Lupus miliaris disseminatus faciei treated with 1,565 nm nonablative fractionated laser resurfacing: A case report
Abstract
Background
Lupus miliaris disseminatus faciei (LMDF) is a rare granulomatous disease. It presents as red-brown papules on the face that can resolve with scarring. LMDF is often resistant to treatment.
Objective
Nonablative fractionated lasers have been used effectively to treat granulomatous disorders; however, there is little data on the treatment of LMDF with lasers. Our objective was to test a novel non-ablative fractionated laser for the treatment of recalcitrant LMDF.
Results
A 24-year-old man had a one-year history of LMDF. He had been treated with various topical therapies, oral medications, and laser devices with no improvement and continued progression. We utilized a non-sequential scanning 1,565 nm nonablative fractionated laser to treat this patient. After only one treatment he had significant improvement. He has been subsequently treated five times in the past 6 months and has continued to improve.
Conclusion
The novel 1,565 nm nonablative fractionated laser may be a useful tool in the treatment of granulomatous conditions such as LMDF. Lasers Surg. Med. 46:663–665, 2014. © 2014 Wiley Periodicals, Inc.
INTRODUCTION
Lupus miliaris disseminatus faciei (LMDF) is a rare disorder of unclear etiology characterized by red-brown papules on the face that can resolve with scarring. Epithelioid granulomas with caseation necrosis are typical on histopathology. Overall response to treatment is poor 1. Nonablative fractionated lasers have been used effectively to treat granulomatous disorders, but there are few reports on treatment of LMDF with lasers 2. Herein we report the successful treatment of LMDF with a novel non-sequential scanning 1,565 nm nonablative fractionated laser.
CASE REPORT
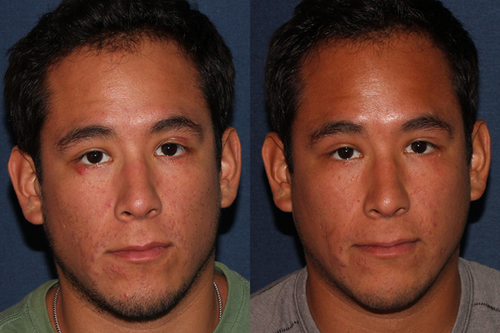
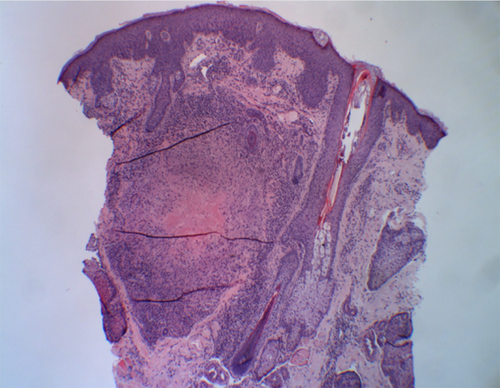
A 24-year-old male Navy SEAL with biopsy-proven LMDF presented to our office with a 1-year history of red-brown papules involving the central face and upper and lower eyelids (Fig. 1a). A biopsy demonstrated a large caseating granuloma comprised of epithelioid histiocytes with scattered multinucleated giant cells, consistent with LMDF (Fig. 2). Stains for fungal and mycobacterial organisms were negative. Investigations for sarcoidosis, including chest radiography and angiotensin converting enzyme level, were normal.
The patient had been previously treated with numerous oral agents including doxycycline, tetracycline, amoxicillin/clavulanate, a short course of systemic corticosteroids, itraconazole, and isotretinoin. The isotretinoin, however, had been discontinued after only 2 months due to decreased athletic performance. Topical treatments included permethrin 5% cream, pimecrolimus 1% cream, tretinoin 0.025% cream, and metronidazole 1% gel. Intralesional triamcinolone acetonide (5–10 mg/ml) was injected into the eyelid papules. He was also treated with three sessions of low fluence Nd:YAG 1,064 nm laser, two sessions of 595 nm pulsed dye laser (PDL), and one session of 532 nm frequency-doubled Nd:YAG (albeit only to the eyelids). Despite the diverse treatments attempted, he had no improvement, only progression of lesions.
