Randomized-controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy among distressed breast cancer survivors (MINDSET): long-term follow-up results
Abstract
Background
Mindfulness-based cancer recovery (MBCR) and supportive expressive group therapy (SET) are two well-validated psychosocial interventions, but they have not been directly compared, and little is known about long-term outcomes. This comparative effectiveness study measured the effects of these two interventions immediately following the groups and for 1 year thereafter in distressed breast cancer survivors.
Methods
Two hundred fifty-two distressed Stage I–III breast cancer survivors were randomized into either MBCR or SET. Women completed questionnaires addressing mood, stress symptoms, quality of life, social support, spirituality and post-traumatic growth before and after the interventions, and 6 and 12 months later.
Results
Immediately following the intervention, women in MBCR reported greater reduction in mood disturbance (primarily fatigue, anxiety and confusion) and stress symptoms including tension, sympathetic arousal and cognitive symptoms than those in SET. They also reported increased emotional and functional quality of life, emotional, affective and positive social support, spirituality (feelings of peace and meaning in life) and post-traumatic growth (appreciation for life and ability to see new possibilities) relative to those in SET, who also improved to a lesser degree on many outcomes. Effect sizes of the time × group interactions were small to medium, and most benefits were maintained over 12 months of follow-up.
Conclusions
This study is the first and largest to demonstrate sustained benefits of MBCR in distressed breast cancer survivors relative to an active control. MBCR was superior to SET for improving psychological well-being with lasting benefits over 1 year, suggesting these women gained long-lasting and efficacious tools to cope with cancer.
Trial Registration
Registered on clinicaltrials.gov number NCT00390169, October 2006. Copyright © 2016 John Wiley & Sons, Ltd.
Introduction
While there has been a great deal of research interest in the acute effects of mindfulness-based interventions (MBIs) such as mindfulness-based stress reduction (MBSR) 1 and our adaptation, mindfulness-based cancer recovery (MBCR) 2, within cancer care, and many studies show benefits for breast cancer survivors 3-9, few studies have investigated the longer term effects of such programmes. We were the first to evaluate 6-month and 12-month follow-up data of MBCR participants, showing long-term maintenance in stress reduction and improved mood 10, 11, but without comparison to control conditions. Hence, whether improvements in these outcomes would have occurred even without the intervention was not clear. One large trial of 336 women with breast cancer randomized to MBSR or usual care reported improvements in anxiety and depression that were maintained over a year of follow-up with medium to large effects 12, demonstrating specific value compared with the usual pattern of recovery from breast cancer treatment. In the same sample, however, while MBSR compared with control resulted in more sleep improvements immediately post-programme, after a year, there were no group differences on sleep measures 13.
Only one study has looked at long-term follow-up comparing an MBI to an active control group. Henderson et al. 14 randomized 172 early stage breast cancer patients into MBSR, a nutrition education programme matched on contact time, or a usual care control condition, and included follow-up assessments post programme, 1 and 2 years later. The MBSR group improved more than usual care on 9 of 13 measures and the active control on 8 of 13 measures immediately post-programme. However, these differences eroded over time as participants in the other two groups continued to improve more slowly while MBSR improvements declined on some measures, so that by 12 months, MBSR was superior to nutrition on only one measure, and usual care on only two. By 24 months, MBSR participants were no different from those in nutrition education, but better than usual care on three measures. Hence, the question remains as to whether MBIs are really better over the long term than other psychosocial interventions for reducing psychological symptoms in breast cancer survivors.
We published in 2013 primary results of the MINDSET study showing greater benefit pre-intervention to post-intervention for MBCR over SET and a control condition on outcomes of stress, social support and quality of life 15. We also tracked outcomes over a full year in both active intervention groups, and in addition, those women in the original control condition were re-randomized to one of the two active interventions and also followed for a year. Hence, in this report, we examined the long-term effects (6 months, 1 year) of MBCR compared with SET including those controls re-randomized to each intervention, on psychological parameters.
Objectives were to determine whether benefits obtained initially after programme completion would be maintained over the course of a full year in MBCR compared with SET, or whether group differences would erode over time, which could happen through slower improvements in SET allowing that group to catch up, or loss of benefits over time in MBCR. We also assessed a broader range of outcome measures looking at both psychological symptomatology (mood disturbance and symptoms of stress) and potential delayed effects of programme participation on positive outcomes including spirituality and post-traumatic growth (PTG).
