Implant assisted ortho-surgery in edentulous jaws: a clinical report
Key Clinical Message
The severely atrophy of jaws often complicates ideally oral reconstruction of esthetics and functionality, and necessitates different preprosthetic surgeries including bone grafting, ortho-surgery, and implant insertion. The mentioned procedures could be done within different approaches. This report describes the management of an edentulous case by implant insertion before orthognathic correction.
Introduction
Successful rehabilitation of patients with severely atrophied jaws who demand implant therapy is a challenging procedure 1 due to insufficient bone for implant insertion, a reversed intermaxillary relationship 2 and an increased inter-arch space 3. Although the sinus bone grafting is a reliable reconstructive technique which provides adequate bone volume 4, 5 in maxillary posterior area, sagital, and vertical discrepancies in such cases are more than what could be solved with sinus lifting or simple bone grafting. Therefore, for correcting extreme deficiencies, ortho-surgery along with bone grafting is recommended 6-9. In these complex cases, the treatment plan includes several surgical interventions including orthognathic surgery, bone grafting, and implant insertion, which could be done in a variant number of steps and sequences 2, 10, 11.
One approach which has shown good results is Le Fort I osteotomy combined with interpositional grafts 12, 13. It could be followed by delayed 14 or immediate 2 implant insertion. However, the skeletal relapse is considered the most common complication after orthosurgery 15, 16. As any adaptive changes in the orofacial complex may lead to relapse 17, the occlusion stability is important to prevent it; but unfortunately we usually encounter edentulous patients whose dentures lack retention and occlusal stability. This article reports a modified approach for step by step rehabilitation of an edentulous case that has experienced two unsuccessful ortho-surgical jaw corrections.
Case Report
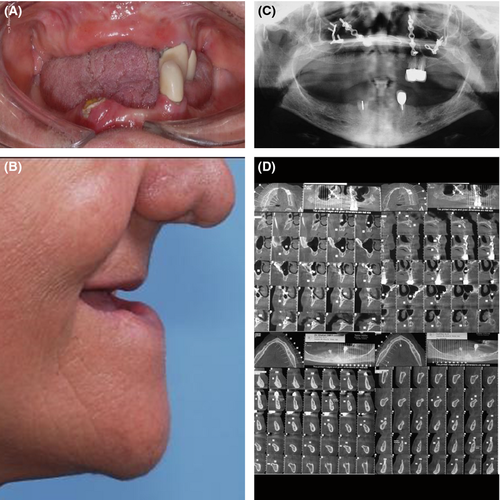
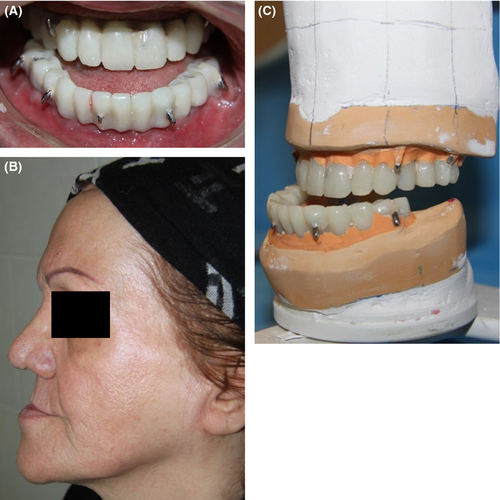
In 2012 a 64-year-old female patient referred to the clinic claiming for esthetic and functional oral rehabilitation. No remarkable finding was identified in her medical history. She expressed extreme dissatisfaction with her profile and her loose-fitting prosthesis; and she wanted to have a fixed prosthesis. The patient stated that she had been subjected to reconstructive surgery twice in order to improve her profile but both procedures resulted in relapse. The first had been done during trauma management after a car accident she had, and the second ortho-surgical correction was 18 months later. Clinical and radiographic examination revealed that only left maxillary premolars and both mandibular canines were present in the oral cavity (Fig. 1A). Excessive maxillary and mandibular resorption had resulted in an increased interarch space. In addition, midfacial soft tissue collapse due to the maxillary retrusion and a class III jaw relationship were detected (Fig. 1B). In panoramic view, bilateral pneumatized sinus cavities and the plates and screws of the previous surgeries were evident (Fig. 1C). In the CT views, the residual bone height (RBH) was 12 mm at the former position of the maxillary central and lateral incisors, 8 mm of the second premolar, and 7 mm of the first molar (Fig. 1D).
