Journal list menu
Export Citations
Download PDFs
ISSUE INFORMATION
ORIGINAL ARTICLES
Surgical outcomes of laparoscopic versus open repeat liver resection for liver cancers: A report from a nationwide surgical database in Japan
- Pages: 833-842
- First Published: 20 April 2022
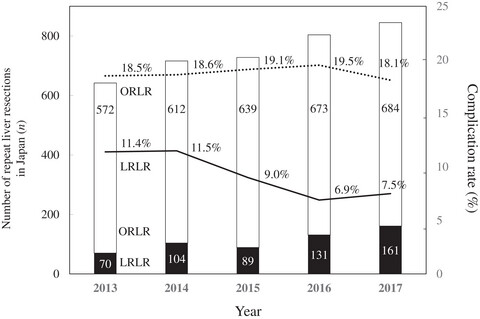
Postoperative grade II or higher Clavien-Dindo classification complication rates were significantly lower in the laparoscopic vs open repeat liver resection group, with shorter operative time, less intraoperative bleeding, and lower intraoperative transfusion rate. Kaibori et al conclude that laparoscopic repeat liver resection is a safer and more effective liver cancer treatment.
An international multicenter propensity-score matched and coarsened-exact matched analysis comparing robotic versus laparoscopic partial liver resections of the anterolateral segments
- Pages: 843-854
- First Published: 07 April 2022
This international combined propensity score-matched and coarsened exact-matched study by Kadam et al showed equivalent perioperative outcomes of robotic and laparoscopic liver resection in selected patients at high-volume centers. The robotic approach was associated with significantly lower blood loss and allowed more surgeries to be completed in a minimally invasive fashion.
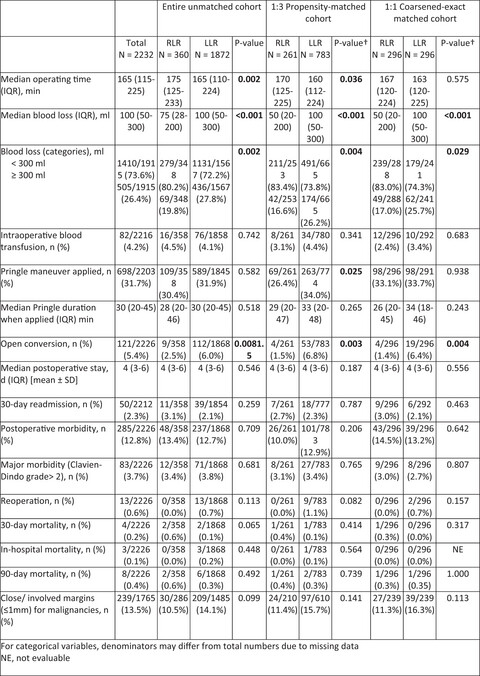
Association between achieving textbook outcomes and better survival after laparoscopic liver resection in the anterolateral segments in patients with hepatocellular carcinoma
- Pages: 855-862
- First Published: 07 April 2022
Textbook outcomes, used to assess the quality of surgical procedures, were achieved in 55.0% of patients who underwent laparoscopic liver resection in the anterolateral segments. D’Silva et al conclude that achievement of a textbook outcome positively affects short- and long-term recurrence and survival after laparoscopic liver resection for hepatocellular carcinoma.
The impact of pylorus preservation on the development of nonalcoholic fatty liver disease after pancreaticoduodenectomy: A historical cohort study
- Pages: 863-873
- First Published: 18 April 2022
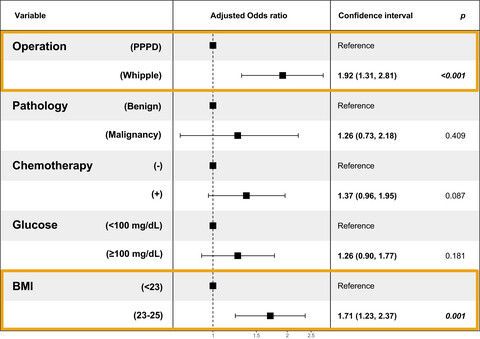
One of the postoperative complications after pancreaticoduodenectomy is de novo development of non-alcoholic fatty liver disease. In this large cohort study of 786 patients, Jeon et al found high preoperative body mass index and Whipple's operation, as opposed to pylorus-preserving pancreaticoduodenectomy, to be associated with newly developed non-alcoholic fatty liver disease.