Spirituality is often defined as having a sense of meaning and purpose in life, a sense of community and connection with others, strength and comfort from one's faith, and an overall feeling of harmony and peace 16, 17. PTG, a similar concept but tied specifically to the context of experiencing a traumatic or life-threatening event, is defined as the collective positive benefits of the cancer diagnosis and experience, and the life changes that follow 18, 19. In some studies, development of PTG and spirituality has been related to improvements in long-term psychosocial adjustment 20-23, and in our previous work, we found enhanced PTG and spirituality after participation in MBCR groups 24, 25, but the extent of this over time and within various sub-dimensions of the constructs has not been investigated. Hence, the objectives of this study were to compare effects of MBSR and SET over 1-year post-treatment in distressed breast cancer survivors on measures of mood, stress, social support, quality of life, spirituality and PTG, as well as on the subscales of each of these measures.
Methods
Study design
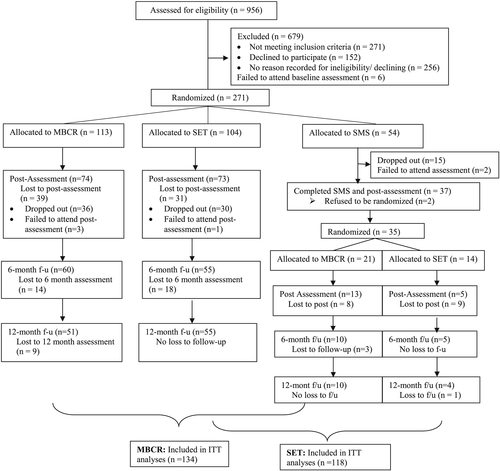
The larger study used a multicentre longitudinal randomized controlled design with three groups: MBCR, SET and a minimal control condition of a 1-day stress management seminar. Participants were initially randomized into one of the three groups with a 2:2:1 allocation ratio, in cohorts up to 30 women at two study cites, Calgary and Vancouver. After the initial intervention period of 12 weeks, women in the control condition were then re-randomized into either MBCR or SET and joined the next session of these groups. All participants in MBCR and SET completed a set of questionnaires before and after the intervention, and 6 and 12 months later (see Figure 1 for study schematic). The details and pre–post primary outcomes of the 3-arm MINDSET study were reported previously 15; this is a follow-up analysis to examine the long-term effects of MBCR and SET on a larger set of outcomes. Ethical approval was obtained from the respective institutional review boards at each study site, and written informed consent was obtained from participants.
Inclusion/Exclusion criteria
- Inclusion Criteria: (1) Women Diagnosed with Stage I, II or III Breast cancer, (2) Completion of all treatments with the exception of hormonal or Herceptin therapy at least 3 months previously, (3) Over age 18, (4) Score of 4 or higher on the Distress Thermometer 26, to ensure a sample who were experiencing clinically meaningful distress 27.
- Exclusion criteria: (1) Concurrent DSM-IV Axis I diagnosis of psychosis, substance abuse, bipolar disorder or active suicidality. Depression, anxiety disorders and adjustment disorders were not excluded. (2) Current use of psychotropic medications (antipsychotics, anxiolytics). Use of antidepressants was recorded but not an exclusionary factor (due to their high prevalence of use). (3) Concurrent autoimmune disorder, (4) Past participation in an MBCR or SET group.
Procedures
Interested participants were phone screened for eligibility. If eligible, they were scheduled for an interview to receive more information and provide informed consent. This was followed by completion of a baseline questionnaire. Each intervention commenced within 2 weeks following randomization. Participants completed another set of questionnaires immediately following the intervention (or at 12 weeks for control participants). This 12-week assessment was considered the ‘baseline’ measure for controls who were then re-randomized into either MBCR or SET, and then reassessed post-programme, 6 and 12 months thereafter.
Randomization and blinding
Once each cohort was assembled and baseline data collected, women were randomly assigned using the Research Randomizer website (http://www.randomizer.org/) 2:2:1 by the statistician to MBCR, SET or control. Women who were initially in control were later randomized 1:1 into either MBCR or SET using the same protocol. At the time of initial assessment, participants as well as RAs were blind to condition.
Interventions
Mindfulness-based cancer recovery
Mindfulness-based cancer recovery has its roots in contemplative spiritual traditions, in which mindfulness, conscious awareness in the present moment in an open and non-judgmental manner, is actively cultivated though training in mindfulness meditation and gentle yoga practices 1. The intervention was modelled on the MBSR programme developed at the Massachusetts Medical Centre 1, modified by Carlson and Speca as MBCR 2 and validated in a series of previous studies (see 28; 8 for a review). The programme consisted of eight weekly group sessions of 90 min each plus a 6-hour workshop between weeks 6 and 7 for a total of 18 contact hours.
