Internet of Things in Healthcare Research: Trends, Innovations, Security Considerations, Challenges and Future Strategy
Abstract
The Internet of Things (IoT) has become a transformative force across various sectors, including healthcare, offering new opportunities for automation and enhanced service delivery. The evolving architecture of the IoT presents significant challenges in establishing a comprehensive cyber-physical framework. This paper reviews recent advancements in IoT-driven healthcare automation, focussing on integrating technologies such as cloud computing, augmented reality and wearable devices. This work examines the IoT network architectures and platforms that support healthcare applications while addressing critical security and privacy issues, including specific threat models, attack classifications and security prerequisites relevant to the healthcare sector. This study highlights how emerging technologies like distributed intelligence, big data analytics and wearable devices are incorporated into healthcare to improve patient care and streamline medical operations. The findings reveal significant potential for IoT to transform healthcare practices, particularly in-patient monitoring, and clinical decision-making. However, security and privacy concerns continue to be a substantial barrier. The paper also explores the implications of global IoT and ehealth strategies and their influence on sustainable economic and community growth. It proposes an innovative cooperative security model to mitigate security risks in IoT-enabled healthcare systems. Finally, it identifies key unresolved challenges and opportunities for future research in IoT-based healthcare.
1. Introduction
The Internet of Things (IoT) entails a connected network of people, devices, services and systems that can be accessed anytime, anywhere, through any network. As a transformative trend in modern automation, IoT has the potential to revolutionise entire industries by enabling the interconnection of uniquely identifiable smart devices within the existing Internet infrastructure. This connectivity extends beyond traditional machine-to-machine (M2M) scenarios, introducing automation possibilities across diverse domains [1]. IoT provides solutions through various applications, including smart cities, traffic management, waste management, physical fitness, safety, backup services, logistics, commercial activities, industrial control and healthcare [2]. Among these applications, healthcare is one of the sectors most significantly impacted by IoT [3]. IoT can transform medical applications such as remote health monitoring, wellness programmes, chronic disease management and elderly care. Integrating various medical sensors, diagnostic tools and imaging devices into the IoT significantly enhances medication management at home and within healthcare settings. This facilitates improved monitoring and care for patients [4].
IoT-based healthcare services are expected to reduce costs, improve quality of life and enhance user experiences. From the perspective of healthcare providers, IoT can reduce device downtime allowing for efficient scheduling of routine and continuous operations [5]. IoT optimises healthcare resources that are already limited, leading to enhanced patient care. Easy access to medical facilities and healthcare records is essential for building comprehensive health profiles and delivering on-demand services to authorised stakeholders. Over the years, researchers have thoroughly explored IoT’s potential in healthcare, addressing real-world challenges. This has led to the development of various valuable applications, services and models that exemplify the transformative effect of the IoT on the healthcare industry [6].
IoT with deep learning techniques [7,8] for pandemic detection highlights recent developments in IoT-based health monitoring systems, especially concerning pandemic detection and response. Applications such as this emphasise a need for the integration of IoT with advanced machine learning techniques, particularly convolutional neural networks (CNNs), in healthcare applications. It highlights the significance of emerging technologies in healthcare automation and illustrates the role of deep learning in enhancing IoT systems [9].
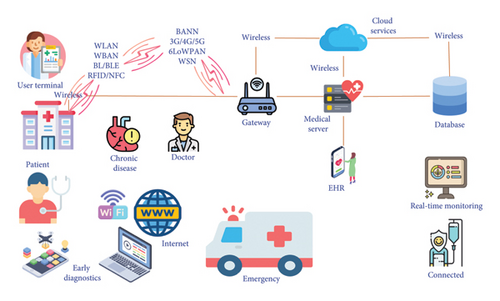
Figure 1 illustrates the integration of IoT technologies in healthcare systems, highlighting key components such as wireless networks, core elements of IoT, applications of IoT, infrastructure and stakeholders of IoT. Wireless networks employed in IoT include wireless local area networks (WLAN), wireless body area networks (WBAN), Bluetooth/Bluetooth Low Energy (BL/BLE), Radio-Frequency Identification (RFID)/near-field communication (RFID/NFC), third-generation/fourth-generation/fifth-generation networks (3G/4G/5G/6G), IPv6 over low-power wireless personal area networks (6LoWPANs) and wireless sensor network (WSN). The core elements of IoT are the cloud services, databases, medical servers, gateways and user terminals. IoT applications include chronic disease management, early diagnostics, real-time monitoring, emergency services and connected healthcare devices. Stakeholders are the patients and healthcare providers such as doctors and infrastructures associated with IoT are the seamless flow of health data from patients to medical servers and cloud services, enabling enhanced diagnostics, treatment and care [10].
This study examines how emerging technologies like big data, wearable devices and distributed intelligence can enhance IoT-based healthcare solutions. It evaluates global IoT and ehealth strategies and regulations, analysing their impact on promoting sustainable growth and improving healthcare. This study further offers a comprehensive overview of the current state and future directions of IoT-based healthcare systems, exploring the associated opportunities and challenges. It provides researchers, engineers, healthcare professionals and policymakers valuable insights and enables these stakeholders to navigate the evolving landscape of IoT in healthcare and leverage its potential to improve health services and patient care.
The motivation for this study arises from the increasing adoption of IoT in healthcare [11,12], which promises significant improvements in patient monitoring, clinical decision-making and operational efficiency. However, despite the rapid growth of IoT technologies in this field, healthcare systems still face several critical challenges that hinder the full potential of these innovations. Key barriers include security vulnerabilities, data privacy concerns and the lack of seamless interoperability between different IoT platforms and healthcare systems. Additionally, while various IoT technologies, such as cloud computing, wearable devices and big data analytics, have been explored in healthcare applications, there is a pressing need for a comprehensive cyber-physical framework that integrates these technologies effectively. Another key concern is the absence of robust security models specifically tailored to the unique requirements of the healthcare industry. These issues threaten the reliability and scalability of IoT in healthcare environments. This study seeks to address these gaps by exploring IoT-driven healthcare automation, proposing an innovative cooperative security model and evaluating the integration of emerging technologies to improve both security and the overall performance of IoT systems in healthcare.
1.1. Research Questions
IoT-driven healthcare trends include advancements in network structures, platforms, new facilities and applications, as well as emerging concerns around security and privacy. Countries and organisations worldwide have developed various strategies and methodologies for integrating IoT technologies into the medical sector [13]. Integrating IoT in the healthcare sector remains in its initial stages, and insights derived from recent research on IoT applications within healthcare are anticipated to hold significant value for stakeholders keen on advancing and refining this technology.
- •
RQ1: How can IoT transform various industries, particularly healthcare, through the interconnection of smart devices and systems?
- •
RQ2: What are the core IoT and network-based technologies that can significantly enhance healthcare services and applications?
- •
RQ3: How can IoT Healthcare System (IoT network (IoTNet)) topology and platforms support remote monitoring, data integration and personalised healthcare in IoT-based healthcare systems?
- •
RQ4: How can IoT-enabled healthcare systems be categorised into services and applications, and what are these categories’ potential benefits and challenges?
- •
RQ5: What are the various industry trends in which IoT can be applied to healthcare, and how can these applications improve health outcomes and patient care?
- •
RQ6: What are the key security issues related to implementing and designing IoT-based healthcare systems, and how can these challenges be addressed?
- •
RQ7: How do different countries and organisations develop and implement IoT and eHealth strategies, and what impact do these policies have on the adoption and effectiveness of IoT in healthcare?
- •
RQ8: What are the key challenges and issues related to implementing and designing IoT-based healthcare systems, and how can these challenges be addressed?
1.2. Contributions
- •
Categorising current IoT healthcare network research into three main trends, with illustrative examples for each.
- •
Providing an in-depth review of IoT-enabled healthcare services and applications.
- •
Highlighting industry efforts to develop IoT-compatible healthcare products and prototypes.
- •
Conducting a thorough analysis of security and privacy challenges in IoT healthcare solutions and proposing a security framework.
- •
Discuss core technologies that have the potential to revolutionise IoT healthcare automation.
- •
Emphasising regulations and strategies to assist researchers and policymakers in effectively integrating IoT innovations into practical healthcare automation.
1.3. Comparison With Existing Reviews
Table 1 provides a comparative analysis of 20 articles from 2020 to 2024, highlighting the various aspects and integrations of artificial intelligence (AI) and IoT in healthcare. The attributes considered include IoT, machine learning, sensors and devices, embedded AI, explainability, Health Artificial Intelligence of Things (AIoT) [31], use cases and synergy of AI [32,33] and IoT [6]. The Internet of Medical Things (IoMT) represents a significant advancement in healthcare, particularly in managing COVID-19 through precise virus identification [34,35]. Nonetheless, the adoption of IoMT [36] is hindered by potential security concerns and obstacles related to the timely delivery of healthcare services. This study highlights the importance of Digital Clinical Trials (DCTs) and the development of IoMT and Internet of Health Things (IoHT) devices for broader use. A bibliometric analysis of 578 publications from Scopus and 500 from Web of Science (WoS) between 2017 and 2022 provides valuable insights into the field’s progress [36].
| Reference | Internet of Things | Machine learning | Sensors and devices | Embedded AI | Explainability | Health AIoT use cases | Synergy of AI and IoT |
|---|---|---|---|---|---|---|---|
| Thakare et al. [14] | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ |
| Alanazi et al. [15] | ✓ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ |
| Ghazal et al. [16] | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ | ✗ |
| Kashani et al. [17] | ✗ | ✓ | ✗ | ✗ | ✓ | ✗ | ✓ |
| Khan et al. [18] | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ |
| Rehman et al. [19] | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Chawla et al. [20] | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Chauhan et al. [21] | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ |
| Ahmad et al. [22] | ✗ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ |
| Gupta et al. [23] | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ | ✓ |
| Kute et al. [24] | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ |
| Aghdam et al. [25] | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ |
| Krishnamoorthy et al. [26] | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ | ✓ |
| Kute et al. [24] | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ |
| Goyal et al. [27] | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ |
| Donta et al. [28] | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ | ✓ |
| Gupta et al. [23] | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ |
| Goyal et al. [27] | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ |
| Kumar et al. [29] | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ |
| Chauhan et al. [29] | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ |
| Heyat et al. [30] | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ |
| This works | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
This comparative analysis reveals a clear trend towards the growing integration of AI and IoT in healthcare. Recent surveys (2021–2025) particularly emphasise the importance of explainability, embedded AI and the synergy of AI and IoT, indicating a shift towards more transparent, integrated and comprehensive healthcare solutions. This evolution highlights the potential of these technologies to revolutionise healthcare by providing more innovative, efficient and personalised care.
This paper identifies challenges and unresolved issues that must be addressed to strengthen IoT-centred healthcare automation. Notably, R&D efforts in healthcare services have concentrated on WSNs, the foundation of IoT-centred healthcare research [37]. The prevailing direction is shifting from conventional norms towards integrating IP-based network devices, especially with the emergence of 6LoWPAN [38]. As WSNs continue to play a crucial role on the internet, further examination is essential to comprehensively ascertain their importance and function within the healthcare context of IoT. Ref. [39] provides an extensive assessment of WSNs in IoT and their distinctions.
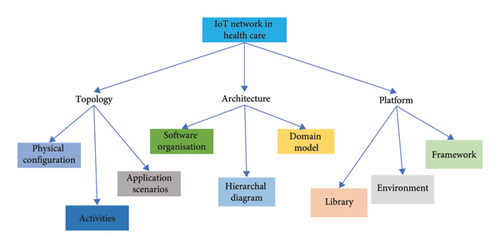
The study begins by examining IoT technologies in the healthcare sector, highlighting key advancements such as cloud computing, augmented reality, big data analytics and wearable devices. The subsequent section, titled ‘IoT Healthcare System (IoTNet)’, provides a detailed overview of the network structures and platforms that enable IoT integration in healthcare, outlining their benefits and practical applications.
The section titled ‘IoT Healthcare Applications and Services’ presents an in-depth analysis of specific IoT applications and services within the healthcare sector, including remote monitoring and telemedicine. Following this, the ‘IoT Healthcare Scenarios’ section provides a comprehensive examination of real-world use cases, emphasising the management of various medical conditions through implementing IoT technologies.
The paper also evaluates Global IoT Healthcare Policies, thereby assessing their impact on the implementation and effectiveness of IoT solutions in healthcare. It is followed by the ‘IoT Healthcare Challenges and Issues’ section, which discusses key challenges such as interoperability, scalability and data security.
In the ‘Future Directions and Research Opportunities’ section, the paper highlights areas for further exploration to address ongoing challenges and leverage emerging technologies for enhanced IoT healthcare systems. The study concludes with a summary of key findings and contributions, emphasising the transformative potential of IoT in the healthcare industry.