Extended criteria donors for robotic right hepatectomy: A propensity score matched analysis
- Pages: 874-883
- First Published: 11 April 2022
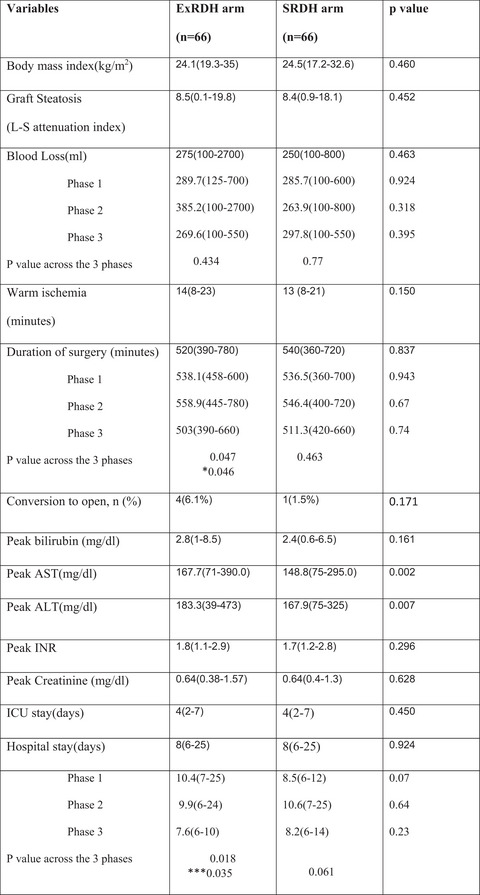
Varghese et al compared robotic right donor hepatectomy in 100 extended criteria donors (graft weighing 800 g or more with or without complex biliovascular anatomy) with that in 70 standard criteria donors, using a propensity score-matched analysis. Once the learning curve was traversed, the perioperative outcomes were similar in both groups.
Steroid therapy still plays a crucial role and could serve as a bridge to the next promising treatments in patients with IgG4-related sclerosing cholangitis: Results of a Japanese nationwide study
- Pages: 884-897
- First Published: 22 April 2022
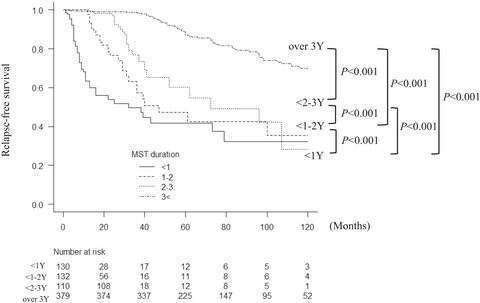
The acceptable duration of steroid therapy for IgG4-sclerosing cholangitis remains debated. Kubota et al conclude that steroid therapy should be continued at least 3 years to reduce the risk of relapse, with preemptive measures taken around 5 years. Steroids as first-line therapy could serve as a bridge to further promising treatments.