Supportive expressive therapy
The SET group was based on a manualized treatment developed by the Psychosocial Treatment Laboratory's Breast Cancer Intervention Program at Stanford University 29. The goals of the therapy include facilitating mutual support and family support, enhancing openness and emotional expressiveness, improving coping skills and doctor–patient relationships, and detoxifying feelings around death and dying. The programme consisted of 12 weekly group sessions of 90 min each and equal contact hours to MBCR.
Measures
Background measures
Demographic characteristics including age, socioeconomic status, medical history, psychiatric history and current medications, and previous experience with yoga or meditation were assessed. Participants were also asked about recent health behaviour, such as alcohol and nicotine intake, quality of sleep and diet. Disease parameters of stage of disease and date of diagnosis at the time of study enrollment were collected through chart reviews.
Primary outcome measure
Mood: The Profile of Mood States (POMS) 30 was used to assess six dimensions of mood: anxiety, depression, anger, vigor, fatigue and confusion, which were summed to generate a Total Mood Disturbance score. The POMS has been widely used in clinical populations, including cancer patients. In our previous report, we included only the Total Mood Disturbance score; here, we examine each of the subscales as well to determine the relative magnitude of changes.
Stress symptoms: The 56-item short form of the Symptoms of Stress Inventory (SOSI) 31, the Calgary (C)-SOSI 32 was used to measure Physical, Psychological and Behavioural Responses to Stressful Situations. There are eight subscales entitled Depression, Anger, Muscle Tension, Sympathetic Arousal, Cardiopulmonary Arousal, Cognitive Disorganization, Neurological/GI and Upper Respiratory. A total stress symptom score was also calculated by summing all the items. As with the POMS, in this analysis, we investigated the magnitude of changes on each of the subscales as well as the total score.
Secondary outcome measures
Quality of life: The Functional Assessment of Cancer Therapy-Breast (FACT-B) module 33 was used. The scale consists of the FACT-General 34, a general cancer quality of life measure and the Breast Cancer Subscale with items specific to well-being of breast cancer patients. Subscales include Physical Well-Being, Social Well-Being, Emotional Well-Being, Functional Well-Being and a Breast Cancer Symptom subscale, as well as the Total QL score.
Social support: The Medical Outcomes Study Social Support Survey (MOS-SSS) 35 was used to measure social support. The scale consists of 19 items and addresses four dimensions of perceived social support: Tangible Support, Affectionate Support, Positive Social Interaction, and Emotional or Informational Support. The total support score as well as subscale scores were assessed.
Spiritual well-being: The Functional Assessment of Chronic Illness therapy-Spiritual Well-being (FACIT-Sp) scale 17 was used to measure spiritual well-being. The FACIT-Sp is a 12-item questionnaire designed for people with cancer or other chronic illnesses. Subscales include Meaning, Peace and Faith, which can be summed to a Total Score.
Post-traumatic growth: The 21-item PTG Inventory-Revised (PTGI-R) 36 was used to measure an individual's perception of positive changes following a traumatic life experience. Subscales include Relating to Others, New Possibilities, Personal Strength, Spiritual Change and Appreciation of Life, which are summed to form the Total Score.
Data analysis
Descriptive statistics were used to examine demographics and medical information at baseline between intervention groups. Two-level piecewise hierarchical linear modelling (HLM) with random intercepts was conducted to analyse the differences in the rates of changes of the primary outcomes (POMS and C-SOSI) as well as the secondary outcomes (FACT-B, MOS-SSS, FACIT-Sp and PTGI-R) and their subscales between the two intervention groups during two periods (i.e. pre-intervention to post-intervention and post-intervention to follow-up). Because of the high attrition rate, intent-to-treat principles were applied for the trajectory analyses. HLM is a desirable approach as all available data at each time point is used in the analyses. At level 1, to model the within-individual variation, we generated two variables representing two segments of study time: the first segment represented the pre–post intervention period, the second segment represented post-intervention to 12 months. At level 2, we modelled the growth parameters using group as a predictor (0.5 for MBCR, −0.5 for SET). All missing values were assumed as missing at random. sas 9.3 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses. PROC MIXED procedures were used to fit the two-level piecewise HLM, using maximum likelihood estimation to produce unbiased estimates. Two-sided statistical tests were used with α < 0.05. To assess the magnitude of the intervention effect using the time × group interaction, we calculated effect sizes
 (analogue Cohen's d: 0.2 small, 0.5 moderate, 0.8 large 37).
(analogue Cohen's d: 0.2 small, 0.5 moderate, 0.8 large 37).