2. Technologies of IoT in Healthcare
Given the extensive list of IoT-based technologies that provide healthcare solutions, creating a comprehensive list can be pretty complex. As a result, this discussion aims to underscore some key technologies that are poised to revolutionise IoT-based healthcare services and applications substantially.
2.1. Cloud Computing
Integrating cloud computing into IoT-based healthcare technologies enables facilities to provide seamless access to shared resources, on-demand services and network capabilities. This combination helps meet various operational needs efficiently while ensuring flexible and scalable service delivery [26].
2.2. Augmented Reality
Augmented reality is vital in healthcare engineering as part of IoT. This technology is particularly beneficial for applications such as remote monitoring and surgery, among other healthcare innovations [23].
2.3. Grid Computing
The integration of medical sensor nodes (MSNs) into an extensive healthcare network through cluster-based computing effectively addresses the inherent limitations of these devices in terms of computational capacity. This approach is fundamental to cloud computing and markedly enhances the efficiency and capabilities of MSNs within healthcare systems [40].
2.4. Ambient Intelligence
In healthcare networks, the primary individuals served are patients and health-conscious consumers. Therefore, implementing ambient-oriented intelligence is essential. Ambient-oriented intelligence facilitates the continuous learning of human behaviour, leading to the automatic initiation of actions based on recognised activities or events. Additionally, integrating automatic control systems with human–computer interaction (HCI) technologies can significantly enhance the capabilities of IoT-based healthcare services [41].
2.5. Wearables’ IoMT
The adoption of wearable medical devices is essential for enhancing patient engagement and advancing overall population health outcomes. These devices present substantial benefits, such as providing access to specific health data within healthcare networks and addressing informational requirements.
2.6. Big Data
Collecting a significant volume of data from diverse medical sensors utilised across healthcare sectors is essential. These data are essential for the innovation of tools intended to enhance health diagnostic processes and improve monitoring techniques and protocols [42].
2.7. Networks
The infrastructure of IoT in healthcare is made of both long-range (LoRa) communication networks, such as cellular-based systems and short-range communication systems. The latter includes WPAN, WLAN, low wireless personal area networks and WSN. Furthermore, this infrastructure incorporates advanced technologies such as ultra-wideband (UWB), BLE, NFC and RFID. These technologies are essential for the development of low-power healthcare sensor devices and effective communication protocols [43].
In the last 2 decades, numerous standards for the development of human health sensing devices have been established. These standards have had a considerable impact on healthcare systems, and they can be categorised into two main types: cellular and noncellular technologies. Notably, legacy standards in unlicensed environments tend to emphasise noncellular technologies. This review evaluates these proposed standards’ positive and negative impacts, particularly emphasising low-power wide area (LPWA) technologies and their influence on healthcare systems and further highlights the substantial advancements in healthcare resulting from developing standards for human health sensing machines, including LPWA technologies, smart body area networks (SmartBAN) and IEEE Standards, each offering distinct advantages and limitations. As these standards continue to evolve, they are expected to enhance the quality and efficiency of healthcare services, providing various solutions for different healthcare applications [44].
2.8. LWPA Technologies
LPWA technologies, which utilise noncellular mechanisms, are specifically designed to cater to the unique demands of IoT applications. These mechanisms operate in conjunction with short-range wireless and traditional cellular technologies to facilitate connectivity for low data rates and low-power devices, which are not supported by conventional technologies. LPWA technologies have great potential for applications like remote wellness monitoring and innovative health systems. These systems integrate WSNs to transmit and receive information through LoRa wireless links. Delay-tolerant applications that necessitate low power consumption, low data rates and minimal costs are especially well-suited for LPWA technologies, as depicted in Figure 2 [45].
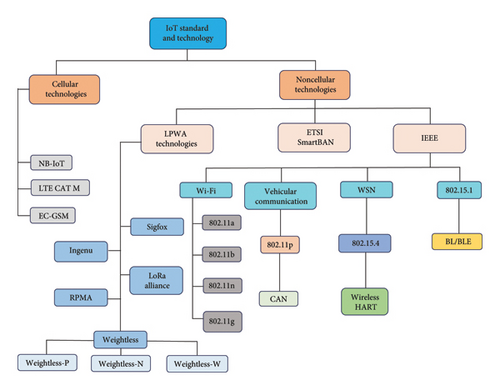
Noncellular LPWA technologies include Sigfox, Ingenu, LoRa Alliance, RPMA and Weightless, which are further subdivided into Weightless-P, Weightless-N and Weightless-W. The European Telecommunications Standards Institute (ETSI) has established a standard for SmartBANs that focuses on advancing communication technologies for health, wellness and personal safety. SmartBAN aims to fulfil the demand for low-power, reliable and secure wireless communication among devices that are worn on or around the human body. These networks are particularly relevant in healthcare applications, where wearable sensors monitor vital signs and transmit data to centralised monitoring systems [42].
IEEE Standards cover a wide range of technologies such as Wi-Fi (802.11a, 802.11b, 802.11n and 802.11g), vehicular communication (802.11p, CAN), WSN (802.15.4, Wireless HART) and BL/BLE.
Cellular technologies include NB-IoT, LTE CAT M and EC-GSM. These technologies highlight the diverse array of standards and technologies employed in IoT-based healthcare systems, classifying them and subcategories to enhance understanding and facilitate implementation [46]. LPWA technologies, such as LoRa, Telensa, Sigfox, Weightless SIG and Ingenu, compete by offering low-power operation, LoRa coverage and high scalability. A detailed comparison of these competing technologies is provided in Table 2.
| Technologies | Sigfox | Ingenu | Lora alliance | RPMA | Weightless-P | Weightless-N | Weightless-W | ||
|---|---|---|---|---|---|---|---|---|---|
| LPWA technologies | Parameter | Modulation | DBPASk/UNB/GFSK | CDMA/RPMA-DSSS | CSS | CDMA/RPMA-DSSS | QPSK/GFMK | GFSK | DBSK/16-QAM/BPSK/QPSK |
| Bandwidth | 100 GHz | 2.4 GHz | 125–500 kHz | 80 kHz | 6–8 MHz | 12.5 kHz | 470–790 MHz | ||
| Data rate | 10–100 bps | 8 bps–8 kbps | 0.3–500 kbps | 624 kbps | 200 bps–100 kbps | 30 kbps–100 kbps | 1 kbps–10 Mbps | ||
| Range | 50 km | 10 km | 15 km | 10 km | 2 km | 3 km | 5 km | ||
| Topology | Star | Tree/star | Star on star | Tree/star | Star | Star | Star | ||
| Link symmetry | No | No | Yes | No | NA | Uplink only | NA | ||
| Devices per access point | 1 million | ≤ 500,000 | 1 million | ≤ 500,000 | Unlimited | Unlimited | Unlimited | ||
| MAC | Unslotted Aloha | CDMA | Un-slotted aloha | CDMA | TDMA/FDMA | Slotted aloha | TDMA/FDMA | ||
| Battery life | 10 years+ | 20 years+ | 105 months | 10 years+ | NA | NA | NA | ||
| Encryption | No encryption | AES 256b, 16b Hash | AES 128b | AES 256b, 16b Hash | AES 128/256b | AES 128b | AES 128b | ||
| Mobility | No | Yes | Yes | Yes | Yes | Yes | Yes | ||
| Location | No | Yes | Need GPS | Need GPS | No | NA | NA | ||
| Over-the-air update | No | Yes | Yes | Yes | Yes | No | NA | ||
Figure 2 categorises various IoT standards and technologies into two primary groups: noncellular and cellular technologies.
2.8.1. Sigfox
Sigfox technology uses an ultra-narrow band (UNB) in the sub-GHz ISM band [47], allowing efficient communication in smart healthcare devices. With channel bandwidths of less than 1 kHz, Sigfox achieves ultra-low power consumption, minimal noise levels, maximum data throughput of 100 bps and high receiver sensitivity, making it an ideal choice for healthcare applications. Binary phase shift keying (BPSK) modulation ensures low power usage. While Sigfox offers a low data rate, it operates on a star topology network and supports uplink communication in its initial version. The latest version now supports bidirectional communication through asymmetric links [48]. This minimal data transmission benefits IoT healthcare applications such as alerting rescue services, heart rate (HR) monitoring and alarm systems, which previously relied on one-way communication.
2.8.2. Ingenu
Ingenu, or On-Ramp Wireless, operates within the Industrial, Scientific and Medical (ISM) band at 2.4 GHz. This technology offers higher throughput, transmission power and capacity than other healthcare technologies, which commonly utilise the sub-GHz band. It is important to note that Ingenu’s shorter range may pose a greater interference risk than LoRa and Sigfox in healthcare devices and sensors. Ingenu leverages a patented access scheme called Random Phase Multiple Access (RPMA), which utilises direct-sequence spread spectrum (DSSS) technology to ensure high receiver sensitivity and robust power control in healthcare applications [49]. RPMA enables large-area coverage at minimal costs, high capacity, extended battery life and enhanced security. The impressive receiver sensitivity ensures substantial capacity, effectively accommodating numerous end devices in healthcare applications.
2.8.3. Weightless
Weightless is an open-source LPWA protocol widely used in healthcare. It operates on an unlicensed sub-Gigahertz (sub-GHz) spectrum and includes three different protocols—Weightless-W, Weightless-N and Weightless-P—each with varying ranges, power consumption and features [50].
2.8.3.1. Weightless-W
Weightless-W supports various modulation techniques, such as Differential-BPSK (DBPSK) and 16-Quadrature Amplitude Modulation (16-QAM), and operates within the TV white space spectrum, utilising a wide range of spreading factors (SF). This enables a high data rate of 1 kbps to 10 Mbps, making it well-suited for healthcare applications. Although Weightless-W operates in narrowband with low power consumption, thus improving battery life, its usage is restricted to specific regions, particularly within European healthcare systems, which limits its widespread adoption [51].
2.8.3.2. Weightless-N
The Weightless-N system utilises a star topology featuring one-way communication, which is particularly well-suited for healthcare systems requiring extended battery life of up to 10 years and cost-effective network solutions. Weightless-N leverages a differential binary-shift keying (DBSK) modulation technique and operates on an UNB sub-GHz frequency, effectively reducing interference in healthcare networks by employing a frequency hopping algorithm. Moreover, it provides support for mobility in healthcare applications.
2.8.3.3. Weightless-P
Weightless-P has been specifically developed to facilitate bidirectional communication within healthcare systems and uses modulation techniques such as Quadrature Phase Shift Keying (QPSK) and Gaussian Minimum Shift Keying (GMSK). This protocol guarantees high network reliability, performance and security, aligning with a 3G Partnership Project (3GPP) standard. It provides data rates ranging from 0.2 kbps to 100 kbps at a reduced cost compared to other LPWA technologies. Additionally, Weightless-P supports over-the-air firmware updates and dependable bidirectional data transfer for healthcare applications.
2.8.4. LoRa Alliance
The LoRa technology, a part of the low-power wide area network (LPWAN) solution, consists of two main elements: LoRa and LoRa wide area network (LoRaWAN) [52]. Operating on the sub-GHz ISM band, LoRa operates at the physical (PHY) layer and utilises chirp spread spectrum (CSS) modulation for healthcare applications. This modulation widens a narrowband channel into a broader bandwidth, improving signal detection and communication efficiency in healthcare networks. LoRa offers six orthogonal SF that are chosen based on the specific requirements of the healthcare application, thereby enabling enhanced spectral efficiency and network capacity. Additionally, LoRa incorporates a cyclic error-correcting scheme designed to improve communication robustness in healthcare systems.
LoRa is well-suited for transmitting healthcare data at rates ranging from 300 bps to 5000 bps, outperforming Sigfox concerning data rate. However, one significant limitation of LoRa is its dependence on a single-vendor subscription, Simulation Technology (SimTech), which results in high costs.
2.8.5. RPMA Technology
RPMA technology, based on the IEEE 802.15.4k standard, is extensively utilised in the healthcare industry [53].
As previously mentioned, Ingenu provides data rates that surpass those of other systems, such as LoRa and Sigfox, albeit at a higher cost and with reduced battery life for healthcare devices. Unlike LoRa and Sigfox, Ingenu incorporates tracking standards such as the Global Navigation Satellite System (GNSS) to track healthcare applications with LoRa and Sigfox while using a separate module. Sigfox only supports one-way communication, and Ingenu enables bidirectional communication within healthcare systems. Nonetheless, Sigfox and LoRa enjoy broader user adoption and base station support, making Ingenu a less favoured option for large-scale healthcare systems.
2.9. ETSI: SmartBAN
In 2013, ETSI established a technical committee (TC) to develop a SmartBAN, a new protocol specifically tailored to the unique requirements and constraints of wearable wireless sensor networks (W-WSNs) in the healthcare sector. This new specification includes the PHY layer and medium access control (MAC) layer [54] and is designed to address the specific needs of the healthcare industry. While the TC completed the initial framework in December 2014, the detailed specification has faced publication delays by ETSI. The initial technical requirements for WBAN parameters proposed by TC SmartBAN are outlined in Table 2.
