Impact of statins on the survival of patients with cancer: a nationwide population-based cohort study in South Korea
List of abbreviations
-
- ACM
-
- all-cause mortality
-
- ASCVD
-
- atherosclerotic cardiovascular disease
-
- CI
-
- confidence interval
-
- CSM
-
- cancer-specific mortality
-
- DDD
-
- defined daily dose
-
- HMG-CoA
-
- 3-hydroxy-3-methylglutaryl-coenzyme A
-
- HR
-
- hazard ratio
-
- NHIS
-
- National Health Insurance Service
-
- NSC DB
-
- National Sample Cohort database
For over 30 years, 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors, statins, have been recommended worldwide as cost-effective lipid-lowering drugs for cardiovascular disease [1]. Cheng et al. suggested that lipid synthesis inhibitors are a promising anti-cancer treatment in preclinical studies and early phases of clinical trials [2]. However, the association between statin use and cancer incidence or survival remains controversial [3, 4]. In addition, most studies on the beneficial effect of statins were based on the survival of one specific cancer, without comparing its effectiveness under various circumstances in real-world data [5, 6]. Therefore, in this study, we investigated the association between statin use and cancer survival in various cancer types, over a long period, with the aim of identifying which daily statin requirements could have beneficial effects on survival among East Asians.
The National Health Insurance Service (NHIS) in South Korea (hereafter referred to as Korea) implements a single national health insurer and compulsory healthcare insurance system that covers the entire population. We used the NHIS-National Sample Cohort database (NHIS-NSC DB) 2.0, which contains the data of approximately one million persons (2.2% of the total eligible population in 2006) selected by stratified random sampling [7]. In our cohort, patients’ health-related indicators were collected during the prospective observation period (2006-2015). The inclusion and exclusion criteria for this study are shown in Supplementary Figure S1. Other details of the methods can be found in the Supplementary Materials. Briefly, given that the number of statin users who were at least 36 years old in the NHIS-NSC DB 2.0 was high, 22,669 patients aged ≥ 36 years with newly diagnosed cancer after 2005 were included and followed up until December 31, 2015. Among them, 1,859 statin users were matched with 3,535 non-statin users (Supplementary Table S1).
The mean (median) follow-up duration of this study was 4.3 (4.1) years, ranging up to 10.9 years. A total of 1,797 patients died from cancer. Sixty-four patients died from atherosclerotic cardiovascular disease (ASCVD), and 353 died from other causes. In univariate analysis, both all-cause mortality (ACM) and cancer-specific mortality (CSM) were significantly lower in statin users than in non-statin users, although statin users were significantly older and had more comorbidities (Supplementary Figure S2A and S2B; P < 0.001, log-rank test). The CSM curves show an increasing discrepancy between the groups, whereas the ACM curves tend to overlap in the late period. Contrastingly, there was no difference in the curves of deaths from ASCVD or other causes between the groups (Supplementary Figure S2C and S2D). The adjusted hazard ratios (HRs) of statin use for ACM (0.68 [95% confidence interval (CI), 0.62–0.75]; P < 0.001) and CSM (0.67 [95% CI, 0.61–0.74]; P < 0.001) were significantly lower in all cancer types than those in non-statin users (Supplementary Figure S2).
In the past decade, compared to other solid cancers, the incidence of thyroid cancer in Korea has markedly increased. Consequently, most patients with indolent thyroid cancer were censored at the end of our study. Even after excluding patients with thyroid cancer, the trends of cumulative mortalities and adjusted HRs remained unchanged (Supplementary Figure S3). Considering the competing risks, the sub-distribution HRs of statin users, when compared to non-statin users, were significant (0.67 [95% CI, 0.62–0.76]) for cancer-specific death but were not significant for ASCVD death (0.92 [95% CI, 0.55–1.52]) (Supplementary Table S2). These findings were consistent with results from the multivariate Cox regression analysis.
Results of the subgroup analyses according to cancer type (based on the International Statistical Classification of Diseases, 10th Revision) are shown in Figure 1. The adjusted HRs for ACM in statin users were significantly lower than those in non-statin users for four cancer types: kidney and bladder, colorectal, prostate and other male genitalia, and gastric and esophageal cancers (Figure 1A). The adjusted HRs for CSM were similar for the four cancer types (Figure 1B). The adjusted HRs for CSM in kidney and bladder cancer, and gastric and esophageal cancer were 0.39 (95% CI, 0.20–0.75) and 0.75 (95% CI, 0.58–0.96), respectively (Figure 1B). Moreover, according to the proportional hazard assumption satisfaction, the lowest adjusted HRs for CSM of colorectal cancer were 0.20 (95% CI, 0.09–0.47), observed before 6 months of follow-up, and 0.65 (95% CI, 0.46–0.93) after 6 months of follow-up in statin users (Figure 1B). Limited samples for other cancer types might have been associated with a certain level of unavoidable bias in the observed differences in mortality between the statin and non-statin users; however, they accounted for only 10.34% of all the subjects.