Results
Figure 1 shows participant flow throughout the study. Adding in those from the control group who were re-randomized to either active interventions following their ‘post-control’ assessment, a total of 252 women were randomized into either MBCR (n = 134; 113 + 21) or SET (n = 118; 104 + 14). Of them, 165 women completed their pre-intervention and post-intervention assessment (MBCR: 74 + 13 = 87; SET: 73 + 5 = 78), 65% of the original sample. At 6 months, 130 women completed the follow-up assessment (51.5%), and 128 women completed the 12-month follow-up assessment (50.8%). Table 1 summarizes demographic and medical characteristics. The two groups (those with complete data versus dropouts) were not different on any demographic or outcome variables at baseline (data not shown). Women in the full sample allocated to either MBCR or SET were not different on any demographic variables, but women in SET had significantly higher baseline scores on symptoms of stress (depression, anger and upper respiratory symptoms), and lower scores on meaning and peace on the FACIT-Sp as well as lower personal strength and appreciation for life subscales of the PTGI.
| Characteristic | MBCR | SET | p-value |
|---|---|---|---|
| (n = 134) | (n = 118) | ||
| Age (years) Mean (SD) | 55.12 (9.84) | 54.14 (10.23) | 0.44 |
| Months since diagnosis Median (range) | 19.12 (2.96–171.10) | 18.99 (6.18–135.72) | 0.81 |
| Marital status n (%) | |||
| Single | 20 (14.9) | 17 (14.4) | 0.41 |
| Cohabiting/Married | 81 (60.4) | 75 (63.6) | |
| Divorced/Separated/Widowed | 29 (21.6) | 18 (15.3) | |
| Unknown | 4 (3.0) | 8 (6.8) | |
| Employment status n (%) | |||
| Unemployed/Retired/Disabled | 54 (40.3) | 46 (39.0) | 0.57 |
| Part-time | 26 (19.4) | 28 (23.7) | |
| Full-time | 51 (38.1) | 38 (32.2) | |
| Unknown | 3 (2.2) | 6 (5.1) | |
| Highest education n (%) | |||
| Primary/Secondary/High school/GED | 21 (15.7) | 14 (11.9) | 0.92 |
| Some university/College/Technical school | 58 (43.3) | 54 (45.8) | |
| University degree | 41 (30.6) | 35 (29.7) | |
| Post-graduate/Masters/Doctorate degree | 12 (9.0) | 12 (10.2) | |
| Unknown | 2 (1.5) | 3 (2.5) | |
| Stage of cancer n (%) | |||
| 0 | 5 (3.7) | 2 (1.7) | 0.82 |
| I | 56 (41.8) | 49 (41.5) | |
| II | 51 (38.1) | 42 (35.6) | |
| III | 17 (12.7) | 16 (13.6) | |
| IV | 1 (0.7) | 2 (1.7) | |
| Unknown | 4 (3.0) | 7 (5.9) | |
| POMS Mean (SD) | |||
| Anxiety | 11.66 (6.68) | 12.87 (7.85) | 0.19 |
| Depression | 10.62 (10.35) | 12.36 (11.59) | 0.22 |
| Anger | 6.77 (6.41) | 8.37 (8.47) | 0.10 |
| Vigor | 13.7 (6.38) | 13.42 (6.76) | 0.74 |
| Fatigue | 10.88 (7.33) | 11.10 (7.28) | 0.81 |
| Confusion | 8.45 (5.36) | 9.63 (5.59) | 0.09 |
| Total mood disturbance | 34.68 (33.99) | 40.54 (39.85) | 0.21 |
| C-SOSI Mean (SD) | |||
| Depression | 7.32 (5.99) | 9.02 (6.58) | 0.03 |
| Anger | 7.24 (4.66) | 8.86 (5.52) | 0.01 |
| Muscle tension | 12.39 (7.32) | 13.98 (8.12) | 0.11 |
| Cardiopulmonary arousal | 3.85 (4.67) | 4.51 (4.89) | 0.28 |
| Sympathetic arousal | 16.97 (8.18) | 17.89 (7.54) | 0.36 |
| Cognitive disorganization | 7.15 (4.42) | 7.47 (4.33) | 0.58 |
| Neurological/GI | 4.23 (4.52) | 4.77 (4.30) | 0.34 |
| Upper respiratory symptoms | 4.71 (4.42) | 6.19 (4.90) | 0.02 |
| Total | 63.85 (29.01) | 72.90 (33.06) | 0.02 |
| FACT-B Mean (SD) | |||
| PWB | 21.10 (5.32) | 19.99 (5.28) | 0.10 |
| SWB | 18.56 (6.07) | 18.36 (5.67) | 0.79 |
| EWB | 16.95 (4.42) | 15.92 (4.59) | 0.08 |
| FWB | 17.93 (5.11) | 16.63 (5.61) | 0.06 |
| BCS | 22.29 (6.29) | 21.67 (5.65) | 0.42 |
| Total | 96.72 (20.92) | 92.42 (19.77) | 0.10 |
