Presentation and resolution of gender dysphoria as a positive symptom in a young schizophrenic man who presented with self-emasculation: Frontiers of bioethics, psychiatry, and microsurgical genital reconstruction
Correspondence
Darius A. Paduch, Arthur Smith Institute for Urology, Northwell Health, 1000 Northern Boulevard, Suite 120, Great neck, NY 11021, USA.
Email: [email protected]
Abstract
Gender dysphoria can present as a positive symptom of schizophrenia. Completion of gender affirmation surgeries should not occur as a result of male genital self-mutilation via a deferral of emergent surgical reconstruction. Instead, gender affirmation should be considered after a full workup and assessment for resolution of any acute psychosis.
1 INTRODUCTION
Male genital mutilations and modifications (MGMM) have been documented since antiquity and are still practiced globally.1 In our practice, we classify MGMM as circumcision, amputation of the glans penis, amputation of the penile shaft (ie, penectomy), castration (ie, orchiectomy), removal of the skin of the scrotum (ie, scrotectomy), complete emasculation (ie, removal of the scrotal skin, penis, and testes), and other (eg. penile and scrotal piercing, subdermal foreign bodies, incisions of the urethra). Anthropologically, MGMM are often described as a rite of passage from boyhood to adulthood (eg, circumcision in adolescent boys in Africa), or as a sign of belonging to specific group (eg, Hijra and Skoptsy), and are either performed willingly or by the will of the parents/tribe.2 In this paper, we will focus self-performed MGMM as they present a multidisciplinary challenge.
Penile amputation is most commonly due to accidental trauma, but it can also be a result of assault, iatrogenic causes such as during circumcision, or rarely as a form of self-mutilation for religious reasons.3, 4 Due to the low incidence of traumatic penile amputation (TPA), most of our knowledge is derived from case reports with the largest series reported in Thailand during a string of domestic violence toward unfaithful husbands.5 When not occurring for religious reasons, penile amputation is a surgical emergency requiring reattachment of the phallus with water tight urethroplasty to allow for voiding while standing and preservation of penile tissue for penetrative sexual intercourse.6
Self-penile amputation and other forms of genital self-mutilation (GSM) performed outside of religious reasons typically happen in the setting of mental illness, and in the third decade of life, more specifically, they often occur during an initial psychotic state or when a patient is not taking their medications.4, 7, 8 For example, simultaneous self-amputation and self-castration is most often performed in the setting of schizophrenia.4
GSM may be result of gender dysphoria in a patient unable to afford or qualify for gender affirmation surgery.9 In the case of schizophrenia, convictions about belonging to the opposite sex may coexist with olfactory as well as sensory hallucinations within the genitals and are experienced by up to 20% of men with untreated schizophrenia. The patient experiences this as a sense of sexual abuse and believes that removing his own genitalia will relieve the unpleasant sensory input.10 It is critical to make an appropriate decision before taking patient to the operating theater as the wrong surgical decision may have catastrophic consequences for the patient.
When presented with GSM in the emergent setting in a patient with an acute psychosis, one must parse out the true underlying psychiatric disease or lack thereof. Such patients can present with gender dysphoria in conjunction with an acute psychosis or gender dysphoria as a positive sign of psychosis. As there are no established clinical pathways and consensus recommendations, such GSM presents logistic, bioethical, mental health, and legal challenges.
When presented with GSM in a conscious patient claiming to be transgender and refusing organ reattachment, the treating team has a medico-legal dilemma in assessing his mental disposition and legal competence. The patient's stated preference must be judged in the context of his psychiatric situation and consequences of refusing organ preservation.11
Unfortunately, as the male genitalia are well perfused, bleed profusely, and thus require prompt intervention for organ preservation, this generally does not leave the requisite time to evaluate for true versus psychosis-generated gender dysphoria. As a result, it is our opinion that in such cases, regardless of the patient's verbalized preference, the genitalia should be reattached as soon as possible.
In this report, we present a case of penile and testicular replantation in a patient with schizophrenia and auditory command hallucinations and gender dysphoria as a positive symptom of psychosis on presentation to the ED, which subsequently resolved completely with antipsychotics.
