Leucine-Rich Glioma-Inactivated 1 versus Contactin-Associated Protein-like 2 Antibody Neuropathic Pain: Clinical and Biological Comparisons
Abstract
Pain is a under-recognized association of leucine-rich glioma-inactivated 1 (LGI1) and contactin-associated protein-like 2 (CASPR2) antibodies. Of 147 patients with these autoantibodies, pain was experienced by 17 of 33 (52%) with CASPR2- versus 20 of 108 (19%) with LGI1 antibodies (p = 0.0005), and identified as neuropathic in 89% versus 58% of these, respectively. Typically, in both cohorts, normal nerve conduction studies and reduced intraepidermal nerve fiber densities were observed in the sampled patient subsets. In LGI1 antibody patients, pain responded to immunotherapy (p = 0.008), often rapidly, with greater residual patient-rated impairment observed in CASPR2 antibody patients (p = 0.019). Serum CASPR2 antibodies, but not LGI1 antibodies, bound in vitro to unmyelinated human sensory neurons and rodent dorsal root ganglia, suggesting pathophysiological differences that may underlie our clinical observations. ANN NEUROL 2021;90:683–690
Patients with autoantibodies against leucine-rich glioma-inactivated 1 (LGI1) and contactin-associated protein-like 2 (CASPR2) most often present with autoimmune encephalitis1-3 and less commonly with peripheral nerve hyperexcitability (PNH) and/or dysautonomia1, 4-6 Pain has been described in approximately 10 to 30% of these patients5, 7, 8; however, prior studies have not utilized validated pain scores, quantified outcome measures, or investigated the underlying neurobiology. Herein, inspired by an index patient with LGI1 antibodies and immunotherapy-responsive neuropathic pain, we systematically characterized clinical features, therapeutic responses, outcomes, and potential pathophysiological mechanisms in 147 patients with LGI1 and/or CASPR2 antibodies.
Patients and Methods
Clinical Characterization
- The Douleur Neuropathique 4 (DN4) was used to define neuropathic pain at disease nadir by a score ≥ 3 (without physical examination).11
- Patient-Reported Outcome Measurement Information System Pain Interference (PROMIS-PI; maximal score = 40) was used to quantify pain interference at nadir of pain, after immunotherapy, and at latest follow-up (median = 5 years, range = 1–17).
- Five-level EuroQol 5-dimension quality of life assessment (EQ-5D) and EQ-5D visual analogue scale were used to evaluate functional domains and self-reported quality of life (QOL; 0 worst to 100 best health) at latest follow-up.
Laboratory-Based Characterization
Intraepidermal nerve fiber density (IENFD) was determined from skin biopsies12 and human leukocyte antigen (HLA) genotyping from blood,9 both as previously described.
The first available serum sample was tested using (1) live cell-based assays (CBAs) for LGI1 and CASPR2 antibodies, with samples defined as positive at serum endpoint dilutions ≧1:20 for LGI1 and ≧1:100 for CASPR2 antibodies1; (2) immunohistochemistry (IHC) using rodent hippocampal sections; (3) live cocultures of human induced pluripotent stem cell (iPSC)-derived sensory neuronal cultures myelinated by rat Schwann cells13, 14; and (4) live murine dorsal root ganglion (DRG) cultures.15 Samples were compared to the following age-/sex-matched controls: healthy controls (n = 12); and patients with characteristic central nervous system (CNS) manifestations but without pain, who have antibodies against LGI1 (n = 6), CASPR2 (n = 8), or both antigens (n = 2).
GraphPad (San Diego, CA) Prism (v8.0) and Adobe Illustrator were used for statistical analyses/figures. Fisher exact test was used to compare binary discrete and Mann–Whitney test to compare continuous variables. Informed consent from patients and controls was obtained with approvals REC16/YH/0013 and 14/SC/0280. Animal work complied with UK Home Office license Ref.P1DBEBAB9.