Healthcare solutions leveraging SmartBAN technology enable body-to-body communication, on-body connections and seamless integration with embedded devices. SmartBAN adopts a multiradio approach, facilitating connectivity among healthcare devices through diverse radio protocols. Operating in the ISM band with frequencies ranging from 2.401 to 2.481 GHz, SmartBAN employs Gaussian frequency shift keying (GFSK) modulation. Furthermore, it utilises benign cephalic histiocytosis (BCH) coding (127, 113) to minimise errors and bolster the reliability of repetition codes in healthcare applications when necessary.
Table 3 outlines the SmartBAN healthcare protocol, comprising two channels: the data transmission and network control channels. The network control channel offers several benefits, including seamless BAN-to-BAN communication and rapid acquisition of channels in healthcare applications. Notably, any significant modifications to the healthcare control channel, such as interference or node association, do not impact healthcare data transmission [6].
| Parameter | SmartBAN requirement |
|---|---|
| Latency | < 125 ms |
| Range | < 1.5 m |
| Maximum node capacity | 16 > 18 nodes |
| Reliability | Robustness to multipath interference and shadowing |
| Quality of service control |
|
| Network topology | Star network |
| Transmission rate in a physical layer | Up to 1 Mbps |
| Data rate sensor | Signal monitoring nominally less than 100 kbps/node |
| Robustness/coexistence | Lower interface to other systems and high tolerance to interference are good |
The transmission of healthcare data is segmented into the inter-beacon interval (IBI), which comprises the control and management period (CMP), the inactive period and the scheduled access period (SAP). Time division multiple access (TDMA) is utilised during the SAP to prevent collisions in healthcare data transmission [21]. The CMP manages healthcare data and control transmissions using a slotted Aloha system. Moreover, the multiuser channel access (MCA) mode is an alternative protocol that prioritises transmitting high-priority messages, such as emergency packets, which are time-sensitive and crucial for low-latency healthcare applications [55].
2.10. IEEE
A diverse array of standards from the IEEE Standards Association (IEEE-SA) have been put forward and executed to address various requirements in healthcare applications, as detailed in Table 4. Protocols such as 802.11, 802.11b, 802.11a, 802.11p, and 802.11n are employed for healthcare-associated wireless fidelity (Wi-Fi) and vehicular communication. Furthermore, IEEE Standards, including 802.15 WSN, 802.15.1 BL, and 802.15.1 BLE, are utilised for short-range communication in the healthcare domain. The IEEE 802.15.1 standard has gained prominence for medical and wearable sensing devices, as discussed in Table 2. Nevertheless, many of these communication models were not explicitly tailored for wearable wireless sensor systems in the healthcare sector.
| Technology | Wi-Fi | Vehicular communication | WSN | 802.15.1 |
|---|---|---|---|---|
| Security | AES encryption | Vulnerabilities’ security with light visible communication | AES encryption | AES encryption |
| Modulation | DSS | 16-QAM, 64-QAM, BPSK and QPSK | MSK | Adaptive frequency hopping |
| Network topology | Star/mesh | Mesh | Star/mesh | Star |
| Throughput | 0.1 Mbps | 27 Mbps | 163 kbps | 0.2 Mbps |
| Data range | 10–200 m | 305–1000 m | 75 m | 10–100 m |
| Data rate | 250 kbps | 3–27 Mbps | 40–250 kbps | 1 Mbps |
| Frequency | 2.4 GHz | 5.9 GHz | 2.4 GHz | 2.4 GHz |
2.10.1. Wi-Fi
The IEEE Standards 802.11a, 802.11b, 802.11g, 802.11ac, and 802.11n are utilised for short-range healthcare communication across various frequency bands but often lack interoperability, as illustrated in Figure 2 [56]. These standards do not accommodate WLAN adaptation for business needs; instead, they primarily focus on the healthcare protocol model’s PHY and data link layers. In the healthcare environment, the local area network (LAN), including its operating systems, applications and protocols such as Novell NetWare and TCP/IP, operates over the 802.11 wide area network (WAN) via Ethernet, as elaborated in Table 4.
2.10.1.1. The 802.11a Standard
This wireless standard provides a maximum speed of 54 Mbit/s, which was considered the fastest at the time for healthcare applications. Operating in the 5 GHz band, it facilitates swift data transfer. However, its signal range is confined to 35 m in healthcare settings. Despite this limitation, it is characterised by reduced interference, offering a more reliable connection with minimal congestion in healthcare networks.
2.10.1.2. The 802.11b Standard
The 802.11B standard operates at a 2.4 GHz frequency, offering a limited signal range of 35 m and a maximum data rate of 11 Mbit/s. It enables healthcare network-independent access to radio waves and other devices, facilitating data transfer in LAN environments. This standard enhances healthcare networks’ availability, performance and throughput via Ethernet, serving as the final link between clients, servers, devices and wired networks [57].
2.10.1.3. The 802.11g Standard
The 802.11G standard represents a significant enhancement over its predecessors. Operating at 2.4 GHz with a data rate of 54 Mbit/s, it boasts a robust signal range of up to 40 m, making it well-suited for healthcare IoT networks. Renowned for its speed, stability and efficient data transfer capabilities, this standard excels in weather penetration. It is ideal for remote sensing and Radio Detection and Ranging (RADAR) communication in healthcare applications.
2.10.1.4. The 802.11n Standard
The IEEE-SA has developed a comprehensive set of standards for healthcare applications, detailed in Table 4. Wi-Fi protocols such as 802.11, 802.11b, 802.11a, 802.11p, and 802.11n are utilised in healthcare settings and for vehicular communication. Furthermore, IEEE Standards, including 802.15 WSN, 802.15.1 BL and 802.15.1 BLE, are extensively employed for short-range communication in healthcare. The 802.15.1 standard has gained significant traction for medical and wearable sensing devices. Nonetheless, several communication models were not initially designed for wearable wireless sensor systems in healthcare. IEEE Standards like 802.11a, 802.11b, 802.11g, 802.11ac, and 802.11n offer short-range communication for healthcare applications across various frequency bands, but they often lack interoperability, as depicted in Figure 2 [58]. These standards primarily focus on the PHY and data link layers, supporting LAN healthcare operations and interfacing with WAN through Ethernet, as specified in Table 4 [59].
2.10.2. Vehicular Communication
The IEEE 802.11p standard, as detailed in Table 4, is widely utilised regarding healthcare vehicular communication. This standard offers a cost-effective solution, guaranteeing dependable message delivery, resistance to electromagnetic field (EMF) noise and nonconflicting message transmission.
2.10.2.1. IEEE 802.11p
The IEEE 802.11P standard introduces Dedicated Short-Range Communication (DSRC) at the PHY layer, utilising Orthogonal Frequency Division Multiplexing (OFDM) for data transmission. It is effective in healthcare settings with multipath fading and offers high spectral efficiency. With the capability to support speeds of up to 200 km/h, this protocol is well-suited for healthcare vehicular communication [42].
2.10.2.2. Controller Area Network (CAN)
CAN is a message-oriented serial communication protocol used in healthcare transportation. It includes CAN controllers and transceivers connected to the data link and application layers. CAN offers high reliability, speed, security, and real-time functionality for healthcare modules and devices [60].
2.10.3. WSN
WSNs are integral to IoT and cyber-physical systems in healthcare. They provide energy-efficient and secure communication while enabling wireless monitoring of healthcare sensors for temperature, blood flow and other metrics [61]. These networks reduce system complexity and cost while enhancing healthcare environments with low-powered, inexpensive devices.
2.10.3.1. IEEE 802.15.4
The IEEE 802.15.4 standard targets the PHY and MAC layers of low-rate wireless personal area networks (LR-WPAN) for short-distance communication in healthcare. Although it provides secure services, it lacks device authentication and key management, compromising privacy and integrity [62].
2.10.3.2. Wireless HART
Built on top of IEEE 802.15.4, Wireless HART adds a MAC layer standard using TDMA for secure and reliable communication in healthcare. It employs advanced encryption and message integrity checks, making it highly safe for healthcare applications [63].
2.10.4. IEEE 802.15.1
The IEEE 802.15.1 BL standard is used for short-range healthcare communication, with connectivity distances ranging from 10 to 100 m [64]. It operates in the unlicensed 2.4 GHz ISM band and uses frequency hopping spread spectrum (FHSS) to reduce interference from other wireless services. BL enables remote communication between healthcare devices, offering reliable and low-cost data transmission.
2.10.4.1. BL
BL is a low-power, short-range wireless communication technology that supports fast and convenient healthcare data transmission. It uses minimal power, operating at 10.1 μA and 3.3 V in 120-s intervals, which includes waking and sleeping periods [65] for connecting to a wireless hub. BL-based healthcare monitors use IoT sensor nodes for data transmission [66,67]. With low data rates and short-range capabilities, BL is ideal for transmitting healthcare data to wireless base stations or hubs [68,69].
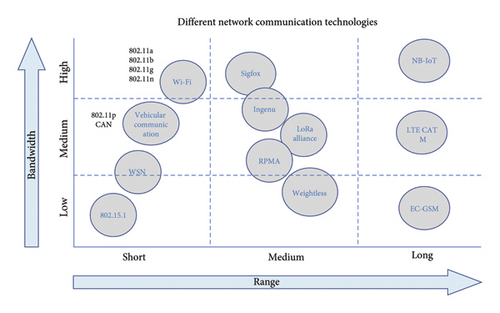
Figure 3 compares various network communication technologies based on their bandwidth and range. Short-range, high-bandwidth technologies include Wi-Fi (802.11a/b/g) and vehicular communication (802.11p, CAN). Medium-range technologies include Sigfox, Ingenu, LoRa Alliance, RPMA and Weightless, while LoRa, low-bandwidth technologies include NB-IoT, LTE CAT (M) and EC-GSM [70].
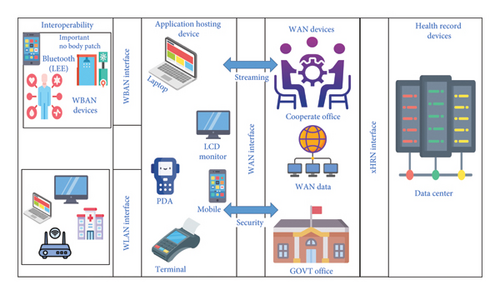
2.11. IoTNet Structural Design
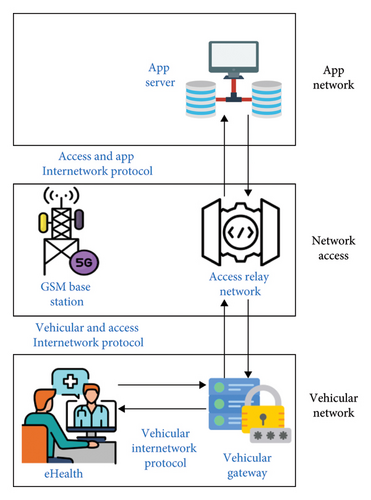
The structural design of IoTNet pertains to the arrangement of its physical components, functional grouping and operational principles. Figure 4 illustrates a fundamental reference structural scheme for telehealth and ambient assisted living (AAL) systems proposed by the Continua Fitness Association. An essential aspect of this design is the interception of IoT gateways, the wireless local network/WPAN interactive programme and the encrypted communication between IoT gateways and caretakers. Multiple studies [71] have affirmed that IPV6-centred 6LoWPAN is the foundation for IoTNet.
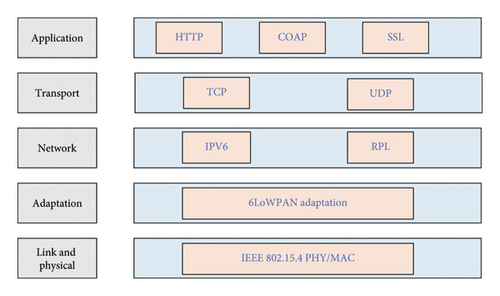
The layered structure of 6LoWPAN, as delineated in reference [47], is depicted in Figure 4. In IoTNet essentials, sensing devices and wearables use IPv6 and the 6LoWPAN system for transmitting data over the IEEE 802.15.4 protocol. Data from sensors are transmitted using the User Datagram Protocol (UDP) [57]. However, 6LoWPAN has limitations, particularly its lack of support for mobile IPv6, a subset of the IPv6 protocol enabling mobility. To mitigate this issue, a protocol has been proposed for message exchanges between a mobile victim node, the core network and the target network [72].
