Subacute brainstem ischemic syndrome in juvenile neurofibromatosis type 2: An underrecognized condition
Abstract
We report the case of a teenager with a neurofibromatosis Type 2 (NF2) presenting a locked-in syndrome due to a brainstem ischemic syndrome. The presence of sudden or rapidly worsening onset of neurological deficits in NF2 patients, should evoke this underknown entity and not only tumors as predisposed by NF2.
1 INTRODUCTION
Neurofibromatosis Type 2 (NF2) is an autosomal-dominant tumor-prone disorder characterized by the development of distinctive nervous system tumors, including meningiomas, ependymomas and peripheral, spinal, and cranial nerve schwannomas, in addition to skin anomalies and visual symptoms. Bilateral vestibular schwannomas are pathognomonic. So, the most common entry in the disease is through hearing impairment, which usually occurs in the second decade of life. But, unlike adults, children most frequently present with ocular, dermatological, and neurological symptoms. Brainstem ischemic syndrome, which is an under-recognized entity of unknown origin, occurs in teenagers without any previously known NF2 diagnosis, presenting as an acute or subacute event, which involves the midbrain or pons.
2 CASE HISTORY
A 15-year-old girl was transferred from a primary care institution for headache, acute left hemiparesis, and left paresthesia. Her history revealed left hypoacusis, left voice cord palsy, and left unreactive mydriasis of unknown origin for over a 3-year period. The admission brain CT scanner had shown heterogeneous parenchymal damage within the right side of the pons (not shown). Three years earlier, the girl underwent brain magnetic resonance imaging (MRI), which was described as normal.
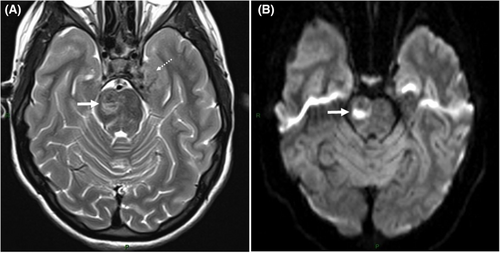
The brain MRI at admission showed a heterogeneous T2/FLAIR hypersignal on the right thalami, cerebral peduncle, midbrain, and pons, displaying marked restriction of free water diffusivity featuring cytotoxic edema on diffusion-weighted (DW) views. A few pontine subareas disclosed low signal intensity on both T2 and diffusion weightings suggesting foci of hemorrhagic transformation (Figure 1). Other multiple lesions already detectable on the MRI performed 3 years earlier, were present as bilateral vestibular schwannomas, left trigeminal schwannoma, together with a meningioma at the cranial vertex and a cervical cord ependymoma, strongly suggesting a type 2 neurofibromatosis (NF2).
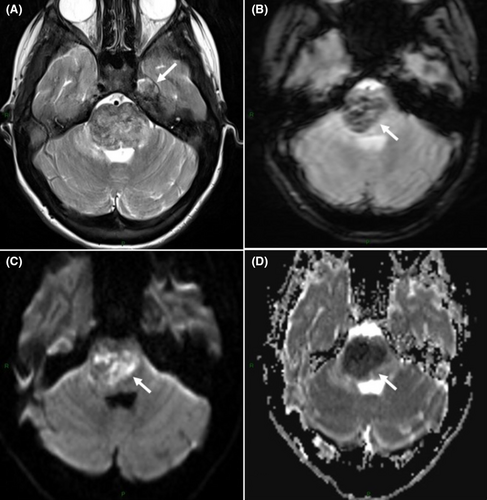
On Day 14, the left hemiparesis worsened, and the girl exhibited swallowing difficulties and bilateral facial palsy. The MRI, carried out on Day 18, revealed a progression of the right-sided pontine lesion with persistent mosaicism of acute ischemic lesions with high T2/FLAIR signal intensity with lowered apparent diffusion coefficient (ADC) and strongly hypointense areas with susceptibility artifacts on gradient-echo T2-weighted views featuring hemorrhagic transformation (Figure 2).
From Day 20 onward, the girl progressively developed a spastic quadriplegia with pyramidal signs and a vesical globe; owing to her bilateral facial palsy, she was not longer able to speak, whereas her cognitive function was preserved. The diagnosis of a locked-in syndrome was retained.