Results
Index Patient
A 66-year-old previously well female presented with 18 months of pain, which commenced as a hot sensation in both feet. Subsequently, she developed shooting pains in her thighs, buttocks, arms, and torso, stereotyped episodes of burning pain described as “being tortured with stinging nettles”, and persistent severe hyperesthesia with a glove and stocking distribution also involving her torso. Symptoms were triggered by heat and movement, and severely restricted activities. Three neurologists observed normal nerve conduction studies and diagnosed her with fibromyalgia or psychogenic pain. A fourth found LGI1 antibodies (endpoint dilution of 1:640) and markedly reduced skin IENFD. High-dose prednisone resulted in complete symptom resolution within 2 days, and a marked fall in PROMIS-PI ratings, from 36/40 to 8/40. Nine months later, a patient-initiated corticosteroid wean was associated with a relapse of pain, which partially responded to reinitiation of corticosteroids and plasma exchange.
This patient prompted us to examine pain across a large cohort of patients with LGI1 and/or CASPR2 antibodies.
Autoantibodies and HLA Genotypes
Antibodies against LGI1 (n = 108), CASPR2 (n = 33), or both targets (n = 6) were detected using live CBAs (Fig 1). Samples reaching endpoint dilutions of ≧1:80 for LGI1 antibodies and ≧1:800 for CASPR2 antibodies consistently showed reactivity by IHC. HLA genotypes were accordant with established associations for both disorders9: 10 of 11 (91%) LGI1 antibody patients carried HLA-DRB1*07:01, and 9 of 17 (53%) CASPR2 antibody patients carried HLA-DRB1*11:01.
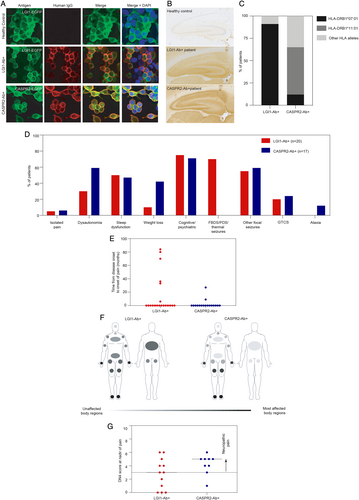
Clinical Features and Investigations
Thirty-nine of 147 patients described pain as a component of their illness, including 52% (17/33) of the CASPR2-antibody cohort versus 19% (20/108) with LGI1 antibodies (p = 0.0005), and 2 of 6 with both antibodies (Table S1). Isolated pain was observed in 2 patients (the index case with LGI1 antibodies, and another patient with CASPR2 antibodies); they carried HLA-DRB1*07:01 and HLA-DRB1*11:01, respectively, and their sera demonstrated high endpoint dilutions on live CBAs with characteristic binding on IHC. The remaining 37 of 39 (95%) described pain in addition to CNS features and/or systemic involvement (weight loss, dysautonomia; see Fig 1). Thirty of 39 patients developed pain concurrent with the onset of CNS symptoms. In 9 of 39 (23%; Fig 1E), pain began after onset of CNS features by a median of 33 months (range 2-84). Fibromyalgia, psychogenic pain, or chronic fatigue syndrome were the original diagnoses in 7 of 39 (18%). Electrophysiologically confirmed PNH was present in 16 of 39 (41%) patients. Nerve conduction studies were normal in 29 of 39 (74%), with one quarter showing a mild sensory axonal polyneuropathy.
Questionnaires revealed that both the LGI1 and CASPR2 antibody cohorts had predominant length-dependent distributions of pain, with truncal involvement exclusive to the LGI1 antibody cohort (5/12 [42%] vs 0/9 [0%] with CASPR2 antibodies; p = 0.045; Fig 1E). At nadir of pain, both groups had comparable DN4 and PROMIS-PI scores with neuropathic pain in 7 of 12 (58%) LGI1 and 8 of 9 (89%) CASPR2 antibody patients (see Fig 1F and Table S1).
