COVID-19 Policy Modeling in Sub-Saharan Africa
Valerie Mueller is an associate professor at the School of Politics and Global Studies at Arizona State University and a Non-resident Fellow at the International Food Policy Research Institute. Glenn Sheriff is an assistant professor at the School of Politics and Global Studies at Arizona State University. Corinna Keeler is a postdoctoral associate at the Department of Epidemiology at the University of North Carolina at Chapel Hill. Megan Jehn is an associate professor at the School of Human Evolution and Social Change at Arizona State University.
Editor in charge: Craig Gundersen
Abstract
After an initial delay, Sub-Saharan Africa (SSA) is being hit by the pandemic. Demand for exports is falling and caseloads are rising. Governments have approached this crisis with a range of policy options. Optimal policy balances reduced infection rates with lost economic output. This paper discusses how an economic-epidemiological model used to analyze policy in high-income countries could be adapted to a context where poverty considerations are paramount. Differences in country characteristics across the continent affect benefits and costs of alternative policy designs. We conclude by highlighting data needs and model calibration challenges for COVID-19 policy research in SSA.
If the 1918 influenza pandemic is any guide, COVID-191 may have disastrous consequences for human health and well-being in Sub-Saharan Africa (SSA). Four of the six countries with the highest cumulative influenza death rates were in Africa, with Kenya experiencing the worldwide maximum (Barro, Ursúa, and Weng 2020). Despite a relatively young population, comorbidities among Africans can worsen the severity and frequency of illness (Nepomuceno et al. 2020); two-thirds of the world's HIV-infected population and one-third of those carrying tuberculosis reside in Africa (Katz et al. 2012). In addition to mortality effects, the combination of high comorbidities and limited healthcare capacity threatens worker productivity, potentially delivering an output shock to a region already struggling with extreme poverty. Policies for fighting spread of the disease can remove healthy workers from productive activity, thus increasing household vulnerability to malnutrition and other poverty-induced illnesses at the same time as a global recession is causing a drop in international demand for the region's exports.
How can SSA governments thread this needle? Here, we describe a combined economic-epidemiological framework that is useful for evaluating the benefits and costs of policy alternatives. Our focus is on how models that have thus far been applied to high-income countries can be calibrated to the SSA context. The discussion is intended both to help applied interdisciplinary policy analysis and to inform data collection efforts.
Early evidence suggests that social distancing policies are effective tools for slowing the spread of COVID-19 (Hsiang et al. 2020). What remains poorly understood is whether the same policies adopted largely in high-income countries are suitable for SSA, given differences in demographics, wealth, health, and medical infrastructure. Zahra Diop et al. (2020) predict that the younger age distribution and high proportion of rural residents may reduce severity of symptoms relative to Europe, but the incidence of HIV, tuberculosis, and other illnesses may work in the opposite direction.
The objective of this article is to conceptualize how one might evaluate the tradeoffs of COVID-19 mitigation policies in SSA. As a starting point, we describe how the current pandemic has affected a selection of eight countries (Botswana, Burkina Faso, Cameroon, Kenya, Mali, Mozambique, Uganda, and Zambia) and how government policy has responded (Section I). In Section II, we provide a brief overview of the main epidemiological approach used to model the spread of the disease, and show how economists have adapted the model for benefit–cost analysis of policy responses. Since most applied policy analysis has focused on high-income countries, in Section 3, we outline the key conceptual ways in which both the epidemiological and economic aspects of the analysis might differ in SSA. Our final section concludes with data-collection implications for calibrating economic-epidemiological COVID-19 models for SSA.
