Mandibular Premolar Impaction
Abstract
Literature specific to impacted premolars is not extensive despite the fact that mandibular 2nd premolars alone account for 2.4% of dental impactions. The purpose of this paper is to describe the radical approach (extraction) of a transversally impacted 2nd premolar in the mandible through a lingual approach due to its peculiar position presuming it will contribute toward the literature regarding impacted mandible premolars.
1. Introduction
Impacted teeth are those which are prevented from erupting by some physical barrier, in the eruption path. Lack of space, due to the crowding of the dental arches or to premature loss of primary teeth with subsequent partial closure of their area, is a common factor in the etiology of partially or completely impacted teeth. Genetic and environmental factors are included in the multifactorial nature of tooth eruption, which may be disturbed at any stage of tooth development [1]. By definition, an impacted tooth is one that is embedded in the alveolus so that its eruption is prevented or the tooth is locked in position by bone or the adjacent tooth/teeth [2]. Mandibular second premolars rank third after third permanent molars and maxillary permanent canines, in frequency of impactions [3]. The prevalence of impacted premolars has been found to vary according to age [4]. The overall prevalence in adults has been reported to be 0.5% the range being 0.2 to 0.3% for mandibular premolars [4, 5]. Premolar impactions may be due to local factors such as mesial drift of teeth arising from premature loss of primary molars; ectopic positioning of the developing premolar tooth buds; or pathology such as inflammatory or dentigerous cyst. They may also be associated with over retained or infraocclusal ankylosed primary molars or with syndromes such as cleidocranial dysostosis [6–11]. In the anterior mandible, the mandibular premolars erupt after the mandibular first molar and mandibular canine. Thus if the room for eruption is inadequate, one of the premolars usually the second premolar remains unerrupted and becomes impacted [12]. Literature specific to impacted premolars is not extensive despite the fact that mandibular second premolars alone account for approximately 24% of all dental impactions [3, 13]. Various treatment methods have been suggested including observation, intervention, relocation, and extraction depending on the tooth’s position, depth of the impacted tooth, relationship with adjacent teeth, and orthodontic treatment. This case report describes the radical approach (extraction) of a transversally impacted 2nd premolar in the mandible in an unusual position with the crown lying lingual to the root apices of 1st molar tooth through a lingual approach presuming it will contribute toward the literature available regarding impacted 2nd premolars. The unusual orientation of the crown and root of this impacted 2nd PM makes this case report rare.
2. Case Report
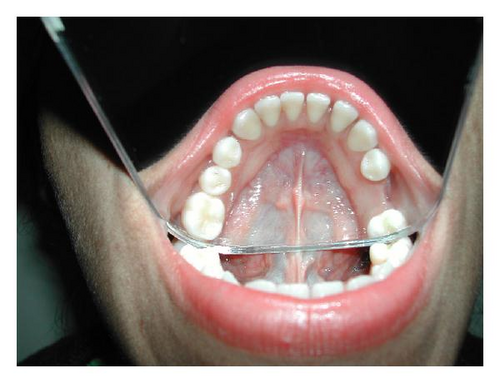
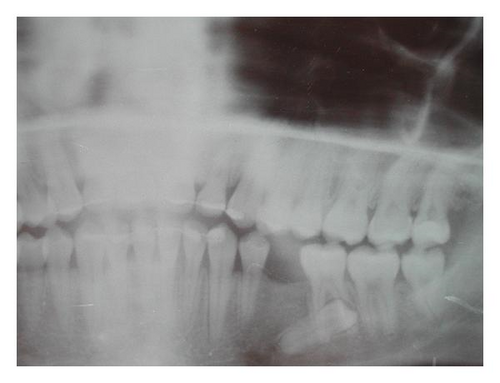
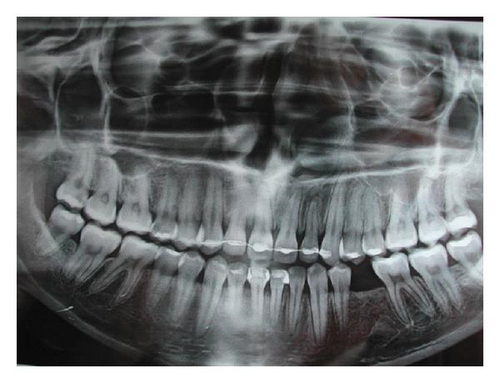
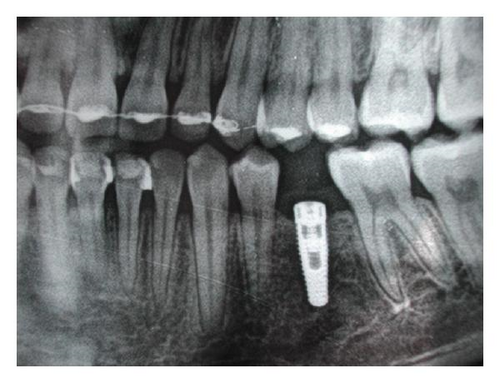
An 18-year-old girl was referred after orthodontic intervention for the removal of an impacted left 2nd premolar tooth 35 which was not visible in the oral cavity. An adequate edentulous space was present instead of tooth 35, and there was a history of extraction of over retained deciduous predecessor during the orthodontic treatment. The present plan was to extract the impacted tooth, place an implant, and rehabilitate the patient. The patient had no significant medical history with no apparent systemic problems. She did not report any history of trauma to the jaws. Intraoral examination revealed the presence of 34 and 36 teeth with an adequate space between them for a 35 to erupt (see Figure 1), but the alveolar bone density in the region was diminished. The occlusion was satisfactory with no