Skin lesions and neutrophilic leukemoid reaction in a patient with angioimmunoblastic T-cell lymphoma: a case report and review of the literature
Key Clinical Message
Here, we present a 53-year-old man with angioimmunoblastic T-cell lymphoma accompanied by skin lesions (vesicles, papulovesicles, and miliary papules symmetrically distributed on extremities and trunk, with more distal lesions increasing in severity). Routine blood tests showed a white blood cell count of 58.97 × 109/L (Neutrophils% 91.64%).
Introduction
Angioimmunoblastic T-cell lymphoma (AITL) is categorized as a peripheral T-cell lymphoma and is clinically characterized by a sudden onset of constitutional symptoms, lymphadenopathy, hepatosplenomegaly, immune disease (hyperactivity of the immune system and immunodeficiency) and pleural effusion, ascites, and edema 1-3. Up to approximate half of patients have skin lesions but vesicles directly caused by AITL are rare 1, 3-5. Elevated white blood cells (usually eosinophilia) are also often observed in laboratory investigations but to our knowledge, neutrophilic leukemoid reaction caused by AITL was not reported, yet 1-3, 6, 7.
Here, we present an AITL case presenting with rare skin lesions (including vesicles, papulovesicles, and miliary papules) symmetrically distributed on the extremities and trunk, with more distal lesions increasing in severity and neutrophilic leukemoid reaction.
Case Report
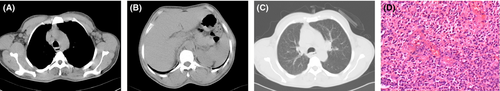
A 53-year-old Asian man was referred to our hospital for evaluation of lymphadenopathy and skin lesions. The patient's symptom history was detailed as follows: a dry cough for 3 months, lymphadenopathy for 1 month, skin lesions (started from the extremities) accompanied by pruritus for 3 weeks, dyspnea, and a mild fever for 1 week. At the time of admittance to our hospital, the patient endured severe pain of vesicles on hands and feet. Upon examination, the skin lesions were symmetrically distributed, with more distal lesions increasing in severity. Some large vesicles containing dark reddish exudate were distributed on both fingers and feet (Fig. 1A and B). Some vesicles (large and small) and papulovesicles containing clear transparent exudate were distributed on the extremities (Fig. 1A and C). Miliary papules were distributed on the upper chest and lower abdomen. Few lesions were found in the face while skin lesions were not found in the palms, soles, genitalia, scalp, around the mouth, or oral mucosa. There were palpable superficial lymph nodes in the neck, axillary fossae, and inguinas. The temperature of the skin was between 37.0 and 38.5°C during his hospitalization. The routine blood test showed a white blood cell count of 44.43 × 109/L, red blood cell count of 5.02 × 1012/L, and platelet count of 214 × 109/L. The cytological study of bone marrow showed hypergranulopoiesis. A computed tomography scan of the chest revealed lymphadenopathy in the mediastinum and axillary fossae (Fig. 2A–C). Immunochemistry of biopsy from cervical lymphadenopathy showed CD3 was diffuse strong positive, CD20 and CD8 was scattered positive, CD21 and Bcl-2 were focally positive, and Ki67 positive cells ratio was higher than 80%. Based on the cytological study of bone marrow, peripheral blood, immunochemistry and hematoxylin & eosin staining of lymphadenopathy (Fig. 2D), the pathologic diagnosis was AITL.

Both morphine and tramadol were used to control pain. After 4 days of intravenous latamoxef sodium and isepamicin treatment, the routine blood test showed a white blood cell count of 58.97 × 109/L (neutrophils% 91.64%, lymphocytes% 5.24%, monocytes% 2.44%, and eosinophils% 0.42%), red blood cell count of 4.50 × 1012/L, and platelet count of 177 × 109/L. Manifestations progressively aggravated. Then chemotherapy consisting of cyclophosphamide, epirubicin, vincristine, and prednisone (CHOP-like therapy) was administered. After chemotherapy, there was abatement of clinical manifestations. The number of skin lesions increased during his 9 days of hospitalization. Some vesicles were blisters in the beginning, without erythematous or hemorrhagic base. Some papules on extremities slowly became papulovesicles and it usually took 1 week. None of papules on the trunk became papulovesicles or vesicles. The patient abandoned further treatment.