We reviewed the diagnostic differential of brainstem lesions (Table 1) and faced with this progressive lesion, a tumor was suspected, and corticosteroids were initiated. But stereotactic biopsy was not contributive with pathological changes evocating necrosis.
| Stroke | Tumor | Infection | Inflammation | Metabolic | Toxic | |
|---|---|---|---|---|---|---|
| Etiology |
Basilar artery occlusion (due to cardioembolism, trauma, hypercoagulable disorders, unknown) Vertebral artery dissection (±after neck traumatism) Brainstem ischemic syndrome in NF2 Unknown |
Diffuse high-grade glioma (±75%) Focal low-grade glioma Exophytic glioma (low grade) Langherans cell histiocytosis Epidermoid/dermoid tumor |
Listeria, Enterovirus, HSV |
ADEM Multiple sclerosis ANE (after influenza A, B, parainfluenza, HHV6) Bickerstaff encephalitis (ganglioside GQ1b antibodies, after Campylobacter jejuni or Mycoplasma pneumoniae) |
Mitochondrial disease | Central pontine myelinolysis |
|
Specific symptoms In addition of headaches, cranial nerve palsy, motor deficit |
– | Ataxia |
Fever Encephalopathy Seizures Ataxia |
±after a viral infection Encephalopathy Seizures Bickerstaff: Ophtalmoplegia, ataxia, coma, areflexia |
±decompensation after a viral infection Multisystemic symptoms, ataxia, dystonia, regression |
severe alteration of plasma osmolality or hyponatremia Encephalopathy Confusion |
|
Brain MRI And other tests |
T2 and flair hypersignal pons > medulla reduction in diffusion |
T2 hypersignal High grade glioma: mass effect, oedema, infiltration, absent or inhomogeneous contrast enhancement Low grade glioma focal, less oedema Exophytic glioma from the 4th ventricle, as low grade glioma Langherans cell histiocytosis With hypothalamic–pituitary lesions (Epi)dermoid tumor Focal, no oedema, reduction in diffusion |
T2 hypersignal multiple lesions, patchy, asymmetric, ±abscess, ±supra-tentorial lesions CSF WBC ↑, protein normal or ↑, glucose: normal or ↓ Culture and PCR |
T2 hypersignal with supra tentorial lesions in white matter (except Bickerstaff: only brainstem) CSF WBC ↑, protein ↑, normal glucose, ±oligoclonal bands, ganglioside GQ1b antibodies + in Bickerstaff |
T2 hypersignal Gray matter: substantia nigra, medullary and pontine tegmentum, basal ganglia and diffuse supra -tentorial leukoencephalopathy Blood test: lactate ↑, alanine ↑, urine organic acid: abnormal CSF §: protein normal or ↑, lactate ↑ Molecular analysis |
T2 hypersignal Central pontine myelinolysis central pons, ±trident shape ± midbrain and middle cerebellar peduncles Blood test: Osmolality alteration |
| Treatment | Anticoagulation or Aspirin ± thrombolysis | According histology | Antimicrobial treatment | Corticoids | Vitamins and supportive therapy |
Prevention Supportive therapy |
| Outcome | good except if size >50% or coma at presentation | According histology | Poor outcome in 50% | According etiology | Poor | Variable |
- Abbreviations: ADEM, Acute disseminated encephalopathy; ANE, acute necrotizing encephalopathy; CSF, cerebrospinal fluid.
Then, by reviewing the girl's full medical record, the diagnosis of brainstem ischemic syndrome was proposed, reflecting an uncommon medical condition associated with NF2. Brain magnetic resonance angiography (MRA), cardiac-carotid and vertebral ultrasonography, and hemostasis evaluation were unremarkable. Aspirin treatment was initiated, and she was transferred to a rehabilitation center. Three months later, she was able to carry out head movements which helped her communicate, as well as some arm movements.
The NF2 diagnosis had meanwhile been confirmed by revealing an heterozygous pathogenic variant on NF2 gene, c.1376dup (p.Glu460GlyfsTer35).
