Rectus sheath hematoma secondary to acute exacerbation of COPD: A case report
Funding information
This article did not receive any grants.
Abstract
Rectus sheath hematoma, a rare condition, develops due to rupture of epigastric arteries or the rectus abdominis muscle. This case report conveys that such condition can occur due to violent coughing spells, and this should not be missed when a patient with chronic obstructive pulmonary disease presents with abdominal pain.
1 INTRODUCTION
Rectus sheath hematoma (RSH), accumulation of blood in the sheath of rectus abdominis, is a rarely occurring condition. It may be due to rupture of epigastric arteries or the muscle within the rectus sheath.1, 2 Significant risk factors of rectus sheath hematoma include female gender, older age, anticoagulant therapy, antiplatelet therapy, abdominal injections, violent cough, and abdominal trauma.3 Rectus sheath hematoma is usually seen to develop in the lower quadrants of the abdominal wall, and it rarely crosses the midline.4 It follows a benign course, but severe outcomes, including mortality, have also been reported.2
In this case report, we report a case where rectus sheath hematoma develops in a patient diagnosed with chronic obstructive pulmonary disease (COPD) due to increased intra-abdominal pressure resulting from chronic coughing. There is a lack of literature and data regarding the development of rectus sheath hematoma secondary to acute exacerbation of COPD, but case reports have been published in this regard. This case report aims to add to it.
This case report is in line with CARE guidelines.5
2 CASE REPORT
A 58-year-old male, with a past medical history of chronic obstructive pulmonary disease (COPD), a resident of a remote village of Nepal, presented to the emergency department of Karnali Academy of Health Sciences (KAHS) with the issues of increased shortness of breath, cough since 7 days and lower abdominal pain since 2 days back. He had started experiencing shortness of breath even at rest, and his coughs were more violent than before, disturbing his sleep and daily activities. The cough had acute onset, and its sputum was yellowish-whitish in color. Lower abdominal pain had started acutely 2 days back (from the day of presentation), and it was severe enough to affect his daily activities. The patient also reported having swollen lower limbs, fever on and off, and non-radiating epigastric pain for a week. However, history of trauma, changes in bowel and bladder habits, burning micturition, retention of urine, paroxysmal nocturnal dyspnea, orthopnea, palpitation, and chest pain were negative.
Thorough history taking revealed that the patient was diagnosed with COPD 8 years back, for which he is under medication. He gave up smoking cigarettes after the diagnosis of COPD and is on complete abstinence at present. There is no other significant medical and drug history. There is no family history for any chronic illnesses, but there is a practice of using wood fuel for heat at his home during the winter season.
2.1 Timeline
The patient presented to our emergency department on November 16, 2021, with clinical features of acute exacerbation of COPD. Later, he was diagnosed to have rectus sheath hematoma. It was first treated conservatively but the patient had to be operated on due to its failure. The patient recovered well and was discharged on December 24, 2021 Figure 1.

2.2 Diagnostic assessments
On the day of presentation, the patient had a body temperature of 98 degrees Fahrenheit, a heart rate of 97 beats per minute, a respiratory rate of 26 per minute, a blood pressure of 110/70 mm of Hg, and an oxygen saturation of 74%. On examination, the patient was ill-looking with a bruise over his periumbilical region (5 cm × 3 cm) and bilateral pitting edema on the lower limbs. Chest examination revealed a barrel-shaped chest and the use of accessory muscles during respiration. Wheeze was heard on the left side and crackles on the right side on auscultation. Abdominal examination showed swelling below the umbilicus, which was tender, slightly hot on palpation, and dull on percussion. There were no visible dilated veins or peristalsis. Carnett's sign and Fothergill's sign were positive. All the hematological tests and biochemical investigations were normal.
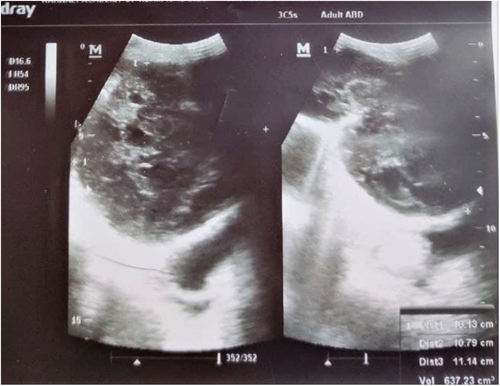
Ultrasonography (USG) showed multiple calcified hepatic granulomas in the right lobe of the liver, slightly echogenic kidneys with intact corticomedullary differentiation, irregular thick-walled collection in the pelvic cavity (10 cm3), which had lace-like multiple septations along with multiple echogenic echoes, mild prostatomegaly, bilateral pleural effusion, and minimal ascites.