After the whole procedure was explained to the patient; she signed a written informed consent form. The procedure began with extracting all the four remaining teeth. Primary impressions of maxillary and mandibular arches were made using irreversible hydrocolloid impression material (Alginate; Zhermack, SpA, Padua, Italy); then record bases and wax rims were fabricated on the casts according to normal landmarks, and were arbitrarily mounted on a semi-adjustable articulator (Stratos 300, Ivoclar Vivadent, Liechtenstein). Mounting was done without making any intraoral records. In other words, they were hand articulated based on a normal imaginary maxilla-mandibular relationship. Setting up the denture teeth was accomplished on the residual ridge, and clear dentures as surgical guides for implant insertion were processed. As there was no need to increase height of the bone, they were also used as surgical guides for bone grafting.
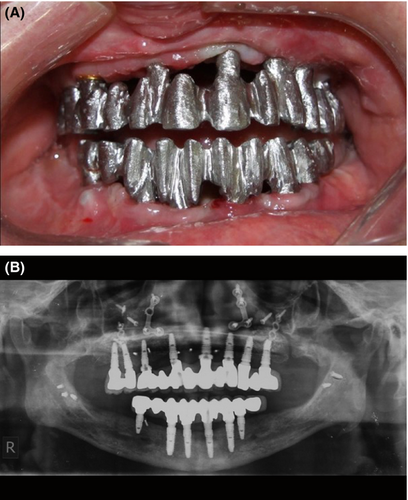
In one session, implant insertion and bone grafting were carried out simultaneously. As height of bone in the anterior region of maxilla was adequate, it is was only augmented in width; and the posterior region was sinus lifted. In the mandibular view there was enough bone for inserting implants. Fourteen implants (Implantium, Dentium, Seoul, South Korea), eight in the maxilla (sites 1.2, 1.4, 1.5, 1.6, 2.1, 2.3, 2.4, and 2.5) and six in the mandible (sites 3.1, 3.3, 3.4, 4.2, 4.3, and 4.5) were inserted (Fig. 2A). The implant insertion torque value applied was not less than 20N cm for all implants.
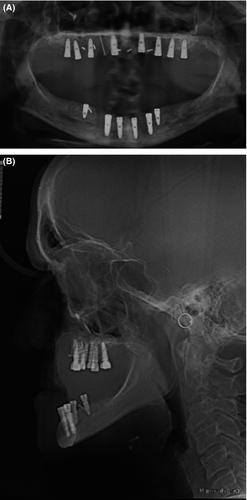
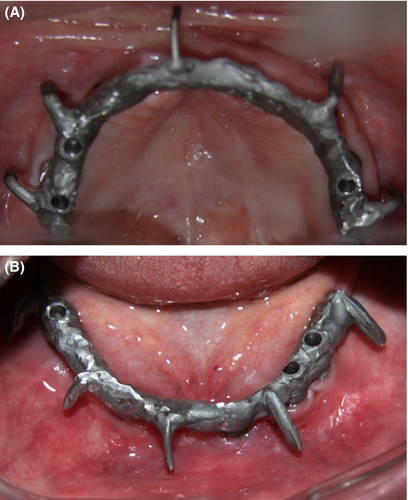
Obviously, because of the extreme intermaxillary relationship (Fig. 2B), the patient could not have a good prosthesis with these implants; especially a fixed one. After a healing period of 4 months, six implants in mandible and five implants in maxilla were uncovered and implant level impressions with a regular-viscosity polyether (Impregum, Espe Dental, Seefeld, Germany) in a custom impression tray were made. Once again record bases were fabricated; and the casts were hand articulated the same as before. Castable abutments (Implantium, Dentium, Seoul, South Korea) were selected, and maxillary and mandibular frameworks for supporting provisional restorations were made and tried in the mouth to check passive fitness. Each framework had five hooks in the buccal side which were considered to use elastics after orthognathic surgery (Fig. 3A and B). The metal-acrylic provisional restorations were finalized and were checked in the mouth (Fig. 4A and B). As expected, they could not have occlusion in mouth; because they were fabricated on an arbitrarily mounted relation. An interocclusal record with an addition silicone-based occlusal registration material (Futar D fast; Kettenbach, Eschenburg, Germany) and a facebow record were taken. Pick up impressions with polyvinyl siloxane impression material (Panasil, Kettenbach, Eschenburg, Germany) were made, and study casts for the model surgery were prepared (Fig. 4C).