Discussion
AITL is a rare malignancy accounting for about 2% of all non-Hodgkin lymphoma and a highly aggressive neoplasm of the elderly 1-3, 8. The median patients’ age is approximate 65 years 1-3, 8, 9. It generally presents with lymphadenopathy and is almost always accompanied by concomitant symptoms, including B symptoms, skin lesions, splenomegaly, hepatomegaly, effusion/edema/ascites, anemia, thrombocytopenia, elevated LDH, hypergammaglobulinemia and so on (Table 1).
| Authors | Federico 1 | Tokunaga 2 | Mourad 3 | Lachenal 9 | Siegert 4 | Aozasa 25 |
|---|---|---|---|---|---|---|
| Patient number | 243 | 207 | 157 | 77 | 62 | 44 |
| Age, years | ||||||
| Mean | 65 | 67 | 62 | 64.5 | 64 | 64 |
| Range | 20–86 | 34–91 | 20–89 | 30–91 | 21–87 | 25–84 |
| Male sex | 56 | 64 | 56 | 58 | 55 | |
| Lymphadenopathy | ||||||
| Generalized | 76 | 90 | 84 | |||
| Localized | 24 | 9 | 16 | |||
| Skin rash | 21 | 44 | 45 | 49 | 27 | |
| B symptoms | 69 | 60 | 72 | 77 | 68 | |
| Splenomegaly | 35 | 51 | 39 | |||
| Hepatomegaly | 26 | 26 | 52 | |||
| Effusion/edema/ascites | 14 | 26 | 25 | >38 | ||
| Bone marrow involvement | 28 | 29 | 47 | |||
| Extranodal sites, >1 | 27 | 23 | 46 | |||
| Anemia | 33 | 61 | 65 | 51 | 57 | 20 |
| Platelet count <150 × 109/L | 25 | 34 | 20 | 20 | ||
| Elevated LDH | 60 | 75 | 66 | 71 | 70 | |
| Elevated C-reactive protein | 35 | 46 | 67 | |||
| Hypergammaglobulinemia | 30 | 50 | 51 | 51 | 64 | |
| Positive Coombs test | 13 | 46 | 33 | 58 | 32 | |
- LDH, Lactate dehydrogenase.
Nearly half of AITL patients have skin lesions 1, 3-5, 8. Skin lesions can precede, follow or be concurrent to lymphadenopathy 5, 10, 11. AITL skin lesions do not have characteristics to enable it to be distinguished from other skin eruptions, especially from drug eruptions. Therefore, misdiagnosis is not rare 5, 12-14. Since AITL is almost always accompanied by concomitant symptoms (Table 1), to be familiar with the common clinical characteristics and types of skin lesions is greatly helpful to avoid misdiagnosis.
Skin lesions in AITL usually accompany pruritus 1-5, 8. Typical lesions are usually a generalized morbilliform or maculopapular eruptions on the trunk mimicking toxic erythema 2, 4, 5, 8. In the literature, uncommon skin lesions of AITL are mostly described in case reports or review articles (Table 2). It is not rare that the patient has a generalized pleomorphic rash composed of several types of rashes, such as macula, papules, maculopapules, nodules, erythroderma, urticaria, petechiae, purpura and so on. Necrotic purpura, polyarthritis, gingival ulceration, erythematous plaques (sometimes annular), toxic epidermal necrolysis, and hemorragic/necrotic nodules are also reported. Two cases of vesicles (one is pruritic papulovesicular (prurigo-like) lesion and the other is a pale erythematous eruption and violaceous plaques with bullae containing pale yellow exude.) were reported but they are apparently different from our case 5, 15.
| Authors | Age/Gender | Skin lesions | Duration of skin lesions before/after onset of lymphadenopathy | Prognosis |
|---|---|---|---|---|
| Wechsler 29 | 53/F | Erythematous macules; petechiae; purpura | 1 month after | Died (23 month) |
| Matloff 30 | 77/M | Macules; petechiae; purpura | 1 year before | Alive (4 month) |
| Seehafer 10 | 74/M | Petechiae | Concurrent | Died (3 month) |
| Seehafer 10 | 61/M | Erythroderma and purpura | Concurrent | Alive (48 month) |
| Seehafer 10 | 57/M | Petechiae | 10 month before | Alive (48 month) |
| Schmuth 31 | 73/F | Macules; petechiae; purpura | 4 week before | Alive (4 month) |
| Martel 15 | Necrotic purpura, maculopapules and urticaria | Died (26 day) | ||
| Martel 15 | Pruritic papulovesicular (prurigo-like) lesion | Alive (96 month) | ||
| Hashefi 32 | Maculopapules, petechiae | 3 month before | Died (23 month) | |
| Suarez-Vilela 33 | 67/F | Sarcoidosis | 1 month before | |
| Huang 34 | 62//M | Erythroderma; plaques; nodules | 3 year after | Died (3 year) |
| Jones 35 | 67/M | Erythroderma, toxic epidermal necrolysis | Concurrent | Died (5 month) |
| Tsochatzis 36 | 50/M | Polyarthritis, subcutaneous nodules | Concurrent | Died (2 month) |
| Jayaraman 11 | 61/M | Macules, papules, plaques, and nodules | Concurrent | Alive (5 year) |
| Ortonne 37 | 63/F | Nodules, gingival ulceration | ||
| Ortonne 37 | 54/M | Maculopapules, hemorragic/necrotic nodules | ||
| Nassar 5 | M/47 | Erythematous eruption; violaceous plaques with bullae containing pale yellow exude | 3 month before | Alive (4 month) |
| Smithberger 38 | 79/F | Cutaneous tumors and ulcerated nodules | No lymphadenopathy | |
| Ponciano 39 | 36/M | Erythematous plaques, sometimes annular | 5 year before | Alive (2 year) |
Vesicles caused by virus infection (such as HSV, VZV) in AITL patients were sporadically reported 12-14, 16, 17. Five AITL patients with VZV infection were reported in the literature and are summarized in Table 3 12-14, 16, 17. The skin lesions of varicella appear on the trunk and face, and rapidly spread centrifugally to involve other areas of the body. Manifestations consist of maculopapules, vesicles, and scabs in varying stages of evolution. Skin rashes become papules within 12 h then become vesicles within 2 days. Over a very short period of time they scab. This rapid progression from stage to stage characterizes the clinical syndrome of varicella and enables it to be distinguished from certain other vesicular eruptions 12, 18, 19. Each skin vesicle appears on an erythematous base and immunocompromised patients have more numerous lesions, often with a hemorrhagic base 18, 19. Since lesions in this patient were not symptoms of herpes zoster because of distribution of lesions and were quite unlike varicella 12, 14, 16-19, lesions are more likely caused by AITL than VZV infection. Further laboratory investigations (assessing for the presence of Epstein–Barr virus infected B cells, VZV in the lesional tissue, pathological examination of the lesional tissue, serological test and so on) can confirm the diagnosis but regretfully, the patient abandoned them.