2 CASE REPORT
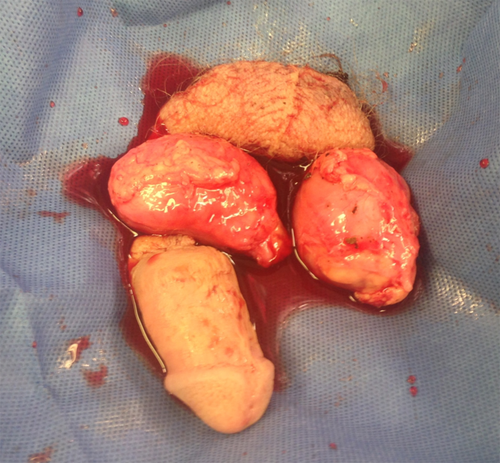
A 23-year-old male with a past medical history of Celiac disease, hypothyroidism, homelessness, and prior in-patient treatments for schizophrenia presented to our institution after having amputated his penis, testicles, and most of his scrotum with a serrated knife. This was done in a public area, 20 minutes prior to arrival after taking two ibuprofens. The penile shaft, both testes, and scrotal skin were brought on ice with the patient by the EMT (Figure 1).
Upon arrival, the massive bleeding from the penile stump/groin was controlled by applying pressure with epinephrine-socked gauze and the patient was stabilized according to trauma protocol. He denied hallucinations and suicidal ideations. He was withdrawn, had affective flattening, disorganized speech, and difficulties organizing his thoughts. He stated that he was homeless and was undergoing gender affirmation surgery but did not supply details. He did not want his penis to be re-implanted nor his family to be informed. He had dramatically diminished sensation of pain given his injury. His toxicology screen was negative. On examination, his penis was amputated at the base. He was given a third-generation cephalosporin and tetanus-diphtheria-acel pertussis vaccine. The prior psychiatric history of the patient could not be obtained at this time and was later hindered by the family's denial that he suffered from schizophrenia. The ED psychiatrist, the attending trauma surgeon, the reconstructive urologist (DAP), and the administrator-on-call all agreed that the patient was in an acute psychosis and lacked legal capacity to refuse emergent medical treatment. He was taken emergently to the operating room for microsurgical replantation. Aspirin therapy was started, and subcutaneous heparin (SQH) 5000 units TID was initiated. Prior to induction, he again stated that he was a transgender woman, refused reattachment, however, did desire for us to control the bleeding. Surgical details are described in the Appendix S1.
After the index surgery, the patient was transferred to the surgical intensive care unit for graft perfusion monitoring. To increase penile perfusion, he was started on tadalafil 5 mg daily. Of note, the patient started to experience morning erections of the proximal and partial erections of the distal shaft within 2 weeks from reconstruction.
Postoperative testosterone was 67 ng/dL, and he was started on replacement with testosterone enanthate IM 200 mg every 10 days. Given the contaminated nature of the wound, he was continued on IV antibiotics (switched to oral after 5 days and then continued for 6 days).
Given prior history of hypothyroidism, his thyroid function was evaluated; his thyroid-stimulating hormone (TSH) was >150 uIU/mL and free T4 was 0.3 ng/dL. Levothyroxine was continued and increased to an appropriate dose.
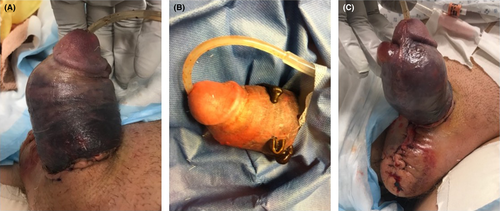
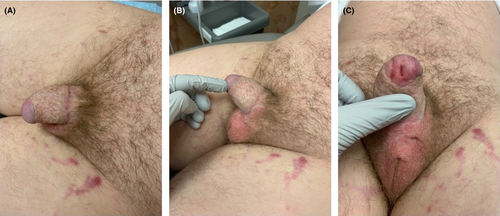
Five days after the index surgery, the patient developed classic venous skin congestion (Figure 2A) and twice-daily medical leech therapy was initiated (one placed ventrally and once dorsally and allowed to imbibe until they fell off). This initially helped reduced the ecchymosis and hematoma (Figure 2B); however, it was stopped after 1 week when skin necrosis developed (Figure 2C). The SPY Fluorescence Imaging System (Stryker) confirmed no perfusion. As the penile skin started to form an eschar, wound care consisted of twice-daily application of MediHoney gel (Derma Sciences) to eschar and Aquacel strips (ConvaTec) to exposed tissues. Daily bedside wound debridement was performed to remove necrotic skin and eschar.
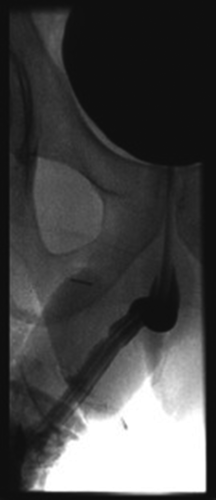
Two weeks after the index surgery, the patient underwent a retrograde urethrogram (RUG) showing no stricture nor extravasation (Figure 3); the Foley catheter was removed. He had no postvoid residual and voided without difficulty. Two weeks later, he was transferred to the psychiatric unit with continued local wound care awaiting eventual skin grafting. Prior to transfer to a psychiatric unit, the SQH and aspirin were discontinued and patient was started on pentoxifylline 400 mg TID to improve perfusion to penis.