Effects on Africa and Policy Response
SSA is facing a growing health and economic burden of COVID-19 as the disease diffuses widely across the world (African Union 2020). Here, we focus on eight representative countries on the basis of wealth, labor force composition, and health capacity (Table A1 summarizes key country characteristics). Half the countries are considered low-income economies and the other half lower-middle to upper-middle economies (World Bank 2020b). Five of the eight countries rely on the agricultural sector as a primary employer of labor (ILO 2020). Hospital beds available per 10,000 people range from 1 in Mali to 20 in Zambia (World Bank 2020c). Together, these eight countries had a cumulative burden of 11,819 confirmed cases and 395 confirmed deaths due to COVID-19 as of June 1, 2020.2 The incident case rate within these countries ranged from 7.86 cases per million population (Mozambique) to 227.44 cases per million population (Cameroon), and mortality rates ranged from 0 (Uganda)3 to 7.35 deaths per million (Cameroon).4
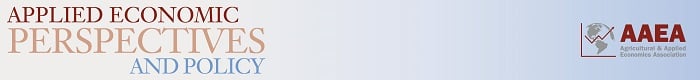
In addition to the increasing morbidity and mortality, the economic effects in the first three months of the pandemic in SSA have been severe. Externally, the epidemic has provoked a worldwide recession resulting in a drop in demand for many of Africa's key export commodities (African Union 2020).5 Figure 1 shows recent price trends in the top exports of the eight countries: gold, copper, crude oil, sawn hardwood, and agriculture (a simple average of cotton, cocoa, coffee, and tea). Most of these commodities have experienced negative price shocks relative to January 2019, ranging from 47% for oil to just under 5% for hardwood. Gold (a leading export for Burkina Faso, Mali, and Uganda) is the exception, seeing its value increase by almost a third. In general, the pandemic has led the IMF to revise sharply downward its 2020 GDP growth rate estimates from projections made a year earlier. The price effects on GDP may manifest in the form of unemployment or revenue and wage losses in the agricultural and mining sectors. Botswana, Cameroon, and Zambia experienced the largest shocks (Table A1).
Source: Author calculations based on data from IMF (2020).
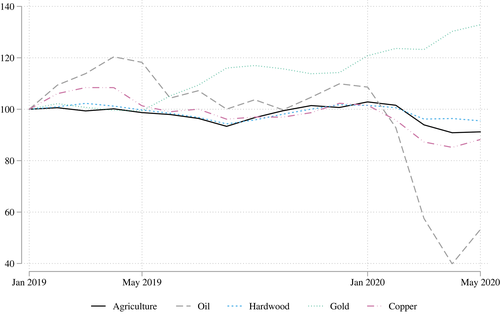
[Color figure can be viewed at wileyonlinelibrary.com]As in many high-income countries, African governments have responded to the pandemic by implementing a range of policies to limit the spread of the disease as well as to provide some economic assistance to their population. We focus on criteria for accessing COVID-19 diagnostic testing (testing), implementation of stay-at-home or shelter-in-place policies (SAH), and nationally mandated workplace closure policies (workplace). Each of these policies intersects with economic activity in the country, either by affecting the ability of people to continue working, or by conditioning access to testing upon the industry in which a given person is employed. Figure 2 illustrates both the spatial and temporal distribution of these policies.
Notes: Authors' calculations using data from Hale et al. (2020b). WFH=Work from home.
[Color figure can be viewed at wileyonlinelibrary.com]Testing policies, shown in the lefthand column of figure 2, are an indicator of policy response within the health system. Among the eight focal countries, only Cameroon had expanded testing access to include anyone experiencing COVID symptoms. The other seven countries had more restrictive testing, making them available to only those who both showed COVID symptoms and met other criteria such as a known positive contact or a high-risk occupation.
The majority of countries in Africa required residents to stay at home (middle column of figure 2). Among the eight focal countries, only Cameroon never implemented SAH guidance, while Mali and Zambia instituted SAH requirements or recommendations in March and April but ended the policy at the beginning of May. In contrast, beginning in early April, Kenya enacted a stringent SAH requirement.
A range of workplace restrictions are being implemented in the African continent (rightmost column of figure 2). Of the eight focal countries, only Mozambique has not initiated any general workplace closure guidance (with the exception of certain entertainment establishments such as theatres and bars). The remaining seven required some or all nonessential workplaces to close during the months of April and May. By the start of June, both Mali and Botswana had relaxed these measures.