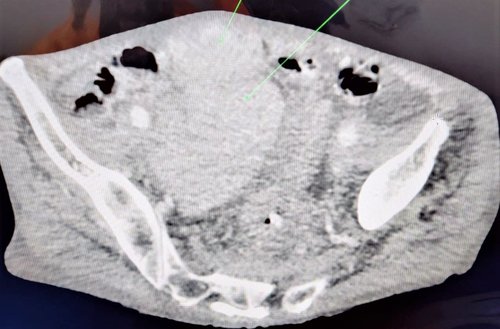
The patient was admitted, and treatment was initiated for acute exacerbation of COPD. USG had to be repeated as the patient's abdominal swelling, and tenderness did not resolve. An intramuscular hematoma extending deep into the abdominal cavity was observed this time. The patient was hemodynamically stable up to this point in time; so, the patient was kept under conservative management by giving a cough suppressant. After 5 days, tenderness and swelling increased, hemoglobin level dropped to 12.9 gm/dl, red blood cells count was 4.4 million per cubic millimeter, and platelets count was 104,000. USG at this stage showed a large intramuscular hematoma of 673.23 cm3 with an echogenic line and debris in the abdominal wall extending deep into the abdominal cavity. Computed tomography confirmed this. Considering these developments and the lack of angiography with an arterial embolization facility, the patient was then planned for surgical intervention.
2.3 Treatment
As soon as the patient was diagnosed of having an acute exacerbation of COPD, he was treated with furosemide 20 mg IV, hydrocortisone 200 mg IV, ceftriaxone 1g IV, azithromycin (500 mg PO stat), nebulization (3 times, six-hourly) with asthalin: ipratropium bromide: normal saline (1:1:2), pantoprazole 40 mg at the emergency department.
The patient was admitted to the medical ward and was put on a combination of amoxicillin and clavulanic acid (625 mg, three times a day) for 10 days and azithromycin (500 mg, once a day) for 7 days. During his stay in the medical ward, he was also given furosemide (40 mg, once a day) 10 days, prednisolone (40 mg, once a day) for 5 days, hyoscine bromide (20 mg, three times a day) for 10 days, fexofenadine (180 mg) for 10 days, codeine (15 mg, three times a day for 10 days), and ranitidine (150 mg, twice a day) for 14 days.
Laparotomy was performed when conservative management failed. Surgery was done through an infra-umbilical incision. Exploration showed stretched and dusky appearing rectus muscle with rectus diastasis, and transverse abdominis muscle was necrosed and lysed. A clot of approximately 1 liter was removed from the pre-peritoneal region on the right side. The bleeding vessel could not be identified, possibly due to thrombosis.
The patient was monitored for 1 week and discharged as all of his symptoms had resolved. The patient was counseled about the condition, the need for oxygen supplementation, and the risk of inhaling smoke coming from burning wood fuel. The patient was discharged with a prescription of oxygen supplementation (2–3 L, for 15–18 h a day) at home, tamsulosin (0.4 mg, once a day) for 30 days, finasteride (5 mg, once a day) for 30 days, and a combination of salmeterol and fluticasone (250 mcg, two times a day) as an inhalant for 30 days.
2.4 Follow-up
The patient and his family were properly counseled regarding his condition, his need for oxygen supplementation, and the risk of burning wood fuel. The patient is asked to come for follow-up after 10 days and is informed to come as soon as possible if he develops new symptoms.