Approximately 10 weeks after index injury, plastic surgery performed a 0.012”-split-thickness skin graft to the shaft using 110 cm2 from the lateral thigh, sutured in place with 4-0 chromic interrupted sutures. The graft healed without any complications. Once the graft was fully epithelialized, the patient started using a penile pump daily to prevent the loss of penile length.
From arrival in our ED, the psychiatry team was involved. He had been diagnosed with schizophrenia approximately 1 year prior but had not been compliant with his home antipsychotics (risperidone, later switched to paliperidone, and then long-acting injectable paliperidone). He had a family history significant for suicide by multiple paternal relatives and father with bipolar disorder. Before his self-mutilation, he had been a missing person while living undomiciled. He had a history of paranoid and persecutory delusions and suicidal ideations; there was no record of prior gender dysphoria. Daily assessment was performed by psychiatry and urology, and he was told that with improvement, he could be enrolled in a transgender program. After the index surgery, the patient initially stated that he had wanted gender affirmation surgery but had disorganized thoughts and poor understanding of his condition. Initially, he continued to endorse auditory hallucinations commanding him to amputate his genitalia; however, after the psychosis had resolved, he denied gender dysphoria. His antipsychotics were initially risperidone 1 mg twice daily and over the next 2 months up-titrating to 8 mg twice daily and then cross-tapered to clozapine 425 mg daily augmented with lithium 1200 mg daily until therapeutic levels met. He was discharged to a long-term psychiatric facility on lithium 600 mg twice daily, clozapine 150 mg q-AM and 275 mg QHS, and sertraline 150 mg q-AM.
The patient presented for follow-up at 12 months after the index surgery. He was still under psychiatric treatment. He denied being able to ejaculate; however, he was not self-stimulating and denied sexual activity. The patient did endorse tumescence although it was not yet adequate for penetration. Penile sensation was present although reduced. The skin graft was well-healed, the testis was palpable albeit atrophic, and the urethral meatus was patent (Figure 4). He was continued on testosterone replacement therapy (testosterone 339.7 ng/dL) and penile vacuum therapy. He was advised to use penile vibratory stimulation to help him reach orgasm if needed. He denied any gender dysphoria nor desire for gender affirmation surgery and identified himself as a heterosexual male.
3 DISCUSSION
GSM involving removal of the penile shaft, both testes, and entire scrotal skin is extremely rare and most reported cases have been in the setting of psychosis.4 Having first been reported by Krafft-Ebing and Freud, patients with schizophrenia and delusions or desires of changing their sex or confusion about their sexual identity remain rare; such gender dysphoria as a positive symptom of schizophrenia is estimated at around 30%.12, 13 Interestingly, in patients who present with gender dysphoria as a positive symptom of schizophrenia, it dissipates with appropriate treatment as opposed to men with gender dysphoria and schizophrenia where it persists despite appropriate antipsychotics.10 Awareness that acute gender dysphoria may be a sign of schizophrenia in patients presenting with GSM is critical for management. Only adequate control of schizophrenia, which can take months, and repeated evaluation of sexual identity over time can distinguish between “reactive” gender dysphoria or “true” gender dysphoria in a patient with mental illness. Thus, in an emergent situation, one must assume that the gender dysphoria is a positive symptom of the acute mental disorder. However, such approach is not without bioethical concerns.
Patient autonomy to make medical decisions must be respected in patients with capacity. Legal competence is an integral part of patient autonomy; it requires mental capacity to reason and deliberate, hold appropriate values and goals, appreciate one's circumstances, understand the information given, and communicate the final decision. The principal of gravity of consequences justifies the escalating threshold for capacity required for legal competence in men with GSM.11 In this case, the morbidity of following the patient's verbalized wishes (to complete the gender affirmation) would have been catastrophic, resulting in the irreversible loss of the genital function. While schizophrenia is associated with impaired decision-making, the presence of mental illness does not always render the patient incapable of making their health care decisions; the provider use tools which have been developed to obtain consent in this vulnerable group such as MacArthur Competence Assessment Tool for Clinical Research.14 This patient, however, lacked the ability to reason and appreciate consequences of his actions and therefore was unable to demonstrate that he had legal capacity. Therefore, despite his stated wish for gender affirmation surgery, the standards of transgender medicine dictate that physicians are to proceed with gender affirmation surgery only after the patient is free of psychiatric disorders such as psychosis or schizophrenia.15 After proper psychiatric management, this patient's gender dysphoria resolved and further justified the replantation of the penis and testis.