The management of mobility is addressed in [44], where four alternative methods are discussed. These methods entail asking routers to wait for a new address, cyclically sending diagram information, connecting to nearby nodes and sending DAG information solicitation messages. Among these approaches, router solicitation and message exchange are considered the most efficient as the mobile node initiates them. Furthermore, a specific entry point for shared medical services is detailed in [73], outlining handling episodic traffic using heterogeneous networks (HeTNet). A comprehensive eHealth service delivery method, consisting of three stages, has been proposed in [74].
Figure 4 illustrates the IoT protocol stack specifically designed for healthcare applications. The stack is segmented into several layers, each responsible for different communication and data management aspects within an IoT healthcare network. The network architecture consists of layers such as the application layer, encompassing protocols such as HTTP, Constrained Application Protocol (CoAP) and Secure Sockets Layer (SSL), which manage end-user interactions and ensure secure communication. The transport layer is responsible for data transport between devices using protocols like Transmission Control Protocol (TCP) and UDP [75]. The network layer includes IPv6 and IPv6 routing protocol (RPL), which handle the network’s addressing and routing of data packets. The adaptation layer incorporates 6LoWPAN to transmit IPv6 packets over low-power networks efficiently. The link and PHY layer operate the IEEE 802.15.4 standard, providing the specifications for LR-WPANs [76].
The establishment of signals and the transfer of data form the cornerstone of the complex infrastructure of IoTNet and underpins the quality of service (QoS) agreements and resource-sharing mechanisms. Signal protocols are critical in facilitating efficient communication and resource management within the network.
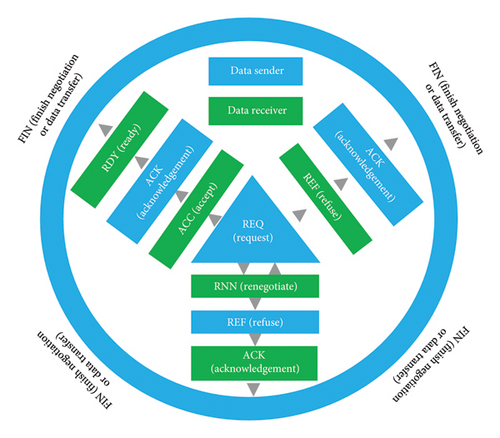
The data transfer process in the context of IoT-based healthcare systems as seen in Figure 5 emphasises the interaction dynamics between the data sender and receiver. The sequence commences with the data sender initiating a request (REQ) to transfer data. Subsequently, the receiver acknowledges (ACK) the REQ and indicates readiness (RDY) to receive the data. The data transfer process commences upon acceptance (ACC) of the REQ. The system may undergo various stages throughout this progression, such as renegotiating (RNN) and refusing (REF) based on its conditions and requirements. The outer circle symbolises the comprehensive data transfer cycle, which commences and culminates with negotiation or the completion of data transfer (FIN).
Integrating medical tools into vehicular networks has facilitated the transmission of health data over the IPV6 application server [77]. A lightweight authentication procedure for vehicle-to-infrastructure (V2I) communication in IoTNet is illustrated in Figure 6. This procedure utilises an IPV6 direct route as predefined in the routing table, offering a range of IPV6 addresses for healthcare equipment within vehicles.
The potential of data analytics to revolutionise information structures in healthcare facilities is expounded upon in [61]. Additionally, synchronising various communication standards to bolster IoTNet growth is deliberated in [78], while the record delivery architecture in cloud computing integration is scrutinised in [40]. Subsequently, the following section delves into the IoTNet policy configuration, encompassing the structural design and the operational framework.
3. IoTNet in Healthcare System
This review highlights the potential impact of IoTNet in the healthcare sector, emphasising its capacity to facilitate remote monitoring, seamless data integration and personalised healthcare solutions. Various components of IoTNet, including intelligent medication packs, wearable devices and cloud platforms, collectively contribute to a holistic approach that enhances healthcare delivery through IoT technologies. Notably, the proposed architecture in [75] serves as a robust foundation for cultivating a deeper comprehension of the IoT system.
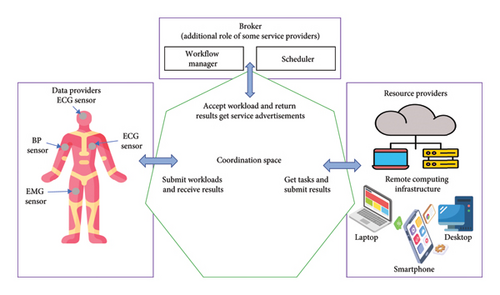
3.1. IoTNet Topology
The IoTNet topology describes the interplay among various modules within an IoT-based healthcare network, illustrating how these components collaborate within a cohesive environment. Figure 7 depicts how a computational system acquires a substantial volume of sensor data, encompassing blood pressure (BP), body temperature, electrocardiograms (ECG) and oxygen saturation levels, forming a prototypical IoTNet topology. This system leverages the computational and storage capabilities of stationary and mobile electronic devices, including laptops, smartphones and medical stations, to establish a unified computational grid [79,80]. Figure 6 portrays a scenario wherein portable medical devices capture a patient’s health data, vital signs and sensors affixed to the patient’s person. The collected data are subjected to analysis and storage, making them vulnerable to aggregation from diverse devices and apparatus. Through this process of aggregation and monitoring, healthcare providers can remotely oversee the patient from any location and respond appropriately.
The categorisation of IoT standards and technologies in Figure 6 distinguishes cellular and noncellular technologies. Noncellular technologies encompass LPWA technologies such as Sigfox, Ingenu, LoRa Alliance, RPMA and Weightless, in addition to ETSI SmartBAN and IEEE Standards (Wi-Fi, Vehicular Communication, WSN, 802.15.1). On the other hand, cellular technologies include NB-IoT, LTE CAT M and EC-GSM. Within healthcare environments, a broker oversees workflow and scheduling to ensure the efficient submission of tasks, workload management and timely result delivery. Furthermore, the network topology supports essential network structures, enabling the transmission of medical videos, such as ultrasound video transmission over a unified network employing Worldwide Interoperability for Microwave Access (WiMAX), an Internet Protocol (IP) network and a Global System for Mobile (GSM) network with a standard gateway and admission facilities network. This analogous structure is detailed in [81].
Figure 8 illustrates an IoT-based healthcare system incorporating on-body sensors for real-time monitoring and remote healthcare management. The system consists of several key components and their interactions such as on-body sensors that are attached to various points on the patient’s body, continuously monitor vital signs and health metrics [82]. 6LoWPAN Edge Router is a component in networks that use the 6LoWPAN protocol. 6LoWPAN enables IPv6 communication over low-power wireless devices, typically in constrained environments like sensor networks, smart homes or industrial IoT applications. The 6LoWPAN router acts as an intermediary, facilitating the connection between a 6LoWPAN network and other IP-based networks, such as the Internet or more extensive LANs. TinyOS is an open-source, lightweight operating system designed for low-power, resource-constrained devices in WSNs and embedded systems. Initially developed at the University of California, Berkeley, TinyOS provides a flexible and efficient platform for microcontroller-based devices that operate under stringent memory, power and processing limitations. The event-driven system responds to external events (such as sensor inputs) and optimises energy consumption by sleeping between events to conserve power and the data are transmitted over the IP network to ensure local and global connectivity.
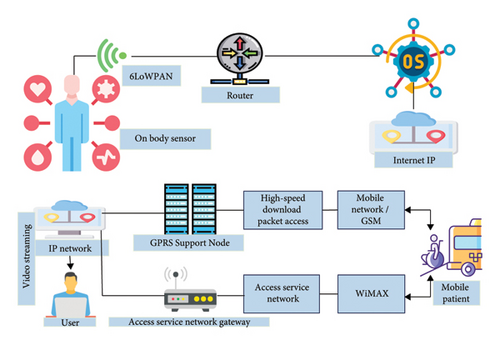
Expert Station is a pivotal component in modern healthcare networks, designed to enhance clinical decision-making and patient outcomes by integrating specialised knowledge and advanced technology. This digital platform connects healthcare professionals with experts across various medical fields, enabling real-time consultations, second opinions and access to the latest research and treatment protocols by facilitating seamless communication between primary care providers and specialists. Expert Station promotes a collaborative approach to patient care, ensuring medical decisions are informed by the most current and comprehensive information available. The GPRS Support Node (GSN) and the Access Service Network (ASN) Gateway are critical components in the mobile healthcare ecosystem, facilitating efficient communication and data transmission between healthcare devices and systems.
Mobile patients leverage mobile technology and healthcare applications to manage their health and medical needs. This growing trend has transformed the landscape of healthcare delivery, enabling patients to access information, communicate with healthcare providers and monitor their health conditions from anywhere.
This setup integrates various communication technologies and network protocols, creating a seamless and efficient healthcare monitoring system supporting stationary and mobile patients. Additionally, intelligent pharmacological packing (iMedPack) plays a crucial role as an IoT device in addressing medication adherence issues and ensuring proper pharmacological compliance [83].
iMedPack interfaces healthcare systems, integrating various sensing instruments and interfacing with multiple wireless protocols. It wirelessly connects several wearable sensing tools and IoT devices to healthcare gateways, establishing a link between the patient’s environment and a fitness IoT cloud within a HeTNet. This configuration enables comprehensive medical analysis and other health-related monitoring. The gateways can independently analyse, store and display complete patient data, as depicted in Figure 9 [84].
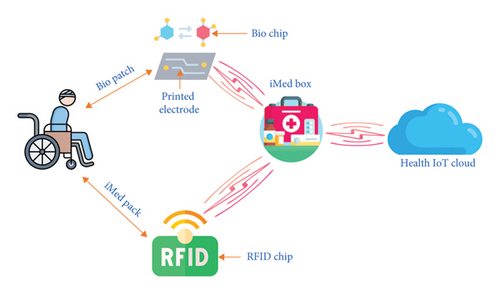
Figure 9 depicts a health monitoring system architecture, where various components are connected through an IoT network to facilitate real-time health data tracking and analysis. The breakdown of the system begins with a BIO Patch, which consists of a BioChip and Printed Electrode, which adheres to the patient’s body to collect vital signs. The BioChip processes the biological signals captured by the Printed Electrode. The BIO Patch wirelessly transmits data to the iMed Box, a central device for gathering and processing health information. Represented by a medical kit icon, the iMed Box plays a crucial role in managing patient health data. The iMed Box connects to the Health IoT Cloud, a cloud-based platform that stores, analyses and enables remote monitoring of the collected health data. It provides real-time insights into the patient’s health status. The iMed Box is linked to the iMed Pack via an RFID Chip, and the iMed Pack likely stores medication or medical supplies. The RFID Chip enables tracking and adequately managing these supplies, ensuring they are dispensed accurately. This iMed Pack also incorporates CDM, designed to maintain the integrity and quality of the pack’s contents, potentially ensuring the medication’s effectiveness and safety. This system exemplifies the integration of IoT technologies in healthcare, enhancing real-time monitoring and efficient management of medical supplies and patient care. Healthcare workflows, particularly in pre- and post-treatment phases, often involve providers with the healthcare facility’s overall infrastructure. These operations have been exemplified in alternative medical facility contexts [64]. Additionally, a universal fitness care IoTNet topology with cloud computing capabilities has been proposed [56], adopting a traditional full-mesh networking scheme with pervasive internet connectivity.
The topology must also incorporate a medical regulation system within the framework of a semantic medical monitoring scheme, as portrayed in Figure 10 [85]. This ensures a comprehensive and adaptable approach to managing healthcare data and patient care in real time.
3.2. IoTNet Platform
The IoTNet framework integrates the network model and computational platform, as depicted in Figure 11. The diagrams in (A) simplified and (B) detailed formats illustrate the roles and interactions between various stakeholders in IoT healthcare services, including healthcare suppliers, application designers, platform providers, content providers, telecom operators, patients and healthcare service providers [86]. These diagrams highlight the complex network of interactions involved in delivering healthcare services through IoT.
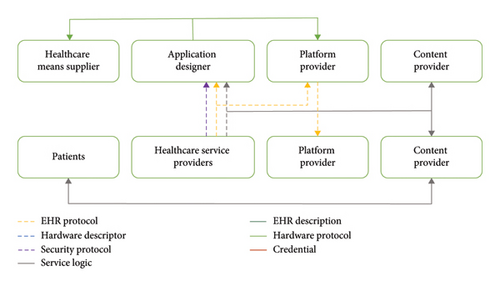
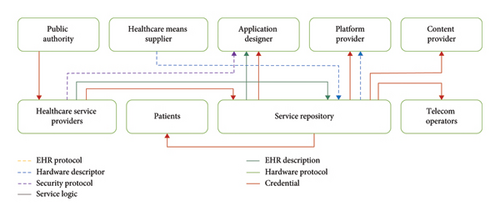
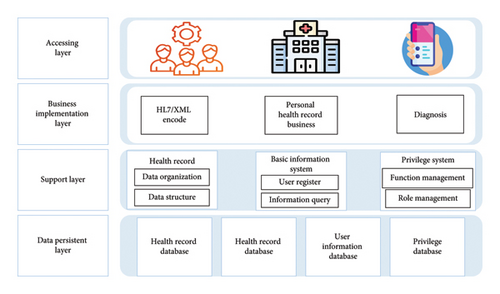
The IoT Healthcare Information System structural design is outlined in a layered model in Figure 12 in which caretakers and agents can access records from the application level, facilitated by a service layer. A similar concept of a data centre platform acting as middleware between smart devices and the business level is discussed in [87]. The importance of managing information through IoTNet stakeholders to build an open platform is emphasised in [44]. As shown in Figure 13, three classifications of edge standardisation are proposed to create a friendly ecosystem, covering tangible and nontangible elements, electronic health record (EHR) formats and security systems, ensuring proper interception and data management.