trismus, and oral hygiene was good. On palpation, a little bulge could be felt on the lingual aspect of 36, at the level of the mylohyoid ridge (see Figure 2). The intraoral periapical X-ray and OPG (see Figure 3) revealed the presence of a severely impacted 2nd premolar tooth 35 which was lying almost horizontal with the crown facing distally and was overshadowed by the roots of tooth 36. The roots of the impacted tooth were mesially directed but appeared short and stunted. The deep impacted mandibular second premolar was extracted from the lingual approach in a surgical procedure under local anesthesia. An incision was given in the lingual gingival crevice extending from 2nd molar to canine tooth; with a mucoperiosteal elevator, a lingual flap was raised to expose the lingual aspect of 36. A slight bulge on the bone was visible (see Figure 4). A sterile high speed handpiece cooled with sterile saline solution was used for osteotomy and crown sectioning. The crown was removed and then the root was delivered (see Figures 5, 6). The wound was irrigated, homeostasis was achieved, and the wound was closed with 3-0 silk sutures. Sutures were removed on the seventh postoperative day. The patient healed uneventfully and clinical and radiographic followups were satisfactory (see Figure 7). Once the bone healing was optimum, an implant was placed in the area of tooth 35 (see Figure 8).




3. Discussion
Treatment options for impacted teeth include observation, intervention, relocation, and extraction. On occasions, there may be some interaction between these treatment options [14]. Literature specific to impacted premolar is not extensive despite the fact that mandibular 2nd premolars alone account for approximately 24% of all the dental impactions [13]. In selecting an appropriate treatment option, the underlying etiological factors, space requirements, need for extractions of primary molars, degree of impaction, and root formation of the impacted premolar should be considered. Factors such as patients medical history, dental status, oral hygiene, functional and occlusal relationship and attitude toward and compliance with treatment will influence choice of treatment options [15, 16]. In this particular case, the degree of impaction, unusual placement of the impacted tooth, that is, transverse position and crown present lingual to the root apices of the first permanent molar, the complete root formation, and the reduced level of available dentoalveolar bone made monitoring a bad choice of treatment as at 18 years of age growth potential had ceased. The position of the transversely impacted second premolar was so unfavorable that no orthodontic treatment of this tooth was envisaged, and hence extraction was planned. Andreasen [4] suggests that surgical exposure should be confined to cases, both maxillary and mandibular with no more than 45° tilting and limited deviation from the normal position, and hence this case definitely required removal of the impacted tooth. As the crown was on the lingual aspect, the lingual approach and splitting of the tooth, that is, odontectomy with odontotomy was the logical choice. The lingual approach was taken due to the tooth position. Besides, the buccal flap would have jeopardized the mental nerve emerging from the mental foramen and the apices of the first permanent molar tooth. But lingual approach comes with the inherent risk of infection in the sublingual space. Careful irrigation of the surgical area and not allowing the bone and tooth dust to remain in that area prevent any delayed healing and infection. Correct knowledge of regional anatomy, careful manipulation of tissues, and correct application of mechanical principles involved in tooth extractions allow surgical success. This peculiar and rare case will contribute toward the minimal literature available regarding impacted second premolar tooth and offers lingual approach as an alternative in such situations.