On presentation, the patient was treated initially with 595 nm PDL to the upper lip, without improvement, followed by two sessions of nonablative fractionated 1,440/1,320 nm Nd:YAG laser (Affirm Multiplex, Cynosure, Inc., Westford, MA) to the left chin and ablative fractionated 10,600 nm CO2 laser (Deep FX, Lumenis Ltd., Yokneam, Israel) to the right chin. The patient had minimal to no improvement from the above treatments at 1-month follow-up.
Given the lack of response to all other modalities, treatment of the chin, cheeks, and infraorbital areas was performed with a nonablative fractionated 1,565 nm erbium-doped fiber laser (ResurFX, Lumenis Ltd., Yokneam, Israel). A 12 mm spot size was used to deliver a density of 350 spots/cm2 and pulse energy of 40 mJ, with built-in contact cooling via a sapphire crystal tip for epidermal protection and pain control. Additional forced cold air cooling (Cryo 6, Zimmer MedizinSysteme, Irvine, CA) was used at a cooling level of 5. Significant improvement was noted in treated areas after the initial treatment session.
Although it is possible that the improvement in LMDF was spontaneous, the substantial response in the treated areas after only one session—after a long period of lesion progression—suggests the laser did contribute to this clinical improvement. It is also likely that his disease process was at a stage where it was significantly more treatment-responsive. Given his treatment response with this modality, we decided to continue treating at monthly intervals. The patient has currently been treated five times in the past 6 months and has continued to improve with each subsequent treatment (Fig. 1b).
DISCUSSION
LMDF, also known as acne agminata or facial idiopathic granulomas with regressive evolution, is a rare granulomatous, inflammatory disease of unclear etiology 3. It has been categorized as a variant of granulomatous rosacea or sarcoidosis; however, LMDF is often viewed as a distinct entity 4.
LMDF is usually seen in adults between the second and fourth decades of life 3, with most patients being male 4. LMDF is characterized by yellow-red to yellow-brown papules on the central face with a predilection for the periocular region. Granulomatous infiltrates with central caseating necrosis are the classic histologic features of LMDF 3. A 1-year period of stability is usually followed by spontaneous involution of the lesions 4. Residual pitted scars have been reported as a characteristic feature 1.
Reported treatments include oral medications such as dapsone, corticosteroids, clofazamine, doxycycline, minocycline, and isotretinoin. Topical erythromycin, metronidazole, and psoralen-ultraviolet A treatment have also been used 5. However, cessation of therapy is often associated with relapse and overall response to treatments is poor 1. More recently, a 1,450 nm diode laser was shown to improve LMDF. Success of this laser was hypothesized to be due to reduction in proinflammatory mediators, thermal damage of granuloma structure, neocollagenesis, and reduction in bacteria that may potentiate granuloma formation 1.
Given the limited success with previous treatments, our group initiated treatment with a nonablative fractionated 1,565 nm laser. Nonablative fractionated skin resurfacing produces narrow, vertical columns of tissue coagulation (microscopic treatment zones, MTZs) in the epidermis and dermis, leaving the stratum corneum and tissue surrounding the MTZs unaffected. These columns of coagulation stimulate the body's natural healing response, causing new, healthy epidermal and dermal tissue formation 6. Infrared laser energy at 1,565 nm has a slightly lower absorption coefficient for water than that of other available nonablative devices, leading to potentially greater dermal penetration. This particular nonablative fractionated laser delivers laser pulses in a non-sequential manner through a sapphire cooled window to both minimize pain and protect non-laser impacted epidermis. This likely allows for quicker healing, less adverse effects, and the possibility of utilizing higher pulse energies. The ability to safely use higher pulse energies and resulting greater dermal penetration with this device may have contributed to the significant improvement in this patient. Double-blind, randomized-controlled split-face studies are warranted to verify the efficacy of nonablative fractionated 1,565 nm laser therapy for LMDF.
Nonablative fractionated lasers have been reported in the treatment of granulomatous disorders such as granuloma annulare. It is thought that wound healing stimulated by this laser may act to resolve the granulomatous inflammation 2. The novel 1,565 nm nonablative fractionated laser may work by similar mechanism and thereby be a useful tool in the treatment of granulomatous conditions such as LMDF.