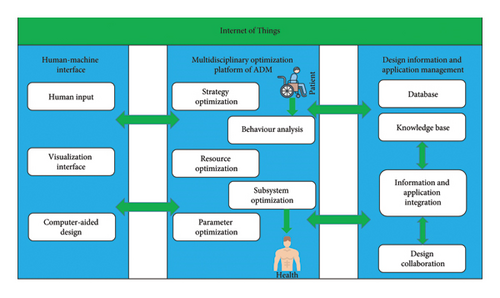
The publication ‘A Comprehensive Automatic Structural Methodology (ASM) Platform for IoTNet’ elaborates on a structural design for IoTNet, explicitly focusing on reintegration purposes. It sought to elucidate HCIs, multidisciplinary minimisation and application administration [88]. The publication also explores the utilisation of ‘VIRTUS’, based on the XMPP standard for real-time messaging, even under suboptimal network conditions. Furthermore, it presents a methodology for IoT gateways to manage multiple users and devices. It offers a systematic approach to acquiring fitness data, transmitting it to a router and conducting analysis within a structured database.
A three-level cloud platform has been developed to access cloud data over IoTNet [89]. The tenant database manages data access, while the business level plays a crucial role in data distribution and interoperation. Specific mechanisms are utilised to process different healthcare records, as investigated in [90], although these studies have not provided a complete scenario. A semantic platform architecture is also outlined in [91], ensuring semantic interoperability across various systems and devices, thereby enhancing user experiences.
The environment, domestic equipment and specific semantic capabilities form a system where the semantic layer supports four categories of ontologies.
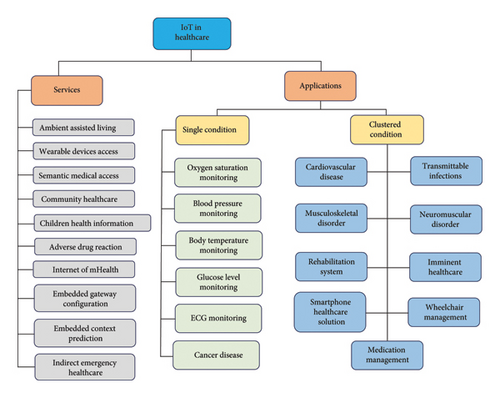
4. IoT Healthcare Services and Applications
IoT technology in healthcare involves paediatric and elderly care, chronic disease monitoring and remote health supervision. These systems are categorised into services and applications, divided into single-condition (focussed on specific ailments) and multiple-condition (addressing various diseases) categories. The classification framework in Figure 14 reflects current IoT healthcare solutions and has the potential for expansion to encompass new services and applications. Figure 15 provides an overview, interconnecting various IoT services (AAL, semantic medical access (SMA), children’s health information and adverse drug reactions (ADRs)) and applications (oxygen saturation monitoring, BP monitoring, glucose level sensing and ECG monitoring) to healthcare outcomes such as cardiovascular diseases (CVDs), transmittable infections [92] and neuromuscular disorders. This illustrates the interrelatedness of IoT services and applications in enhancing healthcare outcomes.
4.1. IoT Healthcare Services
The IoT is designed to support diverse healthcare facilities offering various healthcare solutions. However, a clear distinction between IoT services and solutions is lacking. Sometimes, a service may not be readily separable from a specific solution or application.
4.1.1. AAL
Traditionally, neither smart homes nor specific IoT-based medical facilities are designed to provide specialised services for older people; thus, a dedicated IoT service is required. AAL refers to an IoT platform driven by AI designed to cater to the healthcare needs of elderly individuals. The goal of AAL is to extend the ability of older adults to live independently and safely in their own homes. AAL services can enhance their autonomy and offer human-like support, helping them manage various difficulties.
A flexible design aimed at automating, securing, regulating and facilitating communication within IoT-based AAL is outlined in [93]. This design is intended to serve as a blueprint for delivering healthcare services to the elderly and injured. It utilises 6LoWPAN for live communication, facilitating passive communication through RFID and NFC. Furthermore, the design incorporates an algorithm based on medical knowledge to identify challenges elderly individuals face. The significance of the AAL model within IoT frameworks is a topic of debate [94], with some arguing that combining KIT smart objects and narrow-hop services can support AAL. This subsequent framework enables interaction between stakeholders, including older people, caregivers, doctors and family members.
These initiatives have stimulated the development of standards for KIT smart objects and narrow-loop healthcare services driven by IoT. To this end, an open, secure and flexible IoT framework and cloud computing have been proposed [95]. This framework addresses various challenges related to interception, security, QoS streaming and data storage, and its feasibility has been validated through the implementation of IoT-based health services on a computer. Earlier studies underscored the necessity for AAL and similar technical support, outlining a roadmap for advancing AAL technology [95]. Additionally, [96] explores an IoT-based secure system for AAL-focused medication management.
4.1.2. Wearable Device Approach (WDA)
Many noninvasive sensing devices have been developed for different medical applications, particularly WSN-cantered healthcare services [97]. These devices have the necessary capabilities to integrate into the IoT framework [98]. The combination of wearable sensors and medical devices presents new challenges for researchers and designers working on integration [99]. A dedicated service called the WDA is crucial [100]. Wearable devices are integrated into WSN-based applications for IoT scenarios, as shown in [101]. This process outlines a system for various healthcare applications, including mobile computation tools like smartphones and smartwatches. A motion detection system for remote monitoring using wearable devices is presented in [102], and the use of BLE to enable a WBAN for wearable devices is explored in [98].
4.1.3. SMA
The use of semantics and ontologies to distribute large volumes of medical information has been extensively researched [82]. Semantics and ontology-based systems are crucial in IoT-centred healthcare applications. Integrating medical semantics and ontologies into the IoT framework requires a specific service called SMA. A semantic medical monitoring system using IoT sensors is presented in [103]. This system incorporates a medical regulation engine to analyse a large volume of sensor data stored in the cloud. A pervasive system for collecting and interoperating IoT data to support healthcare services is detailed in [41].
4.1.4. Social Healthcare (SH)
SH involves creating interconnected networks within communities, which include urban hospitals, residential areas and rural societies. IoT-based systems support these networks and operate collaboratively as a SH system. An effective IoT platform has been proposed for monitoring rural healthcare [104]. Comprehensive verification and approval processes are essential for SH networks, which integrate WPANs to facilitate SH. This interconnected medical network is sometimes called a ‘virtual hospital’, enabling the sharing of health information among medical institutions. A local health information system utilising a four-level infrastructure is demonstrated in [105].
4.1.5. Children’s Health Information
Raising awareness about children’s health and educating the public, including children themselves, about cognitive and behavioural health issues is crucial [106]. This has led researchers to develop an IoT-based health system called Child Health Information, dedicated to children’s health. In this system, a paediatric representation offers tools for educating, entertaining and empowering hospitalised children, as discussed in [107]. Additionally, IoT-based mobile health (m-health) services encourage children to adopt healthy habits with the support of teachers and families.
4.1.6. Indirect Emergency Healthcare (IEH)
Natural disasters, transportation accidents and fires require specialised healthcare responses. In this context, a dedicated service called IEH offers resource availability, real-time updates, postdisaster actions and data protection. Despite the lack of substantial research in this area, IEH can address critical emergency healthcare needs through IoT-based systems [75].
4.1.7. ADR
ADR denotes the harm caused by the consumption of medication, either immediately or over time, or as a consequence of drug interactions. Given the ubiquity of ADR, it is imperative to devise pragmatic solutions for its management. As described in [71], an IoT-based optical mark recognition (OMR) system has been developed to identify medication using NFC-enabled devices. Furthermore, the iMed Pack system integrates this technology with RFID and respiratory distress syndrome (RDS) automation to ensure medication safety [108].
4.1.8. The Internet of M-Health Equipment
M-health monitoring involves wearable medical devices and communication technology for healthcare services. Mobile Internet of Things (M-IoT) combines 6LoWPAN and 4G technologies to create a new healthcare infrastructure for future network-based m-health services. While m-IoT specifically focuses on IoT in healthcare, it also has characteristics related to global mobility. A system for noninvasive glucose monitoring and other m-health services is described in [109], and challenges related to the m-IoT ecosystem are discussed in [24].
4.1.9. Embedded Gateway Conformation (EGC)
EGC refers to a structural design that connects network nodes (where patients are directly connected), the internet (which connects servers and clients) and other medical devices. From a service perspective, EGC plays a crucial role in the healthcare system. An example of an EGC can be found in [110], where the system enables automatic and rapid monitoring through a private mobile gateway [111].
4.1.10. Embedded Context Predictions
To create context-aware healthcare applications over IoT networks, third-party developers require a general framework called the embedded context predictions service. This system, developed for ubiquitous healthcare, enables developers to build context-aware healthcare applications, as discussed in [112]. Further research is, however, needed in this area to develop robust context-aware IoT healthcare systems [113].
4.2. IoT Healthcare Application
In addition to IoT services, IoT applications essential in healthcare are discussed in Table 5. Professionals usually design services, while operators and patients use applications. Wearable devices and other healthcare products on the market can be considered IoT innovations contributing to different healthcare solutions. This section will delve into various IoT healthcare applications for individuals and groups, as shown in Table 5.
| Conditions/infirmity | The operation, roles and connection of sensors used in IoT |
|---|---|
| Wheelchair management | For wireless body area network sensors, pressure, ECG, accelerometer were used. It realises abnormality, processes node signals, wirelessly communicates with a sink node and perceives surroundings. It performs connectivity with heterogeneous data centre layers and smart devices |
| Medication management | It uses wireless sensors based on biomedical and delamination materials like humidity, touch and oxygen. Wearable sensors also record prognosis and diagnosis. It uses wireless links, multimedia transmission, database access, GPS and web access for connectivity |
| Rehabilitation system | There are many smart homes and wearable sensors. These sensors are used for tracking, detecting an event, coordination, feedback and cooperation with the system. It performs connectivity with wireless sensor devices and wireless networks that can access different points |
| Body temperature monitoring | It uses a wearable sensor for skin-based and body-based temperature measurements. It uses wireless body area networks to connect devices through a gateway |
| BP monitoring | It uses a wearable sensor for blood pressure, automated inflation and sociometric measurement. It uses wireless body area networks to connect devices through a gateway |
| Heart rate monitoring | Pressure, ECG and accelerometer. Circuit boards with fabricated electrodes printed on board with capacity for wireless body area network sensors. Data are transmitted with a wireless transmitter through digital chain connectivity. Wi-Fi and Bluetooth Low Energy (BLE) are connected with smart devices through a gateway |
| Advanced diabetes patient wound analysis | Image segmentation and decompression from a smartphone camera. To drive the IoT devices, smartphones on chip (SOC) was used to run the software platform |
| Diabetes | No intercourse opts for the physiological sensor. The Telosb mote is connected to sensor output that is used to convert an analogue signal into digital signals. For connectivity, it uses IP-based wireless nodes for wireless devices and sensors with the architecture of 6LoWPAN and IPV6 protocol |
| Remote surgery | It uses an augmented reality (AR) sensor and surgical robot system. A feedback-based sensor system and a master controller are used to ensure telepresence that gives feedback to the user. It performs information management systems and data connectivity in real time |
| Melanoma detection | It uses a built-in smartphone camera that takes images of cancerous skin and matches the pattern of the suspicious image. Smartphone on chip (SOC) was used to drive the IoT devices to run the software platform |
| Nose-related symptoms and allergic rhinitis | It uses a built-in smartphone microphone, a vector machine and speech recognition. Smartphone on chip (SOC) was used to drive the IoT devices to run the software platform |
| Cough detection | It uses a built-in smartphone microphone to classify rainforest machine learning and analyse recorded spectrograms and speech recognition. Smartphone on chip (SOC) was used to drive the IoT devices to run the software platform [114] |
| Cystic fibrosis, chronic obstructive pulmonary disease and asthma | It uses a built-in smartphone microphone. The air flow rate is calculated, and the flow of time, flow volume graphs and volume time are produced. Smartphone on chip (SOC) was used to drive the IoT devices to run the software platform |
| Skin infection, an eye disorder | It uses a built-in smartphone microphone. The standard image library with pattern matching and/or visual inspection. Smartphone on chip (SOC) was used to drive the IoT devices to run the software platform |
| Oxygen saturation monitoring | The Nonin pulse dosimeter wrist features AI-powered pulse-by-pulse filtering, designed for seamless integration in clinical environments |
4.2.1. Oxygen Saturation Observation
Pulse oximetry is used for noninvasive continuous monitoring of BP and oxygen saturation levels. Integrating IoT with pulse oximetry provides valuable insights for medical healthcare applications. Several IoT-based pulse oximetry systems have been developed.