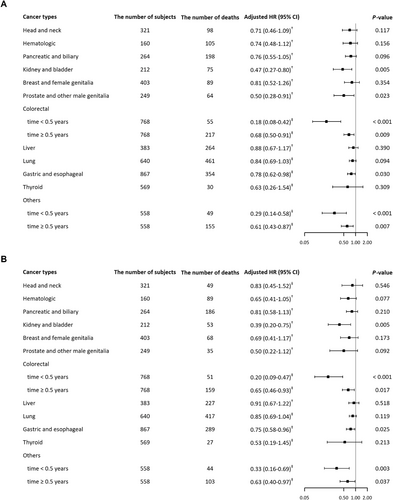
Adjusted HRs for all-cause and cancer-specific mortality in different cancers.
Adjusted HRs were obtained from a subgroup analysis of 12 cancer types. (A) all-cause mortality, (B) cancer-specific mortality. The follow-up time of patients with colorectal cancer and other cancers in years was divided into two sections using the Heaviside function by six months because the proportional hazard assumption was violated.
†Adjusted for income level (0th, 1-5th, 6-10th), residential area, DM before cancer diagnosis, ASCVD before cancer diagnosis, and secondary cancer after cancer diagnosis.
‡Adjusted for income level (0th, 1-5th, 6-10th), residential area, DM before cancer diagnosis, ASCVD before cancer diagnosis, and secondary cancer after cancer diagnosis as a time-dependent variable.
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CI, confidence interval; DM, diabetes mellitus; HR, hazard ratio.
In the analysis of time-dependent association, current statin use for more than 3 months had the lowest HRs for ACM (0.44 [95% CI, 0.38–0.50]) and CSM (0.40 [95% CI, 0.34–0.46]), whereas past statin use had HRs for ACM and CSM of 0.72 (95% CI, 0.65–0.81) and 0.81 (95% CI, 0.71–0.91), respectively (Supplementary Table S3). Furthermore, the adjusted HRs for CSM were consistently low in the analyses of the statin source and solubility, even though they are not consistent in pharmaceutical ingredients and potency (Supplementary Figure S4). These results were similar to the adjusted HRs for ACM (Supplementary Figure S5). In all defined daily dose (DDD) quintile-based groups, the adjusted HRs for CSM were significantly decreased, ranging from 0.60 (95% CI, 0.49–0.74) to 0.75 (95% CI, 0.62–0.91) (Supplementary Figure S6). A dose-dependent pattern was not observed where the second dose level for CSM and the third dose level for ACM had the lowest HRs. Interestingly, we observed that the minimum DDD of statins had a favorable effect on cancer survival, which is consistent with a previous study that suggested that low-dose or lower-efficacy statins are efficient in the management of dyslipidemia in most Koreans, unlike in Western patients [8]. Thus, we suggested a minimum DDD of statins for improved cancer survival among East Asian patients. The adjusted HRs for ASCVD death in all the analyses were not significant.
The good prognosis noted among statin users in our study might be interpreted as an objective, practical reflection of the effect of statins on cancer survival. Our extensive Korean cohort study demonstrated that statin use before cancer diagnosis reduced ACM and CSM by up to approximately 30%, which is consistent with a previous meta-analysis of 55 articles [9]. The negligible difference in risks between ACM and CSM was indicative of accurate cancer diagnoses in our cohort since most of the patients died from cancer. Statin users in our study consisted of older and more comorbid patients than non-statin users. Nonetheless, statin use resulted in beneficial findings unlike previous epidemiologic studies due to healthy-user bias [10]. This study focused on the effect of long-term regular statin use, although prevalent user or immortal time biases could not be excluded [10].
In conclusion, our large cohort data demonstrated that regular use of low statin doses before cancer diagnosis might be beneficial in reducing the risks of ACM and CSM in East Asian patients. Our analysis provides a basis for translational research on statin use in healthy persons and persons without cancer. Future studies are needed to identify the specific mechanisms of statin use as predictive markers for cancer survival.
DECLARATION
AUTHORS’ CONTRIBUTIONS
Study concept and design: SL. Data acquisition: JA, SW. Data analysis and interpretation: JA, SW, SL. Manuscript writing: JA, SW, SL. Critical revision: All authors. Final approval of manuscript: All authors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the Institutional Review Board (IRB, No: E1911/002-007) of Seoul National University, Seoul, Republic of Korea. Written informed consent was not necessary because personal information was anonymized, and the database was only accessed using a remote-controlled desktop.
FUNDING
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HF20C0172).
CONFLICT OF INTEREST
The authors declare there are no conflicts of interest.
ACKNOWLEDGMENTS
The National Sample Cohort DB 2.0 was provided by the National Health Insurance Sharing Service [Research Administration No. NHIS-2019-2-256], and the results of the study are not related to the National Health Insurance Corporation.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the Korean National Health Insurance Sharing Service (NHISS). Data are available at https://nhiss.nhis.or.kr/ with the permission of the NHISS.