3 DISCUSSION
The locked-in syndrome is a neurological disorder that is characterized by quadriplegia and anarthria with preserved cognitive functioning. Patients usually retain eye movements, thereby facilitating non-verbal communication. This clinical diagnosis may prove challenging, given that the children are often considered as being in coma or in an unresponsiveness state, or as displaying akinetic mutism. A normal electroencephalogram (EEG) should alert the physician.1 This condition is mostly caused by a brainstem lesion; in 61% of cases, the etiology in children is ventral pontine stroke due to a vertebrobasilar artery thrombosis.1 The syndrome's prognosis depends on the underlying cause. Around 35% of patients experienced some motor recovery, 26% exhibited good recovery, 23% died, and 16% remained quadriplegic and anarthric.1 Motor recovery is earlier and superior in locked-in syndrome non-vascular cases. Intensive rehabilitative care has been shown to improve motor outcome.1
As illustrated by our case, differential diagnosis of brainstem lesions can be challenging. We reviewed the brainstem disorders in pediatric patients in an effort to guide the clinician in this difficult yet essential differential diagnosis. Usually, brainstem lesions tend to become quickly symptomatic. A small and single lesion can produce severe and mixed deficits related to the large number of essential structures localized within this area including cranial nerves nuclei, the reticular formation, ascending, descending, and cerebellar pathways. Brain MRI is generally carried out early in the diagnostic approach. The resulting findings can help clinicians in regard to differential diagnosis.
Among the causes of brainstem pathologies in children, vascular, toxic, metabolic, infectious, inflammatory, or neoplasia processes appear to play a role, as previously reported. As degenerative diseases are rather rare in this specific area, they will not be discussed here. The clinical presentation of brainstem lesions is roughly uniform with multiple cranial nerve palsy, motor deficiencies, and headaches, whereas the clinical context, brain MRI features, and laboratory testing results may be quite useful in further directing the clinicians (Table 1).2
In our case, the diagnosis was difficult, given that the lesion progression let us to suspect the presence of a tumor, within the NF2 setting.
NF2 is an autosomal dominant disorder, caused by a variant inactivating the NF2 gene encoding the protein merlin whose main function is to regulate cellular proliferation.3 Its loss of function is associated with several neurological tumors including peripheral, spinal and cranial nerve schwannomas, meningiomas, as well as ependymomas, in addition to skin anomalies such as NF2 skin plaques, subcutaneous and cutaneous schwannomas, along with visual symptoms, including cataracts, retinal hamartomas, or optic nerve sheath meningiomas. Bilateral vestibular schwannomas in children, adolescents, and young adults are pathognomonic of the condition. The most common entry in the disease is through unilateral or bilateral hearing impairment, which usually occurs in the second decade of life. The presence of sudden or rapidly worsening onset of neurological deficits in NF2 patients should evoke a brainstem ischemic syndrome, which is an under-recognized entity.4 This syndrome occurs in teenagers without any previously known NF2 diagnosis, presenting as an acute, usually monophasic event, which involves the midbrain or pons. A gradual evolution, as seen in our case, is similarly possible.4 In clinical terms, patients start to suffer from cranial nerve palsy, dysarthria, hemiparesis, or a locked-in syndrome. The brain MRA, cardiac echocardiogram, and thrombophilia screen usually prove to be non-contributive. Several cases have been described exhibiting vascular stenosis, which cannot explain the stroke in anatomical terms. So far, the etiology remains unclear. According to one of the hypotheses, the tumor suppressor protein merlin possibly plays a role in regulating physiological angiogenesis, whereas its inactivation may induce vascular dysplasia that could induce an ischemic event.5 Genetically, any distinct variant in NF2 has been associated with brainstem ischemia. Another hypothesis raises the possibility of a digenic process, given that this syndrome is relatively rare in NF2 patients.4 Concerning treatment, aspirin can be employed, which is the case in ischemic events. The prognosis is variable. While some patients have fully recovered after 6 months, others did exhibit some motor recovery, and still others remained in a locked-in syndrome.4, 6 The evolution likely depends on both the ischemia extension and the quality of rehabilitative care.
4 CONCLUSION
Brainstem ischemic syndrome is a rare and under-recognized entity of unknown origin, occurring in teenagers without any previously known NF2 diagnosis. The adolescents suffer from cranial nerve palsy, dysarthria, hemiparesis, or a locked-in syndrome. The clinical context and MRI provide the diagnosis. So, it is essential to consider this syndrome in NF2 patients and not only tumors as predisposed by NF2. Aspirin can be employed. The prognosis is variable ranging from full remission to persistent locked-in syndrome.
AUTHOR CONTRIBUTIONS
AB contributed to the collection of the case information, reviewing the literature, designing, and writing the manuscript. CL contributed to the interpretation of brain MRI and was involved in drafting the manuscript. TD contributed to the interpretation of brain MRI, revised the manuscript critically for important intellectual content and reshaped it. MCN contributed to the collection of the case information, reviewed the literature, established the diagnosis, revised the manuscript critically for important intellectual content and reshaped it. All authors read and approved the final version of the manuscript.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
CONSENT
Written informed consent was obtained from the patient's parents to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.