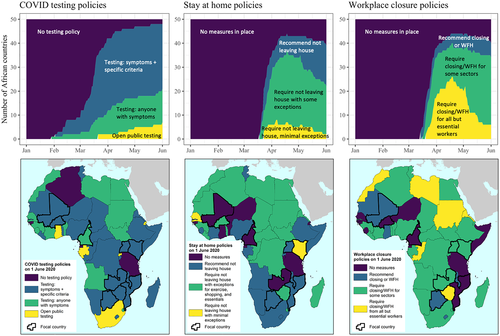
Figure 3 illustrates time trends in policies, measured as a Government Response Index (GRI), and disease cases per million (Hale et al. 2020a, 2020b). The GRI is a composite indicator of health, workplace, and SAH policies combined with government economic support such as income stabilization and debt relief. All countries significantly increased their policy response as (or shortly before) the first cases appeared in mid-March. By mid-May, all countries, except Kenya and Mozambique, had begun to relax some measures. The case trajectory has varied widely across countries, remaining relatively flat in Botswana, Mozambique, and Uganda, and showing relatively large increases in Mali, Zambia, and especially Cameroon.
Notes: The Government Response Index (right axis) is based on the eight containment and closure policies, two economic response policies, and three health policies (for detailed methodology see github.com/OxCGRT/covid-policy-tracker/blob/master/documentation/index_methodology.md). The left axis represents cases per million inhabitants.
Source: Authors, based on data from Hale et al. (2020b).
[Color figure can be viewed at wileyonlinelibrary.com]Given the adverse economic effects of the disease itself in terms of both a drop in demand for the region's products and the effect on worker productivity, a natural question arises regarding the appropriate level of the policy response. The aggressive testing and contact tracing undertaken by much of SSA are relatively low-cost means for preventing the initial spread of the disease. The social distancing policies necessary for containment once it becomes more pervasive, however, can pose significant costs in terms of lost government revenue and household income in countries where many were in a precarious economic condition even before the pandemic. In the next section, we show how models containing elements of both epidemiological and economic theory are being applied to inform how policymakers can decide what is the appropriate level of stringency.
Modeling COVID-19 Policy
This simple model has been modified to incorporate a variety of factors such as a fatality rate (which can also be a function of hospital capacity), age-differentiated disease effects, testing, partial isolation of the infected, and development of a vaccine.6
The SIR model can be adapted for use in applied economic policy analysis using a simplified cost of illness (COI) framework combined with a cost of premature mortality. A full COI approach would estimate direct costs such as medical expenses and indirect costs such as productivity losses of infected workers and members of the infected household (e.g., Cropper et al. 2004). The COI metric is generally a lower-bound cost estimate as it does not include disutility from illness or death.
The COI approach can be supplemented by estimating mortality cost. This cost is often monetized using estimates of an individual's willingness to pay to avoid a marginal increase in the risk of death. Aggregating the valuation of small risk reductions up to 100% yields a monetary amount per life “saved,” commonly referred to as the value of a statistical life (VSL).7 Similarly, it is possible to calculate the disutility of being sick (as in Cropper et al. 2004, for example).
Several studies (e.g., Alvarez, Argente, and Lippi 2020; Eichenbaum, Rebelo, and Trabandt 2020) show how some of these economic factors can be incorporated into a simple SIR model. The basic model abstracts from medical expenses, focusing instead on lost worker productivity. A fraction of the infected are assumed to be at least partially unavailable to work until they recover (or ever, if their illness proves fatal). The recovery period is (1/γ), with the end of the recovery period resulting in immunity or death, depending in turn on a fatality rate parameter. The additional key economic parameters are a value of workday output, and the VSL.
One can also construct a social welfare function (SWF) for deriving an optimal policy or comparing relative net benefits of alternative policy instruments. For example, suppose a proportion λ of infected cannot work, and of those a fraction ϕ die. All other workers can earn wage w. The social cost of death is v, which at a minimum would be foregone future earnings, but could also incorporate a VSL measure.
Here the values of S(t), I(t), and R(t) are governed by their respective equations of motion (suitably modified versions of Equations 1-3)).
The lockdown would have the benefit of reducing the flow of new infections. The benefits of the lockdown are the delay in the costs of death and lost workdays to illness.8 The lockdown itself would incur the cost of a productivity loss for the infected still capable of working and the susceptibles and recovereds who are forced to stay home.