| MOS-SSS Mean (SD) | |||
| Tangible | 61.53 (28.58) | 64.20 (26.74) | 0.45 |
| Affectionate | 71.56 (27.81) | 74.27 (27.48) | 0.45 |
| Positive social interaction | 66.83 (24.37) | 68.38 (22.97) | 0.61 |
| Emotional and informational | 67.02 (24.15) | 68.53 (20.69) | 0.60 |
| Total | 66.41 (22.46) | 68.23 (21.11) | 0.52 |
| FACIT-Sp Mean (SD) | |||
| Meaning | 12.79 (2.91) | 11.76 (3.58) | 0.01 |
| Peace | 8.98 (3.40) | 8.04 (3.75) | 0.04 |
| Faith | 8.32 (4.86) | 7.78 (5.08) | 0.40 |
| Total | 30.04 (8.44) | 27.58 (10.36) | 0.04 |
| PTGI-R Mean (SD) | |||
| Relating to others | 21.39 (7.06) | 21.50 (7.41) | 0.91 |
| New possibilities | 12.16 (5.57) | 11.65 (6.07) | 0.49 |
| Personal strength | 11.86 (4.05) | 10.74 (4.68) | 0.05 |
| Spiritual change | 4.49 (3.27) | 3.97 (3.14) | 0.22 |
| Appreciation of life | 10.76 (2.96) | 9.68 (3.41) | 0.01 |
| Total | 60.74 (18.05) | 57.69 (20.79) | 0.22 |
- PWB, Physical well-being; SWB, Social well-being; EWB, Emotional well-being; FWB, Functional well-being; BCS, Breast cancer Symptom Scale; MBCR, mindfulness-based cancer recovery; SET, supportive expressive group therapy ; POMS, Profile of Mood States; C-SOSI, Calgary Symptoms of Stress Inventory; FACT-B, Functional Assessment of Cancer Therapy-Breast; MOS-SSS, Medical Outcomes Study Social Support Survey; FACIT-Sp, Functional Assessment of Chronic Illness therapy-Spirituality; PTGI-R, post-traumatic growth Inventory-Revised; GED, General Educational Diploma.
Primary outcomes
Profile of Mood States: The fixed effects of the HLM models are presented in Table 2. At baseline, no statistically significant differences on any of the subscales or total POMS score between groups were found. There was a statistically significant decrease for every subscale from pre-intervention to post-intervention favouring MBSR over SET (p = 0.001–0.03), as well as a main effect of time during the intervention period across both groups (all p < 0.0001). Between group effect sizes were in the small to medium range (d = 0.3–0.4). The largest slope differences between groups were on the subscales of Fatigue, Anxiety and Confusion. Over the follow-up period, all slopes were maintained from post-intervention (Supplementary Figure S1a–d).
| Outcomes | Intervention | Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Group × Time | Group × Time | ||||||||
| Est | se | t | p | d [CI] | Est | se | t | p | |
| POMS | |||||||||
| Anxiety | −1.23 | 0.46 | −3.02 | 0.003 | −0.39 [−0.64;−0.14] | 0.04 | 0.08 | 0.48 | 0.63 |
| Depression | −1.58 | 0.59 | −2.72 | 0.01 | −0.33 [−0.58;−0.08] | 0.10 | 0.12 | 0.86 | 0.39 |
| Anger | −1.13 | 0.44 | −2.62 | 0.01 | −0.35 [−0.60;−0.10] | 0.13 | 0.13 | 1.56 | 0.12 |
| Vigor | 0.88 | 0.41 | 2.14 | 0.03 | 0.30 [0.05;0.55] | 0.01 | 0.08 | 0.14 | 0.89 |
| Fatigue | −1.44 | 0.42 | −3.45 | 0.001 | −0.45 [−0.70;−0.20] | −0.03 | 0.08 | −0.30 | 0.76 |
| Confusion | −0.95 | 0.30 | −3.13 | 0.0002 | −0.39 [−0.64;−0.14] | 0.02 | 0.06 | 0.26 | 0.79 |
| TMD | −6.29 | 1.80 | −3.49 | 0.001 | −0.39 [−0.64;−0.14] | −0.06 | 0.31 | −0.19 | 0.85 |
| C-SOSI | |||||||||
| Depression | −0.87 | 0.36 | −2.41 | 0.02 | −0.31 [−0.56;−0.06] | 0.01 | 0.07 | 0.13 | 0.90 |
| Anger | −0.57 | 0.31 | −1.77 | 0.08 | −0.25 [−0.50;−0.001] | 0.07 | 0.06 | 1.08 | 0.28 |
| Muscle tension | −1.43 | 0.42 | −3.35 | 0.001 | −0.42 [−0.67;−0.17] | 0.02 | 0.09 | 0.26 | 0.80 |
| CA | −0.24 | 0.28 | −0.88 | 0.38 | −0.11 [−0.36;0.14] | −0.05 | 0.05 | −0.86 | 0.39 |
| SA | −1.31 | 0.41 | −3.17 | 0.002 | −0.38 [−0.63;−0.13] | 0.13 | 0.08 | 1.53 | 0.13 |