The type of GSM can help elucidate the underlying psychiatric diagnosis. In a systematic review, Veeder and Leo found that while the severity of psychosis did not correlate with the degree of self-injury, the diagnosis held by the patient did correlate with the type of injury. They found that in cases of self-amputation, 58% had schizophrenia spectrum disorders (SSDs); in cases of self-amputation and self-castration, 52.9% had SSDs. Of note, this same group found that self-castration alone was the most common form of GSM among truly transgender individuals with only 14.7% performing both castration and amputation.4 Such complexity highlights the importance of close collaboration between the psychiatric service and reconstructive surgeon both the stabilization of the acute psychosis and the long-term treatment.
Prompt microsurgical replantation of the genitalia is crucial to meeting the goal of a functional, both for voiding and sexuality, and esthetic outcome.16, 17 While most literature focusing on small case series, small meta-analyses have suggested that the best outcomes are achieved with decreased ischemia time and a microsurgical approach.18 Ischemia time should be <16 hours, replantation should focus on a watertight urethral anastomosis, and the neurovascular anastomosis should preferably be done with a microsurgical approach.16, 18, 19 In the presented case, the surgery was completed <12 hours after the injury.
In cases of successful penile replantation, complications are not rare. The case presented was complicated by testicular atrophy and venous congestion with superficial skin necrosis. Given the similarity in size between nonperfused testicular arteries and veins, and the loss of arterial flow to allow detection by microdoppler, testicular replantation remains technically difficult. This was further complicated by the location of the cut just proximal to the epididymis where the main testicular artery divides into sub-millimeter branches. However, we attempted testicular replantation based on prior successful experience with replantation after traumatic orchiectomy.
Skin venous congestion leading to necrosis occurs in over half of all penile replantations and is the most common complication.3, 6, 20 The reason for such a high complication rate lays in the high variability of venous and arterial supply to the skin; arterial blood flow is provided by the external pudendal arteries, which branch early into smaller vessels, before the penis, making arterial re-anastomosis of the skin's arterial supply difficult if not impossible.21 Medical leach therapy was attempted given the prior success reported by others to treat venous congestion after penile replantation. The primary goal was to prevent arterial thrombosis and complete distal shaft necrosis with a secondary goal of preserving the integrity of the skin.22 Medical leech therapy decreases the venous congestion of free flaps, which in turn decreases the back pressure on the arterial blood supply; to be fully successful in preserving skin integrity, venous drainage of the skin and adequate arterial supply have to be present.23 In the present case, the superficial penile veins were very small (1-2 mm) and the proximal veins could not be identified. We believe that if anatomically possible, every effort should be made to re-anastomose veins to bridge the incision and allow for adequate drainage from the skin.
One novel approach that we suggest is the use of the SPY Fluorescence Imaging System to assess, or in our case confirm, the lack of skin perfusion to help counsel the patient on the likely need of a skin graft. However, while this can give insight into perfusion of the skin, one has to be careful not to draw conclusions about cavernosal arterial blood perfusion.
Using a microsurgical technique, we avoided the commonly reported complications of a urethral stricture or fistula at the urethral anastomosis. Prior groups have reported that with a microsurgical approach, the rate of urethral stricture is decreased, likely secondary to the possibility of identifying and re-anastomosing the dorsal artery, which supplies the corpus spongiosum.17, 21 RUG in our patient confirmed this to be true and at 12-month follow up was suggested by normal uroflowmetry and residual.
This case highlights the importance of prompt action and cooperation between acute care psychiatrists, trauma surgeons, reconstructive urologists, and administration to treat patients presenting with GSM. We hope that this case, the review of relevant literature, and our own experience will prompt major trauma centers to develop a multidisciplinary approach and standard operating procedures to address these emergent cases in which wrong assumptions about the nature of gender dysphoria can have catastrophic and irreversible consequences for the rest of the patient's life.
4 CONCLUSION
Our case highlights the importance of a multidisciplinary protocol for managing patients with GSM and psychosis. Furthermore, it supports the use of a microsurgical replantation for the self-amputated penis and self-castration. The complications present are consistent with those described in the literature. We also propose the use of fluorescence imaging to evaluate for skin perfusion of the penis after replantation.
CONFLICT OF INTEREST
The authors report no competing interests.
AUTHOR CONTRIBUTIONS
RNWVB: involved in drafting of manuscript, study concept and design. CDG: involved in data acquisition, critical revision. DAP: served as senior/supervising author, involved in critical revision.