This modeling framework permits the analyst to choose policy parameters (such as lockdown stringency and duration) that maximize welfare. As the models generally lack analytical solutions, the optimum must be calculated using numerical methods. Alternatively, one can input the parameters of a candidate policy into the social welfare function to see if it passes a benefit–cost test (i.e., welfare with the policy is higher than welfare absent a policy).
Adapting an Economic SIR Model to Africa
The COVID-19 epidemic has sparked a surge in economic applications of the SIR model for high-income countries, especially the U.S. In this context, the policy problem has typically been framed in terms of evaluating the public health benefits of actions, such as lockdowns, to justify their costs in terms of lost GDP (e.g., Acemoglu et al. 2020; Eichenbaum, Rebelo, and Trabandt 2020; Thunström et al. 2020). U.S.-based models typically use the epidemiological parameters calibrated by Ferguson et al. (2020). Studies vary in assumptions regarding the VSL, but the benchmark value used by the U.S. EPA in benefit–cost analysis of federal environmental regulation is approximately $10 million.9
These model simulations have generally arrived at a consensus that social distancing policy passes a benefit–cost test. A natural question arises whether a similar conclusion is applicable for lower-income countries. Greenstone and Nigam (2020), for example, estimate that 90% of the U.S. benefits from social distancing accrue to those over the age of 50. Given that lower-income countries tend to have much younger populations, authors such as Barnett-Howell and Mobarak (2020) have raised doubts as to whether social distancing would pass a benefit–cost test there, particularly given the pressing health problems stemming from poverty and malnutrition.
Apart from a younger population, lower-income countries can also be expected to have a lower VSL. VSLs are calculated from observations, typically using US data, of how much income individuals are willing to give up to reduce mortality risk (e.g., accepting a lower wage for a less risky job). If safety is a normal good, richer people can be expected to be willing to pay more for it. Since little data have been collected to calculate VSLs outside the U.S., Viscusi and Masterman (2017) estimated country-specific VSLs by adjusting U.S. willingness to pay to account for income differentials.
In SSA, the Viscusi and Masterman (2017) VSLs range from $45,000 (Burundi) to $1.1 million (Botswana). These estimates do not reflect differences in the values of a human life in some moral sense, but rather the assumption that the poor derive greater utility from an incremental unit of income than the rich, and are therefore willing to give up less income for a given reduction in mortality risk. Although VSL calculations do not explicitly account for mortality from various sources, one might informally defend the lower monetary benefits per reduction in COVID mortality risk by observing that risk-reducing policies that also reduce income (e.g., lockdowns) may increase the risk of mortality from such poverty-related causes as malnutrition or preventable illness (Barnett-Howell and Mobarak 2020; Nachega et al. 2020). Combining the Walker et al. (2020) epidemiological estimates for developing country COVID-19 mortality with the lower VSLs of Viscusi and Masterman (2017), Barnett-Howell and Mobarak (2020) conclude that benefits of social distancing are likely to be quite low for lower-income countries in general.
Framing the benefits of COVID policy in terms of mortality reduction alone, however, potentially overlooks a primary motivation for government intervention–the existence of market failures. In theory, rational agents respond to the threat of infection by reducing interpersonal contacts (working, shopping, socializing less) and taking limited precautionary measures (e.g., washing hands more frequently). There is some empirical evidence supporting this voluntary avoidance behavior hypothesis in previous flu epidemics (Bayham et al. 2015). Pure epidemiological models do not account for such avoidance behavior, instead holding contact rate parameters exogenously fixed. As such, these models would overestimate infection and mortality effects of policy if people do behave rationally (Eichenbaum, Rebelo, and Trabandt 2020).
Voluntary avoidance behavior is too low from a social perspective, however. Rational individuals only internalize their own infection risk, not how their actions affect the risk of others in the community (Eichenbaum, Rebelo, and Trabandt 2020).10 This externality could justify some suppression of economic activity even if COVID-19 were nonfatal.
Suppose, for simplicity, that the only effect of COVID was to reduce available working hours for a fraction of the infected population. Rational workers and employers could be expected to adjust behavior to account for their own infection-related income loss, but not for that of other workers. The resulting equilibrium would be inefficient, i.e., the total welfare to employers and workers could be increased by restricting hours worked. Note that the restriction would have to be fewer hours than would be worked otherwise given the pandemic, not just fewer hours than would be worked in the absence of the pandemic.