4.2.2. BP Observation
Integrating NFC-enabled BP monitoring devices with IoT systems allows for remote monitoring and data transmission, as described in [115]. These devices combine a BP monitor with communication technology, enabling seamless data sharing through an IoT network [116].
4.2.3. Body Temperature Observation
Monitoring body temperature is crucial for maintaining homeostasis and managing healthcare [117]. Several IoT-based body temperature monitoring systems have been developed, utilising technologies like RFID for real-time data collection and transmission. RFID and body temperature monitoring units have been identified as central mechanisms responsible for temperature monitoring and connection. The RFID unit plays a key role in identification and communication, allowing the system to associate temperature readings with a specific user. The RFID tag, attached to the user or their wheelchair, enables automatic recognition each time the user interacts with the system. The temperature monitoring unit, typically a wearable or attachable sensor, continuously measures the user’s body temperature and transmits these data wirelessly to the RFID system. RFID and temperature monitoring integration ensure seamless health monitoring, triggering alerts when abnormal temperature readings are detected and providing accurate tracking linked to the specific user. These two components form a cohesive real-time health monitoring and user identification mechanism.
4.2.4. Glucose Level Sensing
The management of diabetes can be enhanced through the use of IoT-enabled glucose monitoring. This technology facilitates the tracking of blood glucose levels and assists in meal planning, activity scheduling and medication management [118]. Furthermore, there have been proposals for noninvasive IoT glucose monitoring systems to connect patients with healthcare providers through IPV6-based networks [106].
4.2.5. ECG Observation
IoT-enabled ECG monitoring facilitates the real-time tracking of the heart’s electrical activity. Multiple studies have explored the potential of IoT in ECG monitoring, offering valuable insights into heart health and the early detection of abnormalities [8].
4.2.6. Cancer Disease Application
Integrating IoT technology in cancer treatment involves the combination of WSNs and remote monitoring [106]. IoT devices are crucial in monitoring patient’s health status during cancer treatments and chemotherapy, effectively alerting healthcare providers to potential complications [119]. Cancer detection using the olfactory cortex and olfactory bulb is an emerging field of research that explores how changes in smell and related brain regions could be used for diagnosis. The olfactory system, which includes the olfactory bulb and olfactory cortex, as illustrated in Figure 16 plays a crucial role in detecting odours and processing scent information. Recent studies suggest that the olfactory system may have the ability to detect certain volatile organic compounds (VOCs) emitted by cancerous tissues. These VOCs can potentially be identified in breath or bodily fluids, providing a noninvasive way to detect cancer.
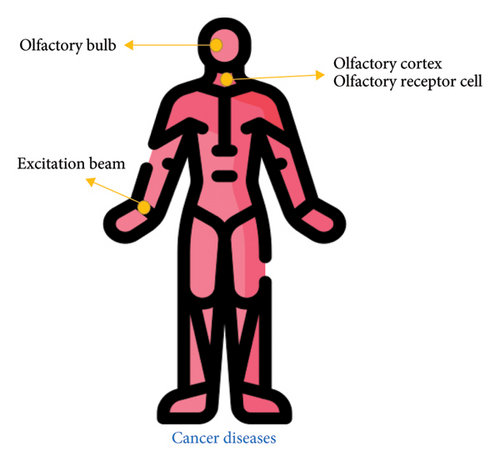
Cancer care is enhanced by the utilisation of electronic medical databases and integrated systems, such as the lab interface system (LIS), pathology interface system (PIS) and radiology interface system (RIS) [120]. These systems function as gateways for healthcare providers to access patient data, such as lab results, cancer diagnoses and radiology reports. RIS interfaces with the DICOM network to exchange diagnostic imaging results, while LIS and PIS utilise the HL7 network to exchange laboratory and pathology outcomes. In conjunction with pharmacy, medical oncology and radiology oncology systems, these integrated systems furnish healthcare professionals with comprehensive patient data accessible from any device within the hospital premises or via a wireless VPN connection from external locations [121].
Incorporating IoT technologies into healthcare services and applications offers numerous benefits, including enhanced patient monitoring, improved medical decision-making and more efficient healthcare delivery. These advancements are transforming the healthcare landscape by offering innovative solutions to the challenges faced in patient care [26].
4.3. IoT Healthcare Scenarios
In addition to IoT services, it is essential to emphasise specific IoT-enabled healthcare applications worthy of attention [122]. These applications, directly utilised by patients and healthcare providers, illustrate how IoT innovations can provide numerous healthcare solutions [123]. The following section delves into various IoT-cantered healthcare mobile applications in Table 6, encompassing those tailored to individual and group-based needs [124].
| Smartphone APPs | Description |
|---|---|
| ECG self-monitoring | Register ECG data, and it works as an automated ECG device having built-in software ECG self-check |
| Cardiac mobile ECG | ECG system having 12 channels of pc, cardiac window full scale is served as an app |
| Heart rate | Using a smartphone’s built-in camera, it measures instant heartbeat rate by sensing the changes in fingertip colour |
| Periodic tracker | Forecasts of fertility and periods are tracked |
| Period calendar | It tracks ovulation dates, cycles and best periods and helps prevent or archive pregnancy |
| Pedometer | It is used to track or record the user’s steps and monitor it to display information about the user, such as burned calories per unit of time |
| Noom Walk | It tracks and counts user steps all day and serves as a pedometer |
| Water your body | It tracks its users’ water drinking habits and reminds them of drinking water daily |
| Calorie counter | It tracks user measurement, weight, food consumed and other activities |
| Google fit | A user is tracked in activities such as walking, cycling and running |
| Healthy children | Paediatricians are searched by using locations and give quick answers by requesting advice |
| Health assistant | The health parameters, such as physical activities, lipids, BP, fat, glucose level, body temperature and weight, are tracked |
| Elektor cardioscope | Registering ECG data and serves as automated ECG by using software name as built-in self-check |
| Heart rate monitor | Heart rate is measured in real time |
| Heart rate | Heart rate is measured in real time |
| Cardio mobile | Cardiac rehabilitation is monitored remotely in real time |
| Blood pressure watch | Blood pressure data are shared, analysed, tracked and collected |
| Finger BP | BP is a measure based on a fingerprint |
| Tracker asthma | Asthma patients are tracked |
| Skin vision | The user’s skin health is tracked, and skin disorder is discovered early |
| Eyecare plus | Monitor and test the vision |
| Rehabilitation game | The patient is rehabilitated using interactive game facilities for hearing loss |
| Dose cast education remainder. | The user’s medication time is reminded, inventory is tracked, and the drug management log is maintained |
| Medisafe meds and pills remainder | It reminds the user of the time the medication is taken |
| Body temperature | Body temperature is tracked, and severity is identified |
| Fingerprint thermometer | By using fingerprints, body temperature is determined |
| Diabetes | Medication and blood glucose are tracked to manage diabetics |
| Oximeter | SpO2 and pulse rate are calculated |
| Daily yoga | Users can practice yoga, which helps their health |
| Mayo clinical meditation | It helps the user to meditate and exercise |
| Calm | It helps the user relax, meditate and sleep |
| iFall | Response and fall are detected |
| Fade | A fall is detected |
| Fall detector | An alert is issued to monitor human activities in case of falls |
| Sleep aid | Sleep apnoea is managed |
| Relax melodies | Relieves insomnia and aids sleep |
| Stop tinnitus | It helps to reduce tinnitus |
| Real noise 3 | In a noisy environment, it helps to stay focused |
| Uhear | It allows for self-aiding of hearing. |
| Test your hearing | Hearing tests in different ways |
| eCAALYX | Disparate chronic conditions are monitored |
| Pulmonary rehabilitation | It serves as self-monitoring for pulmonary rehabilitation |
| My CF (cystic fibrosis) | Cystic fibrosis is tacked for status |
4.3.1. CVD Applications
CVDs, including coronary heart disease, hypertension [125], heart arrhythmias and other heart-related ailments, are primary contributors to global mortality [126]. Acute chest pain serves as a significant indicator of heart disease, while some instances of heart failure may present without apparent symptoms. For patients managing chronic hypertension, continual monitoring of BP and body weight is imperative for long-term care [127]. The most dependable diagnostic tool for heart disease is the ECG, which measures the heart’s electrical activity using electrodes fixed to the patient’s chest [12]. ECGs yield more data than other vital signs, such as HR and BP, and are pivotal in evaluating heart function and detecting irregularities [128].
The conventional method for ECG monitoring utilises Holter devices, which capture the ECG signal over a complete day in a home setting [129]. As depicted in Figure 17, various sensors such as SPR, electromechanical and QCM sensors assist with monitoring CVDs. The collected signal is subsequently analysed for any irregularities [130]. Remote ECG monitoring is valuable for post–heart surgery rehabilitation, as it reduces hospital stays while ensuring patients remain under expert supervision [131].
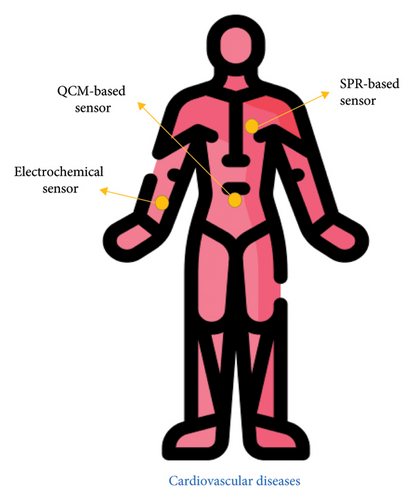
Wireless and mobile technologies have facilitated the real-time transmission of patients’ ECG and other heart measurements to healthcare providers [132]. WBAN plays a crucial role in these systems, integrating sensor data collected during scheduled patient body measurements [66]. Remote monitoring helps reduce healthcare costs by minimising hospital stays and enabling early detection and treatment of heart disease [128]. Innovative devices such as bright vests, equipped with various sensors, noninvasively collect biosignals [133]. These devices measure ECG, photoplethysmography (PPG), HR, BP, body temperature and galvanic skin response (GSR).
Additionally, smaller devices can remotely transmit heart-related parameters like ECG, PPG and impedance data [134]. A comprehensive study of over 120 ECG monitoring systems and signal processing algorithms concluded that innovative wearable ECG systems enhance the quality of healthcare services while reducing costs [135]. These systems also incorporate additional vital sign monitoring features [136].
Adopting innovative monitoring systems that measure essential parameters, including ECG, enhances healthcare services in real time while reducing healthcare costs [137]. From a wireless communication perspective, these systems face power consumption, data rates and latency challenges. However, the critical nature of heart monitoring makes overcoming these challenges essential for improving patient outcomes.
4.3.1.1. Low Information Rate
Frequent tests, including HR, BP and body weight measurements taken multiple times daily, can be efficiently performed using 8-bit data resolution. Each test, accompanied by a time stamp, generates approximately 10 bytes of data, resulting in minimal data flow over time and necessitating limited real-time processing. However, it is essential to note that these tests do not facilitate real-time drop detection or produce large data outputs [138].
4.3.1.2. Medium Information Rate
Technologies within this category include standard ECG monitoring systems, which yield 12- to 16-bit data streams at sampling rates ranging from 250 Hz to 1 kHz. Real-time transmission of ECG signals has opened up new avenues for wireless monitoring of patients with CVD and rehabilitation purposes [139]. As per expert opinion, effective remote care necessitates end-to-end ECG signal processing with a latency of less than 1 s. Commercial devices such as the breeze bio harness can continuously monitor a one-channel ECG with 12-bit resolution at a 250-Hz sampling rate. This device is equipped with an accelerometer to monitor the patient’s activity level (100 Hz) and posture (1 Hz). Typically, these devices generate approximately 3 kbps of ECG data and 1.5 kbps of activity data [140,141].
4.3.1.3. High Information Rate
Sophisticated multichannel ECG instruments employed for clinical evaluation incorporate 12-lead ECGs [142], often with five channels and 16-bit resolution at 1-kHz sampling rates [143]. To enable comprehensive monitoring of CVD patients or capturing unprocessed data on human movement, posture is essential for thorough analysis. Employing a 16-bit inertial measurement unit (IMU) at 50–250 Hz enables high-resolution motion capture, reducing motion artefacts and enhancing signal accuracy, thus contributing to more accurate diagnoses. Data processing can be performed at the device level or in the cloud, with AI techniques playing a pivotal role in both contexts [144]. Remote monitoring of multichannel ECG and EMG typically necessitates data rates of 120 and 60 kbps, respectively. Additionally, real-time transmission of unprocessed data from 1–3 motion sensors is supported, with AI-driven processing ensuring precise diagnosis [145].