By preoperative evaluations, the surgeon determined 8 mm maxillary advancement and 6 mm mandibular setback required to be done. As a bimaxillary surgery was considered, an intermediate splint 18 was made with self cure acrylic resin (Meliodent Cold, HerausKulzer, Ltd., Newbury, UK). Model surgery was performed; and exactly a day before surgery, the provisional restorations were delivered to the patient. Therefore, during surgery, the surgeon was able to use the intercuspation of prosthesis in order to reorient maxilla and mandible (Fig. 5).

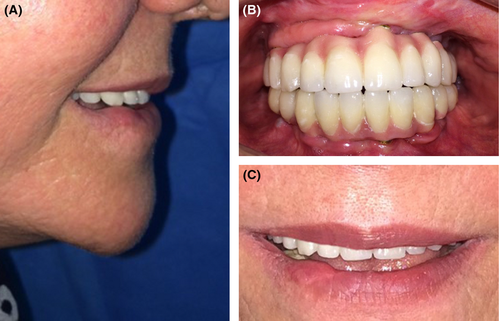
Five months later, remaining implants were uncovered. Definitive implant level impressions were made; after setting up the teeth, a silicone index was used to aid in abutment selection. After try in of the frameworks (Fig. 6A and B), final prosthesis were delivered (Fig. 7A–C).
Discussion
To achieve a satisfactory result in treating a case of severely atrophied jaws, particular problems including lack of bone volume to insert implants 2 and compromised facial esthetics in both antero-posterior and vertical dimensions are encountered 3. According to the available literature, different approaches have been proposed to address these problems and each differ in the number of steps and in the sequence of the steps 2, 10, 11. Some investigators 2, 19-21 reported a one step procedure in which orthognathic surgery, bone grafting, and implant placement were all simultaneously done. Based on the case, the one step procedure would be a combination of Le Fort I osteotomy and implant placement without any bone grafting 22. The one step procedure still poses risk of graft and implant loss 2, 23 which should be weighed against its advantage of short time of rehabilitation 20. Some others 10, 24 described a two-step procedure including Le Fort I osteotomy combined with grafting of the floor of the sinus and nose at first step, and implant placement at further step. This method leads to a decreased probability of bone graft necrosis and implant loss. In addition; precise position and inclination of implants using a drill guide based on CT scans is possible. Gil et al. 11 suggested a three-step procedure including maxillary bone reconstruction, implant insertion and a fixed prosthetic rehabilitation in the existing class III occlusion; followed by orthognathic surgery. Beside the mentioned advantage of implant placement in a separate step, due to its special sequence, this method takes advantage of using implant supported fixed prosthesis during ortho-surgery. A desirable esthetic outcome is related to the accurate repositioning of the maxilla with the aid of fixed prosthesis; which is hard to achieve with a removable one 11.
Orthognathic surgical procedures first developed to correct the intermaxillary relationship in dentate patients 25. However; prosthesis assisted ortho-surgery allows fully edentulous 18, partially edentulous 26 and some dentate patients like the ones who suffer from Amelogenesis Imperfecta 27 to take advantage of orthognathic surgery benefits. In this article, the authors emphasize the importance of Implant assisted ortho-surgery in severely atrophied edentulous cases who could not receive a stable denture. In this way, by implant insertion before orthognathic correction we can not only treat the patient with implant supported prosthesis but also we can ensure the intra- and postsurgical occlusal stability and the final result as well. Moreover, patients could have normal function and esthetic faster after surgery. In this method, considering hooks in the framework of provisional restorations eliminated the need of using orthodontic appliances to allow intermaxillary fixation; which made it distinct from the method introduced by Gil et al. 11. However, to assess long-term success rate of implants followed by ortho-surgery and the possibility of relapse, longer follow-up on a larger group of cases is required.
Conflict of Interest
None declared.