In this nonfatal example, the tradeoff is not between income and COVID-19 deaths, but income lost due to work restrictions and income lost due to illness. In other words, such a policy may still be optimal in a developing country context with a low VSL in which the primary concern is avoiding poverty. This logic suggests that some sort of restrictive policy may be warranted in a developing country context, but does not indicate how much. To answer the latter question requires modeling. While it is beyond the scope of this article to conduct such an exercise, we can identify how the SIR models being used for US analysis might be modified for the SSA context and which data might be useful for calculating relevant parameters.
In principle, the parameters in the model should be adjusted for local population characteristics. Walker et al. (2020) calculate infection and fatality rates for 179 countries. Figure 4 illustrates examples of how factors specific to the African context may influence contract and recovery rates. In practice, data limitations pose a challenge to country-specific calibration.
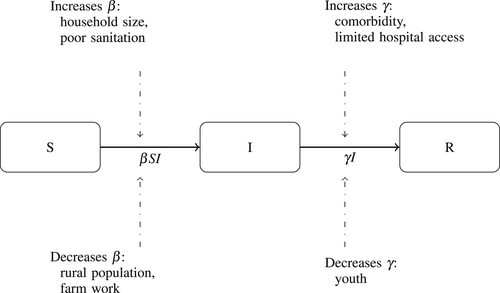
Source: Authors, adapted from Hethcote (2000).
SSA countries face a unique set of tradeoffs, as the factors conducive to transmission β and recovery γ in figure 4 differ from those in both high-income countries and other well-studied lower-income countries, such as China. The fact that SSA populations are younger suggests that the fatality risks associated with COVID-19 are likely to be lower than those experienced in higher-income countries (Figure A1). Yet, all SSA countries may face increased risk due to higher risks of contraction intergenerationally and existing comorbidities.11 Panel (b) of Figure A1 illustrates that most households in Africa have six or more members compared to 4% in the U.S. Moreover, countries like Botswana and Zambia have high incidences of HIV, and Mozambique high incidence of tuberculosis per 10,000 people (Table A1).
We could further tailor the calculation of the consequences of COVID-19 to a particular country in the SIR model, by allowing the cost-of-illness to vary by the structure of the economy. For example, in the absence of a policy, the productivity losses associated with infected cases may be relatively lower in Uganda and Mozambique than Botswana, as the majority of the workforce is engaged in low-value agriculture activities (Table A1). We can refine the total national losses of productivity to account for how workers are spread across sectors and the associated value of the output per worker (or wages earned) in each sector. After considering the structure of the economy, a policy that imposes mobility restrictions on a self-employed, agriculturally based economy may not be warranted due to the minimal monetary losses to production from COVID-19 infections, and given contraction rates are relatively lower in these work environments. Similarly, the ability for individuals to engage in defensive behavior such as rigorous hand washing may vary widely across the continent. Access to basic sanitation, for example, ranges from 26% (Uganda) to 89% (Botswana) of the urban population in our focal countries (Table A1.)12
A simple three-compartment SIR model can be useful for understanding overall dynamics of an epidemic and provide fairly realistic predictions for a homogeneous population, but may not have enough resolution when the population consists of communities with different socio-urban characteristics or demographics. Moving forward, these homogenized SIR models could be adapted to provide the foundation for metapopulation models that account for interconnected communities using separate sets of parameters which account for community-specific settings (Li et al. 2020). The challenges of having missing information about daily new infections and mortality counts are compounded by diverse models of social interaction across different communities and geographic separation of communities. Mobility patterns among communities are particularly crucial when trying to forecast the effects of different measures to contain and control the transmission of the virus. For example, the benefits of restricting the freedom of movement may be relatively small in countries with low internal migration rates, e.g. Burkina Faso, Kenya, and Zambia, but higher in countries like Botswana where migration is more prevalent (Table A1).
