanoyloxy) propane-1,2-diyl bis(decanoate), succinic acid, 2-methylhex-3-yl 2,2,2-trifluoroethyl ester, and neophytadiene, have antioxidant properties with specific abilities to inhibit the COX-2 and NOX-2 pathways [30]. Additionally, 3-(octanoyloxy) propane-1,2-diyl bis(decanoate), succinic acid, 2-methylhex-3-yl 2,2,2-trifluoroethyl ester, neophytadiene, 3,5,9-trioxa-4-phosphaheneicosan-1-aminium, 4-hydroxy-N,N,N-trimethyl-10-oxo-7-([1-oxododecyl]oxy)-, hydroxide, inner salt, 4-oxide, (R)-. Neophytadiene can act as a good anti-inflammatory agent [32]. Moreover, the effectiveness of fumigation intervention may be due to the effect of molecules present in the soot [33]. The soot generated from fumigation of ayurvedic drugs may contain large carbon-based nanostructures with antifungal and antibacterial properties. Further advanced physicochemical and biochar characterization studies must be conducted to explore and understand the empirical evidence in this regard.
The patient's lived experience with disease and treatment noted “When we first learned of my condition as fungal sinusitis, we were extremely stressed due to the alarming news about the disease in Surat. Unsure about surgery, a friend recommended Ayurvedic treatment. We consulted for Ayurveda treatment, and now, my condition is completely fine.” The patient's lived experience may be indicative of distress of being diagnosed with an alarming disease and whole improvement with Ayurveda treatment as full relief. This case report also has limitations, as no quality-of-life assessment with the SNOT-22 was performed to evaluate comprehensive QOL before and after Ayurveda treatment. In this case, the patient's lived experience and cost comparison for FESS-conventional treatment and Ayurveda treatment were considered. Thus, it would be important to use QOL assessments such as the SNOT-22 in these clinical conditions for structured and comprehensive QOL assessments of treatment in case reports.
5 Conclusions
The standalone Ayurveda treatment for fungal ball sinusitis in this case was effective and safe. The significant cost-effectiveness of Ayurveda treatment in this context becomes an additional important benefit. This case report highlights the importance of Ayurveda treatment for fungal sinusitis, which should be further assessed with rigorous research designs.
Author Contributions
Rajanikant Patel: conceptualization, data curation, formal analysis, writing – original draft, writing – review and editing. Lakshmanan Skanthesh: conceptualization, data curation, formal analysis, writing – original draft, writing – review and editing. Vishal Zaveri: conceptualization, formal analysis, writing – original draft, writing – review and editing. Vinayak Padikkal: conceptualization, formal analysis, writing – original draft, writing – review and editing. Oriparambil Sivaraman Nirmal Ghosh: conceptualization, formal analysis, writing – original draft, writing – review and editing.
Acknowledgments
We express our gratitude to the patients' family members for their cooperation.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The datasets generated or analyzed during this study are available from the corresponding author upon reasonable request.