| Authors | Age/Gender | Skin lesions of AITL | Durationa | Manifestations of VZV infection | Durationb | Prognosis |
|---|---|---|---|---|---|---|
| Kaneko 14 | 49/F | Maculopapule | Concurrent | Disseminated herpes zoster | 13 month | Died (15 month) |
| Zelickson 16 | 73/F | Hyperkeratotic papules | 1 week after | Hemorrhagic vesicles and bullae | Concurrent | Alive (4 month) |
| Boni 17 | 81/M | Maculopapule | 2 month before | Unilateral necrotizing herpes zoster | 2.5 month | Died (16 month) |
| Kanzaki 13 | 67/M | No | Not applied | An pharyngeal wall ulcerc | Concurrent | Alive (18 week) |
| Imafuku 12 | 67/M | Maculopapule | 40 day before | Varicella | 1 month | Alive |
- a Duration of skin lesions before/after onset of lymphadenopathy.
- b Duration of herpes zoster infection after onset of AITL.
- c Elevation of antibodies against HSV and VZV were observed in the patient but the ulcer was unlikely caused by VZV.
As mentioned before, hematological changes including anemia, lymphopenia, leukocytosis, neutrophilia, eosinophilia, and thrombocytopenia, are often observed on laboratory investigations but leukemoid reaction is rare. Several cases mimicking plasma cell leukemia and one case of eosinophilic leukemoid reaction were reported by computer-based searches in PUBMED 6, 7, 20. The routine blood test of this case showed a white blood cell count of 58.97 × 109/L (neutrophils% 91.64%, lymphocytes% 5.24%, monocytes% 2.44%, eosinophils% 0.42%). To the best of our knowledge, this is the first report of neutrophilic leukemoid reaction in AITL.
Treatments to AITL are similar to other noncutaneous peripheral T-cell lymphoma but results are often unsatisfactory. The majority of cases are treated with chemotherapy (CHOP, CHOEP, and CHOP followed by ICE, CHOP followed by IVE, dose-adjusted EPOCH and HyperCVAD are the first line chemotherapies), stem cell transplantation, radiotherapy, and molecular targeted therapy 3, 8, 21. Folate antagonists (methotrexate, pralatrexate), purine analogs (fludarabine, azathioprine), prednisone, cyclosporine A, lenalidomide/thalidomide, interferon, and denileukin diftitox are reported to be effective in treating AITL 1, 8, 22. Alemtuzumab and bortezomib are promising therapy options that have been explored recently and warrant 8, 22.
Though about two thirds of patients can achieve a complete remission, only half survive longer than 2 years 3, 8. International prognostic index (based on age, stage, serum LDH, ECOG/Zubrod performance status, and extranodal site) and prognostic index for peripheral T-cell lymphoma (based on age, performance status, serum lactate dehydrogenase (LDH) levels, and bone marrow involvement) are widely accepted and used 2. Skin rashes imply poor prognosis 4, 23, 24. Other factors, such as male sex, B symptoms, edema, ascites, mediastinal lymphadenopathy, anemia, thrombocytopenia, lymphocytopenia, elevated white blood cell, decreased hemoglobin, elevated IgA levels, lymph node eosinophilia, the presence of clear and convoluted cells, high microvessel density measured in the microenvironment, higher ratio of M2 macrophages, failure to achieve complete remission, and drug exposure are reported to correlate with poor prognosis 2, 3, 23-28. So far, due to limited data available, prognostic factors in AITL sometimes yield controversial results.
Conflict of Interest
The authors have no competing interest.