From the perspective of benefit–cost analysis, it is important to refine epidemiological and economic models to account for how policies may influence morbidity risks across different demographic groups and their short-term and long-term consequences on welfare. For example, the contact rate may differ by wealth, if enforcement of social distancing policies is more lenient in the informal sector where low- and middle-income individuals predominantly work. Another consideration is that limiting the participation of healthy workers in the agricultural sector during key periods of the agricultural cycle will not only affect the consumption of rural households, but the food supply available for urban consumers. Finally, promotion of more flexible health policies may allow impoverished households to gain income in the short term, yet jeopardize the long-term food security if a substantive portion of workers fall ill.
Future Research and Extensions
Resource-constrained governments face difficult choices regarding disease mitigation strategies and economic impacts. Although they have demonstrated an impressive level of responsiveness, cooperation, and adaptability to the pandemic, COVID-19 remains an uphill battle given limited resources, fragile health systems, existing disease burden, urban density, conflict, and record levels of population displacement. These unique social dynamics bring unique challenges to predictive modeling to guide the response. Much remains unknown about the trajectory of the transmission of COVID-19 in SSA. It is unclear how the youthful population and significant experience battling epidemics will offset the vulnerabilities due to poverty, weak health care infrastructure and crowded urban areas.
Future epidemiological-economic modeling for COVID-19 should consider country and regional vulnerabilities and how these vulnerabilities increase risk of disease transmission, while also considering that parameters for estimating the impact of various mitigation strategies are likely to be very different in SSA. In other words, it is essential to understand the epidemiological dynamics of COVID-19 within the local context. Recent epidemiology modeling efforts have made impressive efforts to adapt existing models and provide forecasting estimates for SSA (Achoki et al. 2020; Zahra Diop et al. 2020). However, these exercises are limited by the lack of availability of key epidemiological covariates. Researchers require access to unbiased data on testing, case counts and mortality to refine their predictions.13 Innovative strategies for improving data reporting systems could enable more accurate modeling projections to help mitigate the spread and mortality related to COVID-19.
On the economic side, future analyses should address distributional implications of COVID-19 policies. Wealthier individuals are likely to possess jobs with lower COVID-19 contact rates, may be better informed about mitigating behaviors, and have the means to invest in precautionary measures to mitigate risk. Moreover, the increasing burden of social distancing policies on women has become a growing concern among international stakeholders. Women face a disproportionate burden on their time, as schools are closed and family members get sick. Consequently, a greater percentage may be forced to reduce the number of hours they can work, or exit the labor force altogether, thus affecting their earnings.
Rapid response surveys are currently being administered over the phone by entities, such as the World Bank, to inform policy responses to the crisis. Accurate estimates of the cost of illness relies on collection of real-time information of changes in the behavior of men and women. For example, the duration of COVID-related illnesses is crucial to measuring the loss of labor. Documenting how women and men spend time on various activities during the crisis is instrumental in capturing not only the decline in labor supply among the infected, but also the time burden faced by family members as their productive labor is reallocated toward domestic tasks and care-giving. In addition to capturing changes in time use, wage information across sectors, and perhaps by gender, could serve as a proxy for the monetary value of those losses of labor. Although a more relevant metric among subsistence households, restrictions on survey time may preclude collecting the necessary production or profit information to estimate shadow wages of labor.
There are also two important features of benefit–cost analyses of COVID-19 policies that can be improved through ongoing data collection efforts. First, private adaptation to health risks is integral for establishing the costs of COVID-19 in the absence of any policy. Emerging data sources indicate that individuals may be changing an array of practices to avoid risk, such as increasing hand-washing and avoiding congested places (COVID-19 Tracker 2020). Second, measurement of spillover effects of policies may be necessary, out of concern that some may crowd-out investments in control of other illnesses. Collecting individual data on food security, consumption, and illness outcomes can be used to estimate these indirect policy effects in future benefit–cost analyses.
Finally, the dominant policies evaluated in the literature focus on reductions in contraction and fatality rates. We are learning from earlier outbreaks that the types of policies being implemented and their enforcement are quite decentralized. Future models can benefit from subnational data informing these policy parameters to determine whether policies are ineffective or suffer from a lack of enforcement. A second consideration for policy modeling relates to understanding what forms of subsidies may be required to compensate subsistence households for adhering to health campaigns. It may be optimistic to assume that low-income households will alter their behavior toward a socially optimal equilibrium, by refraining from work during temporary quarantines or staying at home when their private fatality and morbidity risk is minimal. For this reason, future evaluations should consider the benefits of bundling existing health policies with social protection programs as a way of subsidizing the costs of these behaviors that benefit society (Hidrobo et al. 2020).