Clinical outcomes of organ-preserving pancreatectomy for benign or low-grade malignant pancreatic tumors: A multicenter nationwide survey in Japan
- Pages: 898-910
- First Published: 19 April 2022
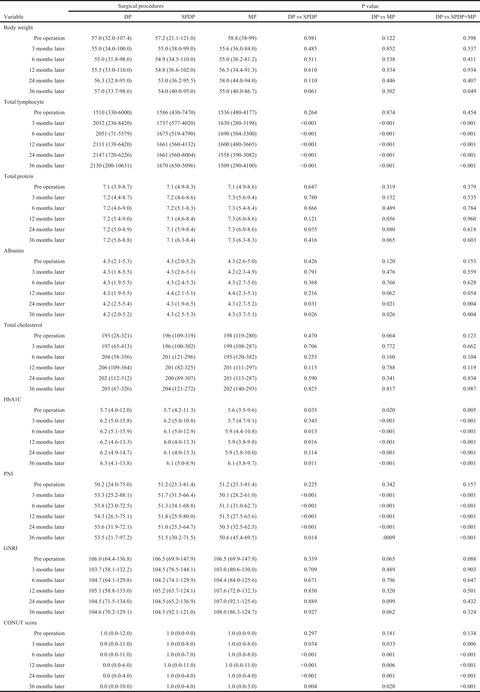
Asano et al investigated the clinical benefits of organ-preserving pancreatectomy using a Japanese multicenter nationwide survey. Middle pancreatectomy may contribute to improving postoperative quality of life in patients with low-grade malignancies of the body of the pancreas, compared with pancreaticoduodenectomy or distal pancreatectomy, but short-term complications remain a challenge.
Prognosis following an extended duration of adjuvant gemcitabine plus S-1 chemotherapy in patients with pancreatic ductal adenocarcinoma: Analysis using inverse probability of treatment weighting
- Pages: 911-921
- First Published: 18 April 2022
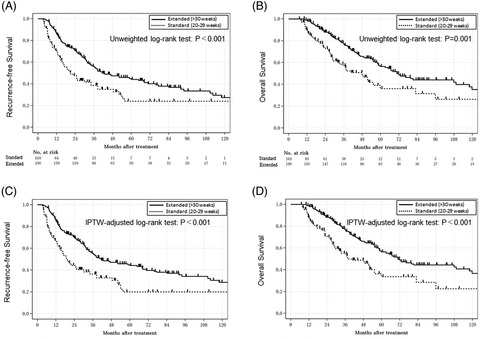
Kondo et al assessed 290 eligible patients with pancreatic ductal adenocarcinoma who received adjuvant gemcitabine plus S-1 chemotherapy for the standard duration of 20-29 weeks or an extended duration of ≥30 weeks. The extended duration significantly correlated with prolonged recurrence-free and overall survival after inverse probability of treatment weighting adjustment.
The prognostic impact of ABO blood type in pancreatic cancer: Relevance to adjuvant chemotherapy
- Pages: 922-931
- First Published: 18 April 2022
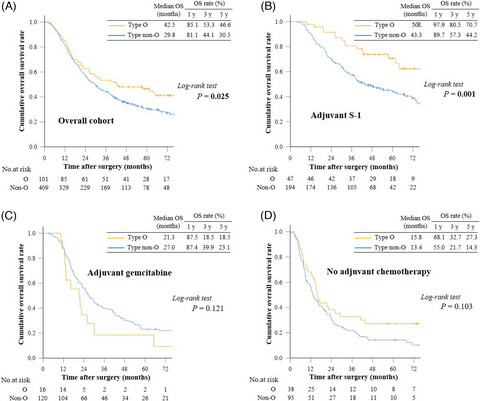
Tezuka et al revealed that blood type O was an independent favorable prognostic factor for overall survival in patients with resected pancreatic cancer treated with adjuvant S-1. The ABO blood type is a potential and readily available predictive biomarker of benefit from adjuvant treatment with S-1 in pancreatic cancer.
Efficacy of endoscopic large balloon dilation extended for 2 minutes in bile duct stone removal: A multicenter retrospective study
- Pages: 932-940
- First Published: 30 July 2021
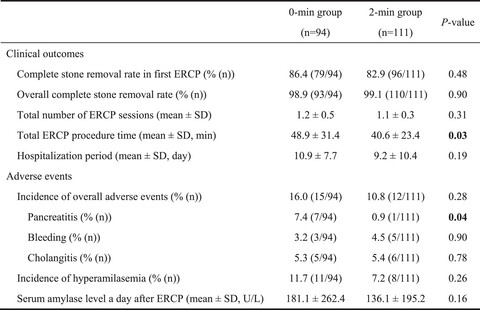
Nakahara et al evaluated the efficacy of a 2-minute extension of the dilation time during endoscopic papillary large balloon dilation for bile duct stone removal. Extension of the balloon dilation for 2 minutes after waist disappearance could help prevent post-endoscopic retrograde cholangiopancreatography pancreatitis and shorten the overall procedure time.
