Ileocolic intussusception due to intestinal lipoma in an adult patient
Abstract
Intestinal obstruction due to intussusception caused by intestinal lipomas is a rare condition in adults that needs urgent treatment. CT (Computerised Tomography) is the radiologic modality of choice for diagnosis. Surgery is the treatment of choice and has excellent outcome.
1 INTRODUCTION
Intussusception is a rare cause of intestinal obstruction in adults, accounting for <5% cases. The clinical presentation in adults is vague and nonspecific, thereby complicating differential diagnosis. A 27-year-old woman presented to our emergency department with complaints of diffuse pain abdomen, nausea, and vomiting for the past 3 days. Abdominal X-ray showed features of bowel obstruction, and computed tomography demonstrated ileocolic intussusception due to a probable submucosal lipoma. The patient underwent emergency laparotomy and right hemicolectomy. The resected specimen on examination showed multiple pedunculated lipomas acting as lead point causing a 15 cm long ileocolic intussusception. Histopathological examination of the specimen confirmed submucosal lipomas. Intestinal obstruction due to intussusception caused by lipomas is a very rare condition that needs urgent treatment. CT (Computerised Tomography) is the radiologic modality of choice for diagnosis. Surgery is the treatment of choice and has an excellent outcome. Choice of procedure depends on involved segment and viability of the affected bowel. Open or laparoscopic technique can be considered based on patient's condition and surgical expertise available.
Intussusception is telescoping of a proximal segment of the bowel, called the intussusceptum, into the distal portion, called the intussuscepiens. Intussusception usually affects children, and is an uncommon condition in adults, accounting for 5% of all cases.1, 2 Over 90% cases have an identifiable cause, though malignant tumors account for most of them.2 A review of literature shows 50 cases of bowel intussusception due to lipomas reported in the first decade of the millennium, with around 21 being solitary ileal lipomas.3 Multiple ileal lipomas presenting as ileocolic intussusception are a rare clinical entity, with only a couple of reported cases.3
Lipomas are benign, slow growing tumors of mesenchymal cells, occurring anywhere in the body. Lipomas in small bowel account for only 20%-25% of the cases of all gastrointestinal lipomas.4 These are usually solitary lesions with multiple lipomas seen in <5% cases.5
Here, we present an unusual case of ileocolic intussusception due to multiple lipomas in the terminal ileum, leading to intestinal obstruction.
2 CASE HISTORY
A 27-year-old woman presented to accident and emergency unit of our hospital with complaints of diffuse pain abdomen, nausea, and vomiting for the past 3 days. The pain was colicky in nature, mild to moderate intensity and started in right lower abdomen, gradually becoming generalized and associated with abdominal distension. There was associated bilious vomiting and unable to tolerate any oral intake over the past 24 hours. She initially had loose stools, but was not opening bowels and passing flatus for the past 2 days. Pt had history of cesarian section in the past.
On examination, patient was tachycardic, tachypneic, hypotensive and afebrile. Her abdomen was distended with generalized tenderness and diffuse guarding. The bowel sounds were exaggerated with borborygmi. Rectal examination was empty with ballooning.
2.1 Differential diagnosis
Clinical diagnosis of intestinal obstruction due to adhesions/band was made. Differential diagnoses included ileocecal tuberculosis, appendicular lump, colitis, and inflammatory bowel disease.
2.2 Investigations and treatment
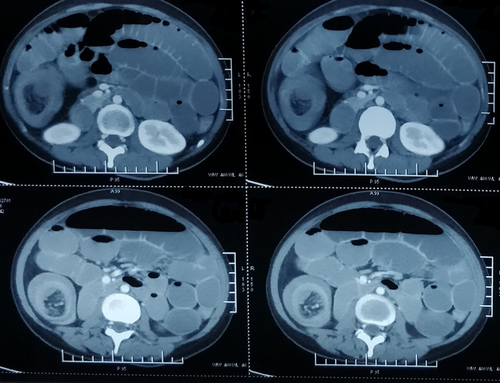
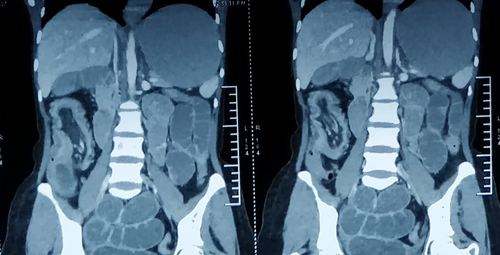
Biochemical and hematological investigations were unremarkable except for raised white cell count of 16 × 109/L with neutrophils 89.3%, and raised CRP of 286 mg/L. Serum lactate levels were 2.4 mmol/L. Plain abdominal X-ray showed dilated small bowel loops with multiple air-fluid levels and collapsed large bowel. Chest X-ray did not reveal pneumoperitoneum. After initial resuscitation, urgent CT abdomen and pelvis was performed (Figures 1 and 2). This showed a prominent “target sign” in the right lower abdomen which was suggestive of long segment ileocolic intussusception. A well-defined, predominantly fatty lesion with enhancing septations was seen inseparable from the invaginated loop, suggestive of intestinal lipoma serving as the lead point. This was associated with upstream dilatation of entire small bowel and stomach, with collapsed bowel distal to hepatic flexure, suggestive of intestinal obstruction.