Acknowledgements
This research benefited from the financial support of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R03HD098357) and the Bill and Melinda Gates Foundation (INV-017300). Corinna Keeler was supported in part by a training grant from the National Institute of Environmental Health Sciences (T32ES007018).
References
- 1 Although there is a distinction between the disease, COVID-19, and the virus which causes it, SARS-CoV-2, for ease of exposition we only use the term COVID-19.
- 2 Case and death data are reported between January 1, 2020 to June 1, 2020 (Hale et al. 2020b). Population data come from UN (2018).
- 3 The difference in mortality risk in Uganda relative to the other countries may be attributable to its experience with other epidemics (Ramamurti 2020). For example, there are several proactive measures, adopted by organizations like the Red Cross to combat Ebola, that are also effective responses to outbreaks of other viruses (Geiger, Harborth, and Mugyisha 2020).
- 4 For reference, the incident case rate in the United States over the same period was 5401.38 cases per million population (314.95 deaths per million), and across the 27 countries in the European Union was 2517.86 cases per million population (284.36 deaths per million).
- 5 The economic impacts of COVID-19 will extend along several dimensions. For example, remittances are expected to be affected by the recession, especially in Burkina Faso, Kenya, Mali, and Uganda where the share of remittances that comprises GDP is 3% or higher (World Bank 2020a). We do not elaborate on this point, as we lack monthly remittance data per country.
- 6 Epidemiological analysis on COVID-19 often includes a fourth compartment E, those who are exposed but not yet infected. The Susceptible-Exposed-Infected-Recovered (SEIR) analyzes the role of asymptomatic transmission in the spread of COVID and shows how more stringent policies may be essential to reduce the threat of COVID-19 even when cases are overtly low. For ease of exposition, we focus on the simpler SIR model as it lays the foundation for many current economic applications. The interested reader can refer to Ma (2020) for a discussion of the differences between the SIR and SEIR models.
- 7 A willingness to pay $10,000 for a 0.1% reduction in mortality risk, for example, would translate to a $10 million VSL.
- 8 The smoothing of the infection rate yields greater benefits in models that have nonlinear death rates, for example due to hospital capacity thresholds.
- 9 For analysis of the Clean Power Plan in 2020, for example, the EPA used a VSL of $9.9 million in 2011 dollars (https://19january2017snapshot.epa.gov/sites/production/files/2015-08/documents/cpp-final-rule-ria.pdf). This value is based on a central estimate of several economic studies, mostly based on analyzing how wage differentials for occupations varies by mortality risk. For greater detail see EPA (2014).
- 10 Altruism may also affect individual behavior, but this type of preference structure is largely ignored in economic models of pandemic policy response.
- 11 Recent work suggests more complex roles for location-specific factors in elevating COVID-19 risk. Household size or family connections can increase the magnitude of secondary infections in absence of a quarantine. For example, a contract-tracing exercise in Iceland noted that the highest source of exposure was from one's family rather than from social activities, tourism, work, or travel (Gudbjartsson et al. 2020). The density of the individual's location also is crucial in the risk of contracting the virus, as urban locations expose residents to more people in confined locations over time (Zahra Diop et al. 2020).
- 12 The examples provided here are not exhaustive of how the parameters of a SIR model may vary by context. An important factor to consider when measuring the impacts of policy is the consequences on agricultural production and food security. We turn to this topic shortly.
- 13 At this stage, it is difficult to evaluate how epidemiological data collected in Africa might be biased. As discussed by Roser et al. (2020), the reliability of epidemiological data has been measured by the “positive rate”: the number of confirmed cases divided by the number of tests performed. A rate between 3 and 10% for a particular country suggests that the country is conducting an adequate number of tests relative to the scale of its outbreak. Unfortunately, there is insufficient information on the positive rate for the eight countries in our study. As of June 1, 2020, only one positive rate was reported (Kenya, 4.1%).