| CD | −0.66 | 0.24 | −2.79 | 0.006 | −0.35 [−0.60;−0.10] | 0.02 | 0.04 | 0.44 | 0.66 |
| Neu/GI | −0.71 | 0.26 | −2.76 | 0.006 | −0.36 [−0.61;−0.11] | 0.11 | 0.04 | 2.38 | 0.02 |
| URS | 0.15 | 0.34 | 0.44 | 0.66 | 0.07 [−0.18;0.32] | −0.04 | 0.07 | −0.62 | 0.54 |
| Total | −5.51 | 1.46 | −3.76 | 0.0004 | −0.40 [−0.65;−0.15] | 0.01 | 0.26 | 0.03 | 0.98 |
- TMD, Total mood disturbance; CA, Cardiopulmonary arousal; SA, Sympathetic arousal; CD, Cognitive disorganization; Neu/GI, Neurological/GI; URS, Upper respiratory symptom; POMS, Profile of Mood States; C-SOSI, Calgary Symptoms of Stress Inventory.
Calgary Symptoms of Stress Inventory: At baseline, Depression, Anger and Upper Respiratory subscales and the C-SOSI Total in the SET group were significantly higher than for the MBSR group. There was a statistically significant decrease on all subscales (p = 0.0004–0.02) except Cardiopulmonary Arousal and Upper Respiratory Symptoms from pre-programme to post-programme favouring MBCR, with medium effect sizes (Table 2). The only further changes from post-intervention over follow-up were slight increases in Depression scores across both groups (p = 0.04), and an erosion of group differences of slope in Neurological/GI symptoms (p = 0.02) favouring the SET group (Supplementary Figure S2a–f).
Secondary outcomes
Quality of Life: On the FACT-B, there were no significant differences between groups on any subscales and FACT-B total at baseline. While there were significant main effects of time during intervention period across all subscales (all p < 0.0001 except Social well-being p = 0.003), group differences of slopes favouring MBCR were also seen on Emotional and Functional Well-Being as well as the Total Score, with small effect sizes (Table 3). Over follow-up, only Functional well-being showed significant continual improvement (p = 0.01) across both groups.
| Outcomes | Intervention | Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Group × Time | Group × Time | ||||||||
| Est | se | t | p | d [CI] | Est | se | t | p | |
| FACT-B | |||||||||
| PWB | 0.51 | 0.29 | 1.73 | 0.09 | 0.22 [−0.03;0.47] | 0.02 | 0.05 | 0.41 | 0.68 |
| SWB | 0.43 | 0.29 | 1.49 | 0.14 | 0.17 [−0.08;0.42] | −0.11 | 0.06 | −1.89 | 0.06 |
| EWB | 0.53 | 0.25 | 2.13 | 0.03 | 0.27 [0.02;0.52] | −0.02 | 0.04 | −0.51 | 0.61 |
| FWB | 0.64 | 0.28 | 2.28 | 0.02 | 0.27 [0.02;0.52] | −0.03 | 0.05 | −0.65 | 0.52 |
| BCS | 0.26 | 0.32 | 0.79 | 0.43 | 0.10 [−0.15;0.35] | −0.04 | 0.06 | −0.74 | 0.46 |
| Total | 2.00 | 0.98 | 2.03 | 0.04 | 0.22 [−0.03;0.47] | −0.14 | 0.16 | −0.86 | 0.39 |
| MOS-SSS | |||||||||
| Tangible | 1.21 | 1.13 | 1.07 | 0.28 | 0.10 [−0.15;0.35] | 0.15 | 0.21 | 0.70 | 0.49 |
| Affectionate | 2.12 | 1.25 | 1.70 | 0.09 | 0.21 [−0.04;0.46] | −0.24 | 0.25 | −0.98 | 0.33 |
| Positive | 2.61 | 1.29 | 2.03 | 0.04 | 0.27 [0.02;0.52] | −0.06 | 0.24 | −0.27 | 0.79 |
| Emotional | 2.87 | 1.25 | 2.30 | 0.02 | 0.21 [−0.04;0.46] | −0.09 | 0.21 | −0.41 | 0.69 |
| Total | 1.87 | 0.90 | 2.08 | 0.04 | 0.19 [−0.06;0.44] | −0.07 | 0.15 | −0.45 | 0.65 |
| FACIT-Sp | |||||||||
| Meaning | 0.29 | 0.17 | 1.76 | 0.08 | 0.20 [−0.05;0.45] | −0.04 | 0.03 | −1.34 | 0.18 |
| Peace | 0.60 | 0.21 | 2.73 | 0.01 | 0.38 [0.13;0.63] | −0.01 | 0.04 | −0.32 | 0.75 |
| Faith | 0.16 | 0.21 | 0.75 | 0.45 | 0.07 [−0.18;0.32] | 0.06 | 0.04 | 1.35 | 0.18 |
| Total | 1.10 | 0.46 | 2.36 | 0.02 | 0.27 [0.02;0.52] | −0.02 | 0.08 | −0.24 | 0.81 |
| PTGI-R | |||||||||
| Relating to others | 0.75 | 0.41 | 1.81 | 0.07 | 0.24 [−0.01;0.49] | 0.11 | 0.08 | 1.39 | 0.17 |