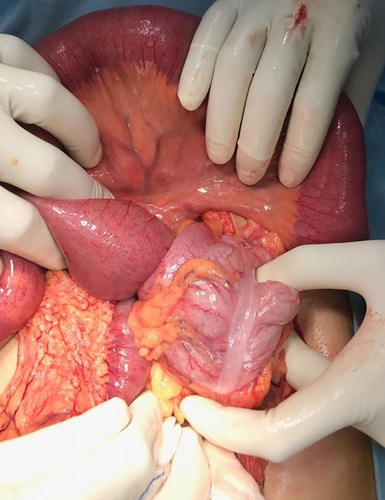
Pt. was taken for urgent exploratory laparotomy under general anesthesia after stabilization. As reported on CT, a long segment (15 cm) of ileocolic intussusception was seen in the right lower abdomen (Figure 3). The proximal small bowel was grossly distended, dusky, and edematous with poor peristalsis, suggestive of early ischemic changes. There was a moderate amount of inflammatory fluid present in the abdomen. Considering the dubious nature of bowel, length of intussuscepted bowel and high risk of perforation, decision was taken to proceed with right hemicolectomy and end-to-side isoperistaltic ileocolic anastomosis. The resected specimen on examination showed multiple pedunculated lipomas (Figure 4).

2.3 Outcome and follow up
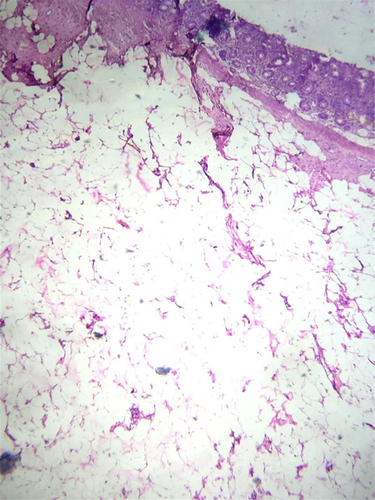
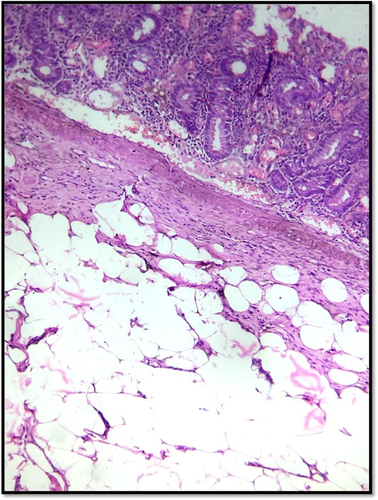
The patient had an uneventful recovery postoperatively. Histopathology showed submucosal lipomas in terminal ileum as a cause of ileocolic intussusception (Figures 5 and 6). There was no evidence of dysplasia or malignancy.
3 DISCUSSION
Classification of intussusceptions is based on location. The commonly used classification divides intussusception into four categories: ileoileal, ileocolic, ileocecal, and colocolic.6 The Ileocolic variant is defined as prolapse of the terminal ileum through the ileocecal valve into the colon. They account for 15% of all intussusceptions. The causative lesion is usually in the ileum.7 However, in 8%-20% no identifiable cause can be found.1, 6
Intussusception is commonly a disease affecting young children up to 4 years, with ileocolic being the most common variant. Adult intussusception accounts for only 5%-10% of all reported cases.8 The classical triad of abdominal pain, palpable mass, and bleeding per rectum (red currant jelly stools) is rarely seen in adults, leading to frequent misdiagnosis. Another point of significance is that an identifiable lesion, usually a malignant tumor, is present in most cases.2 This necessitates surgical intervention.