4.3.2. Transmittable Infection Application
The global prevalence and severity of infectious diseases vary depending on the particular pathogen group. Despite the successful control of some deadly pathogens, sexually transmitted diseases (STDs) continue to pose a significant public health challenge, particularly in developed nations [146]. Although often nonfatal, STDs can result in severe complications, such as infertility. Timely screening, treatment or quarantine measures are essential for preventing outbreaks from escalating into epidemics [147]. Point-of-care testing (POCT) and lab-on-a-chip (LoC) devices play a pivotal role in advancing preventive healthcare by delivering clinical-grade diagnoses at accessible costs [148]. Additionally, automated remote reporting significantly enhances the management of infectious diseases, particularly for vulnerable populations like the elderly [149].
Rapid diagnostic tests (RDTs) are cost-effective, sensitive, specific, user-friendly and fast, making them essential for detecting infectious diseases [150]. Originally developed as part of standardisation efforts for large-scale medical diagnostics [151], RDTs, including serological tests, are available in European pharmacies. However, these tests rely on pre-existing immune responses and require a few days of incubation before detecting infections [152]. Although RDTs are less accurate than traditional diagnostic tests, they can be equipped with automated readout systems using ultraviolet light sources and CCD cameras, similar to the technology used in digital pregnancy tests [153]. BL-enabled microprocessors can be integrated into these systems for real-time data transmission.
Smartphones equipped with advanced cameras can read lateral flow tests and automatically upload results to a central medical database [154]. Current RDTs are available for diseases such as HIV-1 and Chlamydia trachomatis. Furthermore, serum biomarker levels, such as C-reactive protein (CRP), can be measured to monitor infection progression and response to treatment, as illustrated in Figure 18 [155].
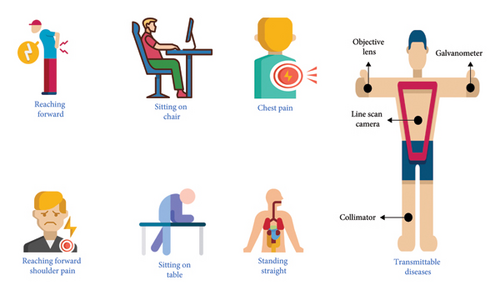
Second-generation POCTs utilise advanced molecular diagnostic techniques, particularly nucleic acid amplification tests (NAATs), currently regarded as the gold standard for pathogen detection. These techniques, such as polymerase chain reaction (PCR), are widely employed in clinical settings due to their well-established and comprehensive protocols [156]. However, for LoC applications, isothermal NAATs are more suitable as they only require a stable incubation temperature for the reaction, unlike PCR, which necessitates thermal cycling. NAAT amplifies target deoxyribonucleic acid (DNA) to detectable levels in a sample, such as blood, even in background noise. The amplified DNA (amplicons) can be detected using marker molecules or electrochemical sensors. Additionally, these amplicons can be visualised on a lateral flow assay, similar to first-generation RDTs, providing the same options for automated readouts as previously mentioned.
Electrochemical sensors are a highly effective option for integrating high levels of functionality, as both sensors and processing units can be developed in a single process and packaged together in the same module [157]. LoC tests have immense potential in distributed healthcare environments [158]. Only a few LoC tests have been performed with automated remote reporting capabilities [159]. One example is the SIA Lab, a portable, battery-powered device that uses disposable LoC cartridges to conduct enzyme-linked immunosorbent assays (ELISAs) for detecting antibodies to specific infectious diseases, as illustrated in Figure 18. The device tests for HIV-1 and transmits the results to a central database via an integrated cellular broadband connection. This system was rigorously tested for HIV-1 detection [160].
The MChip platform detects HIV-1 at one-tenth the cost of a standard bench-top ELISA test and requires minimal user training. The MChip platform is a first-generation POCT with automated remote result reporting that relies on serological testing rather than the more reliable NAAT method [161]. Currently, no second-generation POCTs feature automated reporting, although there are commercial NAAT devices, and the literature suggests efforts to implement them. The Alere Flu A&B [162] is a prominent example of a portable NAAT test with automated result readouts, though it lacks remote reporting features, as shown in Figure 19.
This device offers a robust bench-top solution for rapid diagnosis of the flu virus at a lower cost and faster than conventional methods. Ref. [163] demonstrated a LoC cartridge powered and controlled via a computer’s universal serial bus (USB) port. The cartridge showcases a self-contained HIV-1 detection platform based on NAAT testing, integrated with a pH sensor to measure the concentration of all amplicons [164].
4.3.3. Neuromuscular Disorder Application
Present telemedicine and ehealth systems, along with wearable and M-Health solutions, are mainly focused on gathering data and exchanging information between patients and physicians [165]. These systems do not impose strict real-time performance requirements and are not heavily reliant on communication channel quality [166]. Advanced remote sensing applications, such as LoC systems, also do not impose stringent demands on communication channel quality. However, closed-loop systems involving multiple actuators present more complex scenarios. For instance, assistive technology for patients with neuromuscular diseases may offer physical walking assistance and help prevent falls [167]. In 2005, approximately 40 million neurological disease cases contributed to over 90 million disability-adjusted life years (DALYs) globally. In this context, electrical muscle stimulation (EMS) offers a new therapeutic approach for stroke and Parkinson’s disease. Additionally, rhythmic auditory stimulation may help alleviate Parkinson’s off-phases. Many patients with stroke, ataxia or traumatic brain injury could benefit from EMS to improve their gait [168].
As depicted in Figure 20, neuromuscular disorders can be managed using femoral and micro-electromechanical systems (MEMS) sensors integrated into a system using USB interfaces, microprocessors and SD cards. EMS devices are available to stimulate muscles in patients with neurological disabilities [61]. For instance, using electrical signals and commercial foot drop devices stimulates heel muscles during walking, reducing the risk of falls. These electrical triggers can be manually controlled over a wireless connection or, in modern systems, activated by sensors embedded in the sole, as shown in Figure 21.
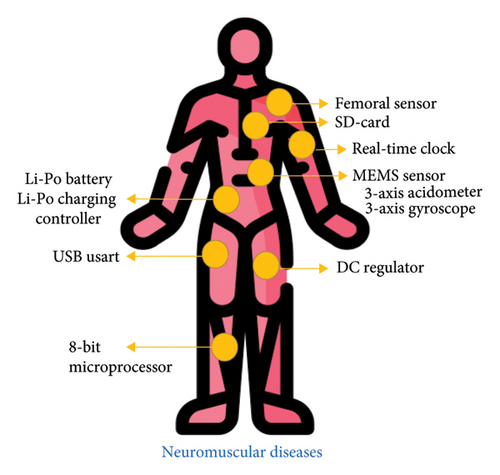
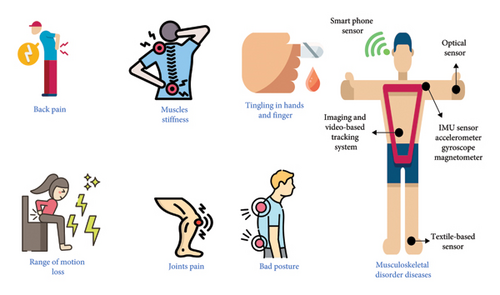
Research findings on human haptic feedback suggest that latency should not exceed approximately 50 ms for an immediate response or action to be achieved [138]. Currently, whether manual or sensor-activated, stimulators function as standalone devices and do not consider varying environmental conditions or the patient’s other health parameters. Present systems fail to consider environmental factors such as icy surfaces, stairs or increased HRs. Communication delays between the sole sensor and the actuator also pose potential risks to patient safety. Consequently, network solutions for wearable actuators must ensure consistent QoS levels, particularly in the presence of multiple external reference inputs.
The sophisticated EMS system depicted in Figure 20 integrates additional data for muscle activation. Inertial measurement units (IMUs) fixed to the patient’s body provide information about body posture to prevent falls proactively. External sensors, such as HR monitors, also gather environmental data.
The clinical requirements of such systems can be delineated using intelligent medical objects (IMO), which amalgamate accelerometers, gyroscopes and magnetometers, providing 9 degrees of freedom (DOF) [169]. The accuracy of each sensor is typically 16 bits, and with a resolution of 100 Hz, the computational load amounts to 14.4 kilobits per second. With multiple IMUs and an actuator, the system must handle approximately 10 kilobytes of data every 50 milliseconds. The selection of communication technology is pivotal for such advanced systems. The Continuous Health Alliance of medical device manufacturers has certified BL and ZigBee for wireless communications in medical applications. Nonetheless, with the escalating ubiquity of medical devices, specialised wireless standards, such as WBANs, medical body area networks (MBANs) based on IEEE 802.15.1j and SmartBANs, have been introduced for healthcare applications.
4.3.4. Musculoskeletal Disorder (MSD) Application
MSDs impact the movement of the human body or the musculoskeletal system, such as the hands, wrists, elbows, neck, shoulders and spine [170]. MSDs represent a prevalent occupational health concern within the European Union (EU), commonly referred to as work-related MSDs (WMSDs), as illustrated in Figure 21 [171]. According to European Occupational Diseases Statistics (EODS) data, MSDs are among the most prevalent occupational diseases. The latest Labour Force Survey in Great Britain stated that 41% of work-related illnesses stem from MSDs [172]. Similarly, MSDs pose a significant health issue for workers in the EU [165]. Statistical data and safety reports on work-related MSDs have been disseminated globally, including those published by the Australian and Canadian Centres for Occupational Health and Safety.
The development of MSDs can be attributed to several factors, including awkward postures, repetitive movements, forceful actions, vibrations, heat exposure, increased workload for productivity enhancement and poor communication [173]. Workplace design, task intensity (especially in transportation-related roles) and the weight of materials being handled all contribute to developing MSDs in various work environments. Numerous studies have investigated MSDs in different occupational groups, such as office workers, healthcare staff and paramedics, focusing on identifying the prevalence of discomfort and disorders affecting the neck, shoulders, wrists, hands, and upper and lower back [27]. Traditionally, MSD data collection relies on surveys and questionnaires, which may be inaccurate [174]. Wearable sensors and devices can improve accuracy and detect posture, strain on specific bones and load estimation [175]. These devices can support precise data collection and provide early warnings to workers about harmful movements or postures. At the local level, POCT and diagnostics can alert workers to potential hazards. Infrared cameras can also be used for gait analysis, providing early warnings [176].
Remote monitoring is another critical aspect of diagnosing and predicting potential MSDs. Accurate sensor data can be transmitted to the cloud for long-term analysis and projections. Advanced systems could leverage AI algorithms and big data analytics to address complex MSD prevention challenges.
4.3.5. Rehabilitation Scheme
Physical therapy and rehabilitation are essential components of the medical field, and they contribute to restoring functionality and improving life quality for individuals with physical injuries or disabilities. IoT holds significant potential to enhance rehabilitation processes by addressing challenges faced by the elderly population and the shortage of healthcare professionals. An ontology-based automation system for IoT-driven innovative rehabilitation, as presented in [27], illustrates how IoT can effectively integrate essential resources to provide real-world material interfaces. IoT-based technology offers a valuable infrastructure for supporting remote rehabilitation sessions, allowing for limited yet effective rehabilitation [176]. Various IoT-cantered rehabilitation systems have emerged, including integrated applications for prisons [177], rehabilitation training for hemiplegic patients [41], smart city rehabilitation systems [178] and a linguistic training system for children with autism.
4.3.6. Imminent Healthcare Answers (IHS)
The complete integration of several mobile medical devices into the IoT network has yet to be fully demonstrated. However, these devices are anticipated to become an integral part of IoT operations soon. The growing demand for IoT-based services globally has been accompanied by increasing medical healthcare applications, devices and cases. Healthcare services expected to merge with the IoT shortly include haemoglobin monitoring, peak expiratory flow rate measurement, cancer treatment, eye disease, skin conditions and remote surgery [179]. The majority of presently available devices are mobile diagnostic tools with traditional connectivity.