| New possibilities | 0.78 | 0.31 | 2.53 | 0.01 | 0.31 [0.06;0.56] | 0.09 | 0.07 | 1.34 | 0.18 |
| Personal strength | 0.13 | 0.29 | 0.45 | 0.66 | 0.07 [−0.18;0.32] | 0.08 | 0.06 | 1.41 | 0.16 |
| Spiritual change | 0.28 | 0.15 | 1.83 | 0.07 | 0.20 [−0.05;0.45] | 0.02 | 0.03 | 0.81 | 0.42 |
| AOL | −0.04 | 0.19 | 1.33 | 0.82 | −0.03 [−0.28;0.22] | 0.03 | 0.03 | 0.96 | 0.34 |
| Total | 2.21 | 0.97 | 2.27 | 0.02 | 0.26 [0.01;0.51] | 0.42 | 0.19 | 2.22 | 0.03 |
- PWB, Physical well-being; SWB, Social well-being; EWB, Emotional well-being; FWB, Functional well-being; BCS, Breast cancer symptom scale; AOL, Appreciation of life; FACT-B, Functional Assessment of Cancer Therapy-Breast; MOS-SSS, Medical Outcomes Study Social Support Survey; FACIT-Sp, Functional Assessment of Chronic Illness therapy-Spiritual; PTGI-R, post-traumatic growth Inventory-Revised.
Social Support: On the MOS-SSS, there were no significant differences between groups on any subscales and MOS-SSS total at baseline. The differences of growth rates between groups favoured MBCR on Positive support (p = 0.04), Emotional/Informational support (p = 0.02) and Total support (p = 0.04) during the intervention period, along with main effect of time on Positive support and Total support, with small effects, which were maintained over the follow-up period. However, Affectionate support decreased slightly (p = 0.03) in both groups at follow-up (Table 3).
Spirituality: At baseline, the MBCR group had higher Meaning and Total spirituality scores than the SET group. FACIT-Sp scores on the Peace subscale and overall scores improved more from pre-intervention to post-intervention in the MBCR group than in the SET group, with small to medium effects that were maintained over time (Table 3).
Post-Traumatic Growth Inventory-Revised: The Personal Strength subscale and the Appreciation of Life subscale were higher in the MBCR group at baseline. PTGI-R scores improved during the intervention period in both groups on subscales of New Possibilities, Personal Strength and on the Total score, but more in MBCR on New Possibilities and the Total score (Table 3). At follow-up, most differences were maintained on the subscales, but the total score continued to increase in MBCR relative to SET (Supplementary Figure S3).
Discussion
This study is the first to show lasting effects of an MBI in a comparative effectiveness trial against another active intervention. In the primary analysis of outcomes pre–post intervention, MBCR proved superior to SET and the control group on overall stress symptoms, quality of life and social support 15. Here, we included a broader range of outcomes, including positive psychology measures of flourishing and growth, and investigated all the subscales of the various measures used, not only total scores as in the primary outcomes paper. This revealed some interesting patterns of outcomes. Overall, while there were main effects of time across measures pre-intervention to post-intervention, indicating women in both MBCR and SET benefitted from the interventions, the magnitude of improvements was consistently larger for the MBCR group. Improvements gained immediately following both programmes were maintained over the full year of follow-up; hence, because immediate benefits were larger in magnitude for MBCR, these greater improvements were maintained. Across outcomes effect sizes between groups ranged from small to medium, with the largest effects seen on fatigue (d = 0.45), muscle tension (d = 0.42), confusion, anxiety (d = 0.39), sympathetic arousal, feelings of peace (d = 0.38) and new possibilities (d = 0.31).