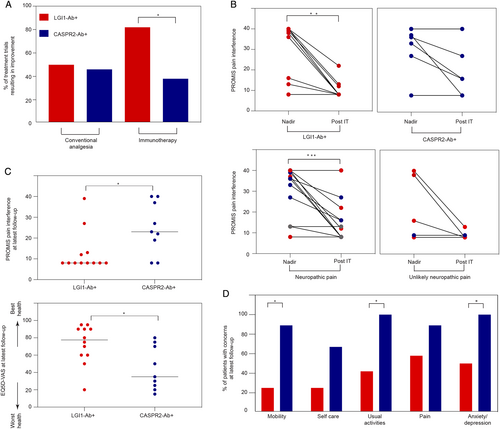
Short- and Long-Term Outcomes after Treatment
Patients were administered a median of 2 conventional analgesic agents (range = 1–6; most commonly pregabalin, gabapentin, and amitriptyline) and a median of 2 immunotherapies (range = 1–4, mostly prednisone and intravenous immunoglobulin or plasma exchange). Improvement of pain with conventional analgesic trials was reported in approximately half of both LGI1 (7/14; 50%) and CASPR2 antibody (6/13; 46%) patients. In contrast, 18 of 22 (82%) immunotherapy trials in LGI1 antibody patients resulted in a rapid improvement in pain, over a median of 14 days (range = 2–21), compared to 5 of 13 (38%) in CASPR2 antibody patients (p = 0.024; Fig 2, Table S1). Moreover, by comparison to the CASPR2 antibody cohort, the LGI1 antibody patients showed the most marked PROMIS-PI reductions following immunotherapy (p = 0.008): this was particularly pronounced in those with neuropathic pain (p = 0.0005, Fig 2B). The lower PROMIS-PI scores in LGI1 antibody patients were sustained at latest (median = 5 years) follow-up (p = 0.025, Fig 2C) and, at this time point, CASPR2 antibody patients lower overall self-reported health (p = 0.019), with greater concerns in the domains of mobility (p = 0.014), usual activities (p = 0.019), and anxiety/ depression (p = 0.043, Fig 2D).
Intraepidermal Nerve Fiber Densities
Four patients underwent IENFD evaluation at a median of 20 months (range = 13–30) following onset of pain (Fig 3A–D). One patient with CASPR2 antibodies, CNS involvement, and non-neuropathic pain (DN4 score = 1) had an IENFD in the healthy control range. This contrasted with strikingly low, sometimes absent, IENFDs in 3 patients with LGI1 or CASPR2 antibodies, all with neuropathic pain and DN4 scores of 4–5 (see Fig 3D).
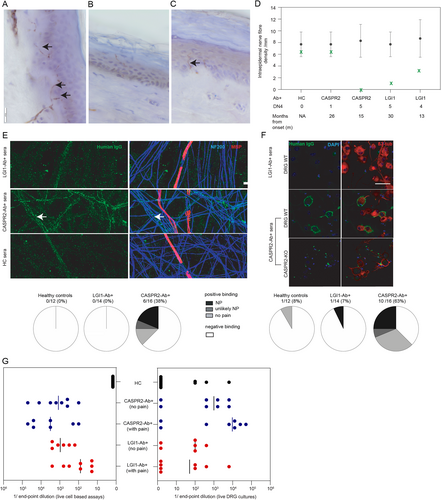
Binding to Live Neuronal Cultures
LGI1/CASPR2 antibody titers by live CBA, and their binding to extracellular domains expressed on neurons with the potential to mediate small fiber pain, were assessed from the 16 of 39 patients with pain and sufficient sera available, and from 26 controls. By contrast to LGI1 antibody and healthy control sera, CASPR2 antibody sera showed a higher frequency of binding to both unmyelinated axons of live iPSC-derived human sensory neurons (LGI1 antibody 0/14 [0%] vs CASPR2 antibody 6/16 [38%], p = 0.019) and live rodent DRG neurons (LGI1 antibody 1/14 [7%] vs CASPR2 antibody 10/16 [63%], p = 0.0024). All CASPR2 antibody binding was abrogated in DRG cultures derived from a CASPR2 knockout mouse (see Fig 3E, F). The binding and endpoint dilutions of LGI1 and CASPR2 antibodies were similar between patients with and without pain (see Fig 3G).
Discussion
This study shows neuropathic pain as a frequent and often rapidly immunotherapy-responsive feature in a large cohort of patients with LGI1 and CASPR2 antibodies, including ~10% with relatively isolated pain syndromes. A comparison of patients with LGI1 versus CASPR2 antibodies revealed that length-dependent pain was frequent in both groups, whereas truncal involvement was exclusive to LGI1 antibody patients. The LGI1 antibody patients demonstrated more dramatic responses to immunotherapy, often observed within a few days as highlighted by our index case. Their preferential response to immunotherapy over conventional symptomatic treatments is reminiscent of the superior effect of immunotherapy versus anticonvulsant therapy in LGI1 antibody–associated seizures.10 Importantly, this benefit was sustained at 5-year follow-up in LGI1 antibody patients. The higher rate of residual immunotherapy-resistant pain in CASPR2 antibody patients interfered with activities of daily living and was associated with reduced QOL.
