Hippocampal sclerosis caused by repetitive parieto-insular seizures through a possible kindling mechanism
A 37-year-old woman with a right parietal oligodendroglioma developed focal epilepsy with 10 years of infrequent parietal seizures. Four days after surgery due to tumor recurrence, she had focal non-convulsive status epilepticus with impaired consciousness and slightly different parieto-insular semiology (one-hour subintrant manifestations of numbness in both hands and the perioral region, dystonic posture of the left hand and left oculocephalic version, along with mild impairment of consciousness), controlled with different anti-seizure drugs. Three weeks later, postoperative MRI showed right hippocampal hyperperfusion and swelling (figure 1), as well as the total tumor resection. Over the next months, she developed refractory typical temporal lobe seizures with onset consisting of rising epigastric sensation followed by piloerection and impaired awareness, not present before surgery, with resolution of previous parieto-insular seizures. MRI performed six months post-operatively showed hippocampal atrophy (figure 2) without tumor recurrence. Eventually, the patient underwent an anterior temporal lobectomy which controlled her seizures (Engel Class IA, at 18 months of follow-up). Histopathology was consistent with type 1 hippocampal sclerosis [1]. Kindling via repetitive electrical stimulation of limbic structures is a well-known model of epileptogenesis in temporal lobe epilepsy in animals, yet still poorly demonstrated in humans. This case displays evidence of previous normal hippocampi, and new acquired functional, structural and pathological findings consistent with hippocampal sclerosis after the status, along with a concordant variation in semiology. These findings support the idea of how, in an adult patient, repetitive extratemporal non-convulsive seizures may provoke hippocampal sclerosis through a possible kindling mechanism in the limbic pathway [2].
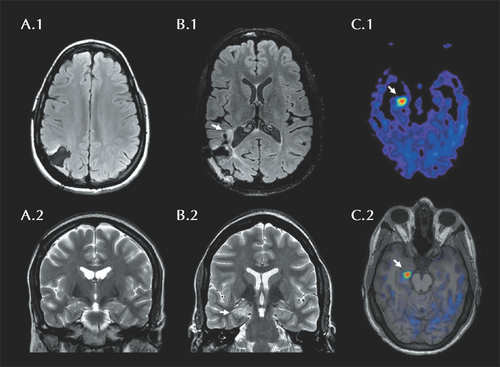
Neuroimaging showing right hippocampal swelling after repetitive seizures. Initial axial FLAIR and coronal T2 sequences show tumor resection (A.1) with normal hippocampi (A.2). A MRI after repetitive seizures shows progression of the tumor over the posterior insula (B.1), while, three weeks after the status epilepticus, coronal T2 sequence (B.2) depicts marked swelling of the right hippocampus with hyperperfusion on arterial spin labelling (C.1, C.2).
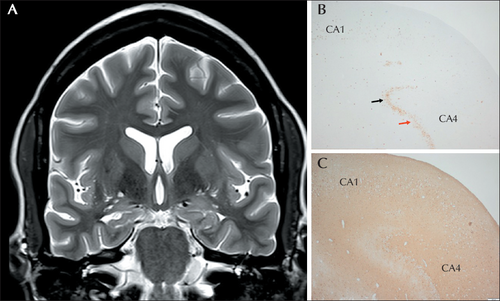
Follow-up MRI and pathology demonstrate right hippocampal sclerosis. Six months after the status epilepticus, a follow-up T2 coronal sequence shows right hippocampal sclerosis (A) while the pathology confirmed type 1 hippocampal sclerosis: decreased neuronal densities and gliosis in sectors CA1 and CA4 on NeuN/GFAP immunohistochemistry (B, C) with granule cell dispersion (black arrow) and foci of granule cell loss (red arrow).
Disclosures
None of the authors have any conflicts of interest to declare. No financial support was required for the writing and publication of this paper.