Single session endoscopic ultrasound-guided double bypass (hepaticogastrostomy and gastrojejunostomy) for concomitant duodenal and biliary obstruction: A case series
- Pages: 941-949
- First Published: 07 October 2021

Canakis et al describe the technical feasibility, safety, and clinical success of single-session endoscopic ultrasound-guided double bypass in patients with concomitant biliary and gastric obstruction. The durability of stent patency and decreased length of hospital stay may lead to increased use of this approach, especially in patients with end-stage malignancy.
Detection rate of endoscopic ultrasound and computed tomography in diagnosing pancreatic neuroendocrine neoplasms including small lesions: A multicenter study
- Pages: 950-959
- First Published: 01 April 2022
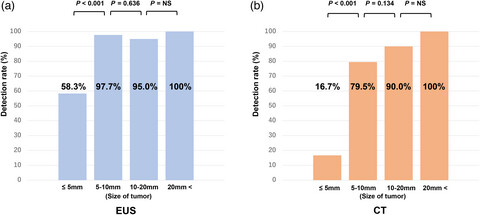
Kurita et al found that endoscopic ultrasound had the best detection ability among imaging modalities for pancreatic neuroendocrine neoplasms. It may be desirable to detect and identify lesions suitable for treatment using computed tomography, and then accurately locate and diagnose pancreatic neuroendocrine neoplasms using endoscopic ultrasound before treatment, including surgery.
HOW I DO IT (ONLINE ONLY)
Laparoscopic intragastric approach to transgastric necrosectomy
- Pages: e75-e76
- First Published: 02 December 2021
Vellalta et al demonstrate how severe necrotizing pancreatitis complicated with extensive infected necrosis is successfully treated with transgastric laparoscopic necrosectomy. Furthermore, through the use of three intragastric trocars, the contributed approach provides excellent access and improved vision of the necrosis cavity, avoiding the need for wide anterior gastrotomy.
Transferring a naso-gallbladder drainage tube to the mouth for re-examination of a gallbladder lesion
- Pages: e77-e78
- First Published: 06 April 2022
Conventional gallbladder re-intervention along the naso-gallbladder drainage tube may result in dislocation of the tube during scope insertion or failure of guidewire insertion into the gallbladder. Mandai et al report a simple method for transferring a transpapillary naso-gallbladder drainage tube to the mouth that facilitates reliable re-intervention for gallbladder lesions.
CASE IMAGE (ONLINE ONLY)
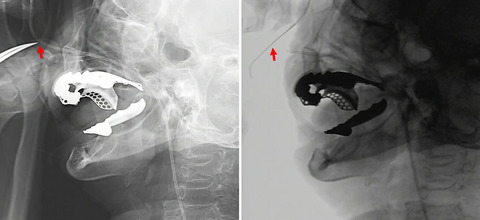
Operative findings of the migrated stent into the abdominal cavity following endoscopic ultrasound-guided hepaticogastrostomy: Anchoring force of a novel self-expandable metal stent with an anti-migration system (with video)
- Pages: e79-e80
- First Published: 10 January 2022
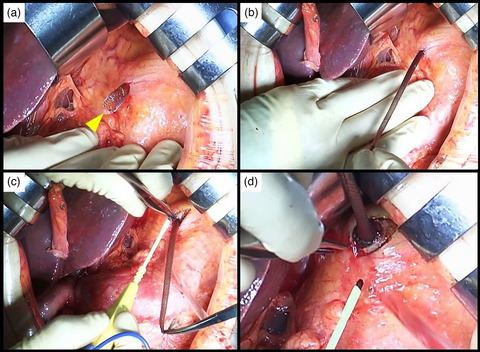
Koga et al report an emergency surgery for stent migration during endoscopic ultrasound-guided hepaticogastrostomy, which revealed the strong anchoring force of a stent with a spring-type stopper as an anti-migration system at the proximal end. The stent could not be pulled out of the stomach wall and was removed via gastrotomy.