While the majority of these benefits were maintained for the full year of follow-up, one measure continued to improve differentially over time: PTG. This suggests that the full impact of the MBCR programme on the ability to appreciate life, find meaning and purpose and see new possibilities from the breast cancer experience was not fully felt immediately after the programme, but rather continued to develop slowly over time. Overall, these results paint a picture of the slate of benefits accrued by women in the MBCR group – they felt more relaxed yet also energized, could focus and concentrate more easily, were more at peace with their lot in life and optimistic about the future. This is in contrast to before the programme when mood disturbance and anxiety were quite high. Women in the SET group also benefited in many of the same ways, but not to the same degree. We are heartened to see that these benefits persisted over the course of a full year.
In terms of the specificity of these findings, this is the first study to show differential effects specific to MBCR, while controlling for nonspecific therapeutic factors and group support, which were also part of the SET intervention. In the Henderson study, comparing MBSR with health education controls, while the MBSR group initially benefited much more than control, the benefits eroded over time and at 1 year they were only superior on one measure 14. By contrast, in our study, the incremental improvements in MBCR over SET persisted for the full year, suggesting there are lasting specific and unique benefits of training in mindfulness practices, above and beyond those due to the salubrious effects of group support and sharing, attention from caring professionals, self-monitoring and the boost to self-efficacy associated with doing something positive for one's own health. More research using comparative effectiveness trial designs is needed to further elucidate any benefits specific to MBIs.
There are, however, also several limitations that need to be taken into account in interpreting these results. Most important is the high attrition rate over the course of the year, in which we lost contact with half of the participants. This is troubling as there is a possibility that those who were lost to follow-up were somehow different from those who completed the data collection. They may have been worse off, and hence, the effects we report might be exaggerated. However, the HLM modelling estimates a growth curve for each participant with one or more data points, taking into account their scores in relation to others with similar profiles to impute the missing values. This attenuates somewhat the error associated with other approaches, which use last observation carried forward or eliminate people with incomplete data entirely. As well, we compared the baseline scores of all participants with complete data to those without and found both no differences between dropouts and completers overall and no differences between dropouts in the two groups. Hence, the assumption that women dropped out of groups equally and for similar reasons is most likely valid, as is the assumption that dropouts were not dissimilar from completers in any significant way. This likely supports the comparative results between the two groups, but the magnitude of the change could be smaller were all participants included.
Another limitation is the large number of tests conducted, because we wanted to investigate effects on all the subscales of our six main outcome measures. These subscale analyses should be considered exploratory in nature, because we choose not to correct for multiple comparisons. It is interesting to note, however, that many of the comparisons were highly significant (ps < 0.001) and likely would have remained so with corrections in place. These results should be used to suggest measures and constructs that may respond to MBIs and be further tested in future studies.
Finally, an unexpected finding was that baseline scores on a few of the stress, spirituality and PTG subscales were worse at baseline in the SET group, suggesting the possibility that group differences in slopes might be due to these baseline differences. Contrary to this possibility is the observation that more extreme baseline scores usually show more regression towards the mean and improve to a greater degree than less extreme scores. However, in this study, the opposite was found: the SET group showed less change over time than the MBCR group. The HLM analyses also included baseline values as random effects in each analysis, further mitigating the possibility that these baseline differences affected the results.
In sum, these results represent the first demonstration in a comparative effectiveness approach that MBCR is superior to another active intervention, SET, which also showed lesser benefit to distressed survivors of breast cancer. Our previous report also showed that MBCR was superior to a minimal intervention control condition pre-intervention to post-intervention. Benefits were accrued across outcomes measuring stress, mood, quality of life and PTG, painting a picture of women who were more able to cope with cancer survivorship and to fully embrace and enjoy life.
Acknowledgements
Dr. Linda Carlson holds the Enbridge Research Chair in Psychosocial Oncology, co-funded by the Canadian Cancer Society Alberta/NWT Division and the Alberta Cancer Foundation. This study was funded by a grant from the Canadian Breast Cancer Research Alliance. Many thanks to all the research staff who worked on this project: Beth DeBruyn, Barbara Pickering, Linnette Lawlor-Savage, Kimberley Burris and Dale Dirkse. Thanks also to the programme facilitators: Shirley MacMillan, Lisa Lamont, Sarah Sample and Heather Rennie. Finally, none of this work would be possible without the generous participation of so many breast cancer survivors.
Conflict of interest
The authors have declared no conflicts of interest.