Whither melanoma in Australia?
To improve melanoma outcomes, the focus on prevention, early detection and new treatment strategies must continue
Over the past 5 years, we have seen a dramatic response to the intense biological research into late-stage, metastatic melanoma, with therapies targeting melanoma metastases and improving an individual's immune response to the disease. This has led to an improvement in progression-free and overall survival in a group of patients who would have previously been treated with drugs that had little effect. Intense research and clinical trials continue with the aim of identifying patients most likely to respond, as well as exploring new combinations of therapies with this new paradigm for melanoma treatment.
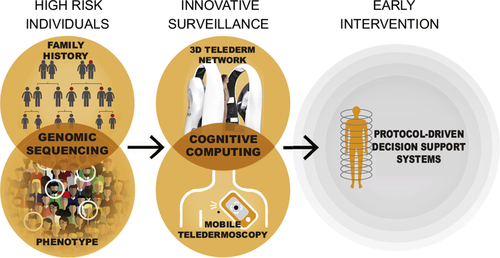
As exciting as it is for patients and the community to see and hear of these advances in melanoma treatment, we must not relax our focus on prevention and early diagnosis, because together these actions will have a greater impact. Recent incidence data in Australia between 1982 and 2011 show a peak in 2005, with a projected reduction expected over the following 20 years.1 This reduction appears to relate to the younger cohorts who appear to have had less ultraviolet radiation exposure compared with the older members of the community (aged over 60 years) who continue to have an alarming and sustained rate increase. This decline in the rates of melanoma in young Australians reinforces the effective and critical role that focused, evidence-based public health campaigns can play in improving the health status of a community. For melanoma, it was the Slip, Slop, Slap campaign in the 1980s and the SunSmart campaign in the 1990s that increased the focus on children. This experience demonstrates the need for a sustained commitment to such programs because change may take decades, as it has with melanoma rates. Most invasive melanomas in Australia are diagnosed at an early stage (less than 1 mm thick) where the overall survival at 20 years is 96%.2 In Queensland, campaigns of public and professional education into melanoma began in the late 1960s and resulted in better survival figures in Queensland compared with other countries.3 A continued national focus on public and professional education about melanoma will offer benefit to individuals and improvement in costs for the health system.4 Along with public campaigns for early diagnosis, identification of and appropriate surveillance schedules for individuals at high risk of developing a melanoma need to be explored further. The highest risk individuals will be identified by deploying epidemiologically based melanoma risk classification with the incorporation of next generation genomics.5 For this group, imaging technology and artificial intelligence will allow development of precision medicine protocols (Box) for the targeted early detection of melanoma.6 This approach will involve innovative surveillance using total body imaging technologies and cognitive computing, in both the traditional clinical setting and via pioneering consumer engagement models (mobile teledermoscopy and melanoma apps), as noted by Janda and Soyer in this issue of the MJA.7 Cutting-edge imaging technology that generates a digital 3D model of an individual's skin allows for easy tracking and monitoring of skin lesions over time and will minimise unnecessary excisions. This technology is ideally suited to telehealth implementation, which along with the complementary consumer imaging modalities, will allow more equitable access to specialist care for Australia's highly dispersed population. These advances in technology and continued education can also enhance the recognition of atypical presentations of melanoma to improve their early detection, as highlighted in a guideline summary by Mar and colleagues8 and a research article by Pan and Adler and colleagues9 in this issue of the MJA.
In Australia in 2016, it was estimated that 1770 people would die from melanoma.10 The focus on early detection must continue through public health and medical education, as well as research into more personalised, technology-driven care that focuses on identifying individuals who have a higher risk of developing the disease. The impetus to treat subclinical metastasis through adjuvant therapies and treat patients with evidence of metastatic disease also needs to be maintained by assessing new therapies, along with perfected use of the treatments presently improving survival.
In Australia, we have the transdisciplinary expertise in public health, disease management, and clinical and scientific research to minimise the impact of melanoma on individuals and to reduce the burden of associated health care costs on the community with improvement of health outcomes. This will be achieved by an ongoing and holistic focus on preventive strategies to reduce melanoma incidence, early detection to downstage the disease at the point of diagnosis, and through the translation of innovative research and practice to optimise patient care.
Provenance
Commissioned; not externally peer reviewed.
Competing Interests
No relevant disclosures.