LGI1 and CASPR2 are expressed in the CNS and also in the peripheral nervous system, including peripheral nerves and DRGs.15-17 Our observations, and those of others,5, 7, 8, 15, 18 suggest small nerve fiber dysfunction may underlie our patients' pain, as supported by the distal limb predominance and neuropathic quality with typically both unremarkable nerve conduction studies and large nerve biopsies.8 Furthermore, we show IENFD can be markedly reduced in both LGI1 and CASPR2 antibody patients, similar to prior observations from CASPR2 antibody patients.7 A direct effect on peripheral sensory neurons is supported by the DRG hyperexcitability observed in rodents administered CASPR2 immunoglobulin Gs (IgGs) from 2 patients.15 Here, we extend these data by showing that serum IgGs from many CASPR2 antibody patients bind with high frequency to both rodent DRG neurons and, for the first time in human tissue, iPSC-derived unmyelinated sensory nerve axons. The neuronal IgG binding from CASPR2 antibody patients without pain suggests additional factors may regulate their neuropathic potential in vivo, for example, blood nerve barrier access. Additionally, our data suggest CASPR2 IgGs are unable to access the juxtaparanode underneath the myelin sheath, as demonstrated by the undetectable IgG binding to our in vitro myelinated axons. Overall, the high rate of CASPR2 IgG binding may underly the more frequent and sustained pain observed in this cohort.
The absence of LGI1 antibody binding to both preparations may be because LGI1 is a soluble molecule and hence may not be retained in vitro.16 Alternatively, a CNS action of LGI1 antibodies may mediate pain consistent with observations including the frequent concurrent encephalopathy, striking binding to CNS tissue, and the truncal distribution reminiscent of central cord syndromes. The molecular basis for frequent immunotherapy-mediated pain resolution despite small nerve fiber loss requires further study.
Our work methodologically advances the field with (1) the first structured neuropathic pain evaluations using validated clinical and laboratory tools; (2) ascertainment of transferable measures of QOL for future cross-comparisons; (3) long-term follow-up data; and (4) the study of strictly autoantibody-mediated conditions, by exclusion of voltage-gated potassium channel antibody–positive patients without LGI1/CASPR2 reactivities.8, 18, 19 Limitations include the inherent caveats of a retrospective cohort review and the potential for recall bias in patients with residual cognitive impairment.
In summary, here, by contrasting LGI1 and CASPR2 antibody patients, we advance established differences between their clinical presentations and HLA associations to now differentiate their pain in terms of its relative frequency, clinical characteristics, short- and longer-term therapeutic responses, and the underlying neurobiology. Our detailed characterization of "autoimmune pain" syndromes20 aims to ensure appropriately selected patients are directed toward early proactive immunotherapy to limit long-term morbidity and associated disability, and suggests that autoantibody testing in cohorts with a prior diagnosis of fibromyalgia or psychogenic pain may identify a modest subset with immunotherapy-responsive pain20 and inform their biology.
Acknowledgments
We thank Dr G. Baskozos for assistance with generating Figure 1C, and Dr A. Candalija for technical assistance with the sensory neuronal cocultures. S.Ra. is supported by an NHMRC Early Career Fellowship (APP1141169). This research was funded by the Wellcome Trust (104079/Z/14/Z) and the Medical Research Council (MR/V007173/1). For the purpose of open access, the author has applied a CC BY public copyright license to any author-accepted manuscript version arising from this submission.
Author Contributions
S.Ra. and S.R.I. contributed to conception and design of the study, as well as acquisition and analysis of data and drafting a significant portion of the manuscript or figures. All coauthors contributed to acquisition and analysis of data, in addition to editing and approval of the final draft.
Potential Conflicts of Interest
J.D. and D.L.B. have a patent relating to the use of CASPR2 for the treatment of excess neuronal activity in pain and epilepsy (PCT/GB2017/052909). S.R.I. and P.W are coapplicants and receive royalties on a licensed patent application WO/2010/046716 (UK patent no. PCT/GB2009/051441) entitled "Neurological Autoimmune Disorders." All other authors have no relevant disclosures.