3 DISCUSSION
In this case report, we have reported a case of a 58-year-old gentleman who developed rectus sheath hematoma secondary to acute exacerbation of COPD due to the associated violent cough spells. Cough-induced abdominal wall hematoma is rare, and hematoma can occur in other abdominal wall muscles.2, 3 Rectus sheath hematoma develops due to rupture of one of the epigastric arteries or tear of the rectus abdominis muscle itself. Injury can be caused either by direct abdominal trauma or violent, forceful contraction of the rectus abdominis. The inferior epigastric artery is usually involved, and rectus sheath hematoma is usually seen in the lower abdomen.6
The incidence of rectus sheath hematoma increases with age and is more common in females than males. This is believed to be due to decreased muscle mass. In addition, several risk factors such as atherosclerosis, hypertension atherosclerosis, vasculitis, hematologic disorders, direct trauma to the abdomen, surgical intervention, anticoagulation therapy, coughing/intense rectus abdominis muscle contraction, and pregnancy have been identified predispose patients to develop rectus sheath hematoma.6 Rectus sheath hematoma is generally seen as a self-limiting condition, but it can prove to be fatal, and mortality can rise from 4% to 25% in patients under anticoagulation therapy.6, 7 However, our patient was not under anticoagulation therapy. Commonly patients with rectus sheath hematoma present with abdominal pain, abdominal cramping, abdominal wall mass, abdominal wall ecchymosis, abdominal distention, decreased hemoglobin, fever, nausea, vomiting, tachycardia, and peritoneal irritation.3 Fothergill's and Carnett's are positive in the case of rectus sheath hematoma, which differentiates this condition from intraabdominal pathologies. Fothergill's sign is positive when the hematoma does not cross the midline, and Carnett's sign is positive when there is increased pain and tenderness over the hematoma on rectus abdominis contraction. Moreover, externally visible ecchymosis may be seen over the abdomen causing Grey Turner's sign and Cullen's sign.4 Our patient's signs were present (Figure 2), but he had no ecchymosis over his flanks.

To confirm the case, we made use of ultrasound and computed tomography (Figures 3 and 4). Ultrasound has a high sensitivity rate and is commonly used as it is time and cost-effective. Computed tomography is considered more sensitive; so, it is used in doubtful and inconclusive ultrasound cases. Magnetic resonance imaging is another less commonly used measure for confirming the diagnosis.8 Patients who are hemodynamically stable and have non-expanding hematomas can be treated conservatively. Conservative treatment includes rest, analgesia, cough suppression, compression of hematoma, ice treatment, intravenous fluid maintenance, and stopping the anticoagulation therapy (if needed). Invasive intervention is needed if the patient becomes hemodynamically unstable if hematoma enlarges or signs of abdominal compartment syndrome.6 Angiography and embolization or surgical ligation of bleeding vessels are treatment choices due to the lack of angiography and arterial embolization in our facility. (Figures 5 and 6).


Presentation of rectal sheath hematoma can mask other conditions such as appendicitis and pancreatitis. Thorough history taking and diagnostic assessments are crucial for diagnosing this condition. Moreover, rectus sheath hematoma can occur in patients having no history of abdominal trauma, strain, or anticoagulant therapy. Rectus sheath hematoma should always be looked for in patients with a COPD history presenting with abdominal pain.
4 CONCLUSION
Rectal sheath hematoma should be in the mind of the health professionals when a patient having a history of chronic obstructive pulmonary disease presents with abdominal pain. Thorough history taking, diagnostic tests, and ultrasonography are essential for the early diagnosis of the condition. This saves the patient from invasive diagnostic procedures and decreases morbidity and mortality.
ACKNOWLEDGEMENTS
We would like to acknowledge Dr. Suryaman Menyangbo, Dr. Abijit Mishra, Dr. Yagya Rokaya, and Dr. Rajesh Niraula for the role they have played during this study.
CONFLICT OF INTEREST
No conflict of interests.
AUTHOR CONTRIBUTIONS
Prashant Pant (PP) and Oshan Shrestha (OS) contributed to the conception and design of the study. PP, Nebula Devkota (ND), and Pawan Budhathoki (PB) contributed to acquiring patients’ detailed information. OS performed the literature review and contributed to initial manuscript drafting. Sanjit Adhikari (SA) and Dhan Bahadur Shrestha (DBS) guided throughout the study and edited intellectually. All authors were involved in drafting and revising the manuscript and approved the final version.
CONSENT
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
PATIENT PERSPECTIVE
The patient was surprised to know that his cough spells caused hematoma in his abdominal wall. He is intrigued by the anatomy and complexity of the human body. The patient and his family understand the risk of exacerbation of COPD and are willing to follow all that they are counselled about.
Open Research
DATA AVAILABILITY STATEMENT
All the findings are present within the manuscript.