Lipomas of the bowel are usually submucosal, pedunculated lesions, and occasionally being subserosal. As per Cancer Research UK, small bowel cancer affects about 1600 people in the UK each year, and <2% of these are benign tumors like polyps and lipomas.9 Although usually asymptomatic, they can cause bleeding, obstruction, or intussusception.10
The radiologic modalities available for the diagnosis of intussusception include plain abdominal X-ray, ultrasonography, and CT scan. Abdominal X-ray is the first diagnostic tool used in the A&E, and it indicates the site of possible small bowel obstruction. Abdominal ultrasound can detect intussusception as a “target sign,” “pseudo kidney sign,” or “crescent in a doughnut sign”. However, it is operator dependent and findings may be obscured by bowel gas in obstruction cases.11 CT scan is the most commonly used investigative modality for acute abdomen. For intussusception, diagnostic accuracy of CT ranges from 60% to 100%.6, 12 The findings are usually diagnostic, with a typical appearance of bowel-within-bowel configuration with or without contained fat and mesenteric vessels. This appears as a “target” or a “doughnut” mass in images vertical to the longitudinal axis of the lesion or as a “sausage-shaped” mass parallel to its longitudinal axis.13
Diagnosis of intestinal lipomas can be made by a variety of modalities. Non-invasive methods include barium studies and most importantly CT scan. Endoscopic visualization is possible by conventional, balloon, or capsule endoscopy. Typical CT appearance is a smooth, well-demarcated sausage-shaped mass. An advantage of CT is that any associated intussusception is also revealed, and vascularity of the bowel can be assessed.14 Other methods to confirm associated intussusception are contrast enema showing a “crescent sign” and MRI abdomen.15 Endoscopic appearance is of a smooth, yellowish surface with pedunculated, or sessile base. Other characteristics signs on endoscopy include “cushion sign” – the tumor indents on pressure application by biopsy forceps, and “naked fat sign” – multiple biopsies cause protrusion of yellowish fat.16, 17
Surgery is the recommended management in adults due to the presence of a causative lesion in a large number of cases and the relatively high risk of malignancy.18 However, the procedure to be adopted is controversial.6, 8 It has been argued that small bowel lesions are less likely to be malignant. Hence, if a preoperative diagnosis of a benign lesion is made, or en bloc resection has the possibility of causing short gut syndrome, reduction of the intussusception can be considered provided the bowel is non-ischemic.2, 8, 19 This has to be balanced against the risk of rupture of edematous bowel, risk of anastomotic leak due to manipulation of friable bowel, or seeding due to peritoneal rupture. Hence in older patients with colon involvement, formal oncologic resection with anastomosis between healthy, viable bowel is recommended.2, 8, 19-21 For left-sided colon, Azar et al 6 recommend colostomy or Hartmann's procedure with anastomosis as a second stage surgery. Laparoscopic approach is a valuable diagnostic and therapeutic tool, with a number of reports being published.22 The procedure followed is the same as for open techniques. Success rates dependent on patient selection and surgeon's expertise.
4 CONCLUSIONS
Intestinal intussusception in adults, though rare, is a challenging condition for the surgeon as it usually presents as an acute abdomen. It is usually not considered in preoperative differential diagnosis as the signs and symptoms are vague and nonspecific, without the classical triad seen in children. Abdominal CT is the diagnostic modality of choice in intussusception, and distinguishes the presence or absence of a lead point. Surgical intervention is indicated in adults on diagnosis of bowel intussusception due to the frequent presence of a malignant etiology. Reduction is only indicated if a benign pathology is confirmed, short gut syndrome would be caused by the resection, and the affected bowel is non-ischemic and viable. Otherwise, treatment usually requires formal resection of the involved bowel segment.
ACKNOWLEDGEMENT
The authors wish to acknowledge the contribution of the staff of Safdarjung Hospital, New Delhi, and in particular the departments of General Surgery, Radiology and Pathology without whose help and support this report would not have been possible. Published with written consent of the patient.
CONFLICT OF INTEREST
The authors whose names are listed above certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial in the subject matter or materials discussed in this manuscript.
AUTHOR CONTRIBUTION
AS: is the operating surgeon and lead author in this case. He helped provide the clinical information and images. He also helped to write the article, with prominent contributions in the abstract, introduction and actual case report. AT: is the corresponding author and co-author for the article. He played a major part in the abstract, introduction, discussion, referencing, and formatting.
ETHICAL APPROVAL
Ethical approval was taken from the hospital ethics committee. All patient details have been anonymized to protect their identity.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analysed in this study.