4.3.7. Healthcare Solutions Using Smartphones
In recent years, there has been a notable increase in the prevalence of electronic devices equipped with smartphone-controlled sensors, emphasising smartphones as pivotal enablers of IoT as shown in Figure 22. As Table 6 discusses, this trend has spurred the development of numerous hardware and software products intended to transform smartphones into versatile healthcare applications. A comprehensive examination of smartphone healthcare applications is expounded upon in [180], detailing applications catering to patients, general healthcare, medical education, training, information retrieval and other related functions, collectively called secondary applications. A range of solutions have been devised for healthcare professionals, including drug reference apps, medical literature search tools and applications for medical education, among others. Smartphones are now equipped to carry out diverse healthcare diagnostics and monitoring tasks, such as asthma detection, chronic obstructive pulmonary disease (COPD) management, cystic fibrosis monitoring, HR and BP tracking, and diabetic wound assessments [176]. While smartphones offer substantial benefits due to their widespread availability and cost-effectiveness, ongoing challenges such as computational complexity, power consumption and environmental noise require attention. Notably, various health and fitness accessories tailored for smartphones, such as the Fitbit Flex, are furnished with resources to aid individuals in attaining optimal health.
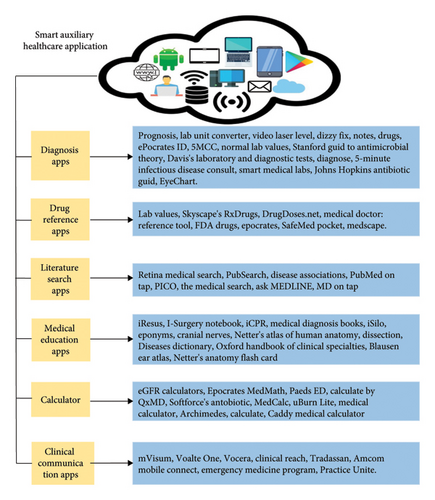
The limitations of using smartphones as edge devices in monitoring diseases and disorders and their effectiveness for specific conditions are discussed. While smartphones offer significant potential for disease monitoring, they have limitations regarding processing power, battery life, sensor accuracy and data privacy concerns. Smartphones may struggle with computationally intensive tasks, such as complex data analysis for certain diseases. They may not offer the precision required for medical-grade measurements, such as blood glucose or oxygen saturation levels [181]. Additionally, privacy risks related to health data remain a concern [182].
However, smartphones have proven particularly effective for managing chronic conditions like hypertension, diabetes and asthma, where they can track vital signs, provide medication reminders and support disease management [183]. They are also valuable for mental health applications, such as monitoring mood and supporting behavioural interventions [184]. Smartphones paired with wearables for MSDs and rehabilitation effectively track movement and progress [185]. On the other hand, smartphones are less effective in monitoring conditions that require specialised equipment, such as neurological disorders (e.g., epilepsy or Parkinson’s disease) or infectious diseases requiring diagnostic tests like PCR [183]. Overall, smartphones are valuable for certain types of disease monitoring but are not a one-size-fits-all solution, especially when high precision or specialised diagnostics are needed [184].
4.3.8. Wheelchair Administration
Researchers have developed smart wheelchairs with full automation designed for individuals with disabilities, and IoT holds the potential to expedite this advancement. An IoT-based healthcare system for wheelchair users has been detailed in [186], integrating WBANs with multiple sensors tailored to IoT requirements. Furthermore, a peer-to-peer (P2P) healthcare system combined with IoT technology has been implemented in [187] offering functionalities such as chair vibration control and the monitoring of the wheelchair user’s position. One notable illustration is Intel’s IoT-driven connected wheelchair [133], highlighting the transformation of traditional devices into data-driven machines. This device monitors the user’s sitting posture and collects environmental data, enabling the evaluation of a location’s accessibility.
The incorporation of WBANs and sensing devices into wheelchair systems. WBANs, which consist of a network of small, wearable or implantable sensors, play a critical role in enhancing the functionality and user experience of modern wheelchair systems, particularly in the context of mobility assistance, health monitoring and user safety. In a typical wheelchair system, WBANs are integrated with various sensing devices that monitor the user’s physical health and the wheelchair’s performance. These sensors can track a range of vital signs such as HR, body temperature and respiratory rate, providing real-time data that can help caregivers or healthcare professionals monitor the health status of the wheelchair user. Additionally, sensors within the wheelchair can detect parameters like seat pressure, posture or movement, which can help prevent issues such as pressure ulcers or improper seating posture. Similarly, sensors integrated into the wheels and motor of the wheelchair can monitor its speed, battery life and maintenance status, ensuring that the wheelchair is functioning correctly. Data from these sensors can be wirelessly transmitted through the WBAN to a central hub, such as a smartphone, tablet or cloud-based system, where it can be analysed and acted upon. The wireless communication ensures that the user is not tethered to the device, providing mobility and independence while maintaining continuous monitoring of health and wheelchair performance. In some advanced systems, the integration of WBANs also enables automatic adjustments to the wheelchair’s settings based on real-time data, such as adjusting the seating angle or motor assistance in response to the user’s posture or physical condition. WBANs can be synchronised with remote monitoring platforms, enabling healthcare providers or family members to receive data updates and intervene in case of any health-related concerns.
4.3.9. Medicine Administration
Failure to adhere to medication protocols poses a significant public health risk and results in substantial financial losses on a global scale. IoT presents promising solutions to this challenge. A rapid packaging technique for medication cases, utilising IoT-driven medicine administration, was proposed in [188]. This system involves a sample scheme comprising 12 packs and an intelligent medicine box (iMedbox), which underwent validation through field trials. The packaging technique features a tamper-evident seal based on delamination material managed through wireless communication. An eHealth system architecture centred on RFID identifiers for medication management through the IoT network was also discussed in [189]. The prototype demonstrates how a pervasive medication regulation system can be customised for AAL solutions.
5. IoT Healthcare Industry Trends
As detailed in Table 7, IoT is introducing new technologies and trends expected to significantly impact the healthcare sector. This advancement holds the potential to shape the future of healthcare through innovative applications, the emergence of entrepreneurs, the involvement of venture capital firms and the development of creative solutions. Established companies and emerging start-ups actively explore this space, striving to establish a presence in a potentially massive market by introducing enabling technologies and products.
| Firms | Status/vision |
|---|---|
| Intel | Interaction between patients and doctors is improved, and information security is strengthened by using Intel power devices. A communication system is synchronised in real time, health data are streamed, cycle time is reduced, and the quality of medical workflow is improved in different environments. Healthcare results should be provided anywhere, anytime using IoT, which is the central Intel vision |
| Qualcomm | The 2net platform of Qualcomm Life offers Wireless Health Solution which can deliver and capture data from wireless health devices by combining databases and portals for the user. Security and interoperability are integrated into a system to store data. Qualcomm aims to expand innovative, intuitive and intelligent solutions for healthcare |
| Samsung | San Francisco, the University of California and Samsung Electronics established a digital health lab and developed smart health technology. Samsung and the International Medical Education Conference (IMEC) enlarged a platform named Simband, an open-reference design for sensors and device modules. Samsung aims to develop a seamless and ubiquitous user experience for health solutions with no complexity |
| For IoT, Google opens an open-source physical web-standard code and uses it to communicate with medical devices more effortlessly and in a more arranged manner | |
| Microsoft | Microsoft provides an IOT-based healthcare solution by focusing on the intelligent system. In Healthcare technology, an innovative system is a backbone that collects the data from health devices and sensors for connectivity inquiry. From collected data and extracted essential data using a business intelligence tool |
| CISCO | Commercial and Industrial Security Corporation (CISCO) introduces an effective algorithm and provides a network coverage system for handling load balances with advanced data analytics for IoT health devices. It is using an intelligent application for security and efficiency. Healthcare organisations are working with CISCO to develop a medical network architecture |
| GSMA | It is associated with related firms and mobile operators that have developed living programs to deliver health solutions in the healthcare and mobile industry over secure and intelligent IoT networks |
| Deutsche Telekom | Deutsche Telekom follows a secure healthcare internet system. The research team develops technologies for helping healthcare services that can be digital, local, personal, etc. It is like a bridge between associate stakeholders |
| Wind river system | Wind river system introduces a business logic model and a cloud for IOT healthcare solutions. These designs consist of a data aggregation/supervisory system, data entry and gateway with a device or sensor control system for IoT healthcare purposes. This will improve medical services, such as aid for providers and patients, in the future |
| Apple | IoT is the ultimate technology Apple has claimed. That is why Apple developed an IoT-based healthcare watch, a smartwatch that tracks user fitness and monitors the heart. Memorial Hermann’s medical solution focuses on better care, secure access and physical gains |
| IBM | Through smarter healthcare, International Business Machines (IBM) grows based on healthcare and redefines its success and value in this field. IBM and other firms get together in partnership to develop IoT devices |
| Eurotech | Eurotech develops a building block for enlarged systems that connect healthcare and medical products |
| Aeris | Aeris provides an IOT healthcare solution for providers, remote patients and medical device manufacturers |
| Machina research | Machina research develops an IOT healthcare solution. These research workers covered telemedicine, connected medical environments, AAL and remote clinical monitoring |
| Numerex | Numerex provides the top IOT solution and designing a new health system requires and offers stakeholders support |
| ThingWorx | ThingWorx has developed a healthcare system solution that many organisations use. It is used to connect healthcare and work in a firm efficiently |
For example, Edisse has created a prototype of a wearable sensor that offers real-time fall detection, tracking and alerts [190] By integrating mobile data, SMS, accelerometers and GPS, the device can detect unusual movements, such as falls and promptly alert caregivers or family members. Withing has introduced various healthcare devices and applications, including internet-enabled scales and baby monitors [191]. A Chinese company has developed a management information (MI) platform that integrates medical imaging, cloud-based storage, 3D imaging virtualisation and telemedicine, offering comprehensive healthcare IT solutions [192] as shown in Table 7. Neusoft has also directed its attention towards IoT-based healthcare services, like public health management and hospital facilities [193].
LiftMaster has developed products designed to facilitate easier access to homes, enabling users to control home entry via smartphones. This technology holds significant potential in applications catering to elderly individuals [194]. Garmin’s Vivosmart is a fitness smartwatch that can generate smart alarms, aiding users in making informed decisions about their daily activities [195] Additionally, Jawbone UP3 offers features for tracking physical wellness, heart health and sleep patterns. Angel is another wearable device that monitors pulse, blood oxygen levels and temperature, transmitting vital information to the user’s smartphone [196].
In South Korea, researchers have developed a wearable BP sensor that is compact and capable of continuous monitoring without disrupting the user’s daily activities [197] as shown in Figure 23. iHealth Lab has produced a range of IoT healthcare devices, including wireless BP monitors, pulse oximeters and glucose monitoring systems. Basis introduced a health tracker that monitors sleep, stress and fitness, while Phyode created a wristband that tracks HR variability and provides insights into users’ mental and physical states [198].
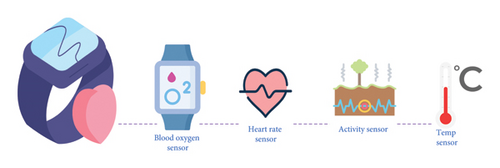
The advancements in wearable technology are noteworthy. Rejuven’s Rejiva, for instance, monitors users’ ECG, HR variability, respiratory rate and sleep position, enabling the analysis of the autonomic nervous system’s state [199]. Fuelband tracks full-body movement and physical activity, while Sync is a family tracker that monitors steps, calories and sleep, synchronising information across family members [200]. IBitz has introduced innovations for fitness tracking [200], and Remo regulates a user’s environment using gestures [194]. In addition, wearable devices like the Halo Band, Runtastic Orbit, Samsung Fit Gear and Melon offer health-tracking capabilities [198]. Reebok, RunScribe and MI Coach Smart Ball have introduced wearables for athletes, aiding them in improving performance while ensuring safety [196]. OM Signal is working on biosensing apparel, aiming to transform users’ approach to physical well-being [199].
Vessyl is a bright cup that tracks real-time beverage consumption [201], while Owlet has developed a baby health tracker that monitors HR, temperature and oxygen levels [202]. Sproutling has introduced a baby monitor for similar purposes [203]. HR monitors are from AliveCor and Pulseo, Skulpt’s body composition measurement tool, and NutriCrystal’s smart food scale to track nutritional intake [204]. Proteus Digital Health has also developed a pill sensor powered by stomach fluids to track drug intake [204], and GlowCaps by Vitality Inc. aids users in maintaining their medication schedule with prescription bottle sensors [205]. Mimo’s infant monitor tracks breathing, body temperature and sleep via a smartphone app [206]. Preventice’s Body Guardian remotely monitors cardiac arrhythmias and biometric data, sending results to healthcare providers [207]. The range of IoT-based healthcare products and prototypes, as depicted in Figure 24, illustrates the diversity of technologies enhancing patient care. Each of these devices represents the trend of integrating IoT into healthcare, providing insight into the future of medical technology.

6. IoT Healthcare Security Issues
The rapid expansion of IoT is expected to profoundly impact the healthcare industry, leading to the widespread adoption of applications and devices that enhance eHealth. These technologies facilitate the management of critical healthcare data, including personal information, which can be accessed globally anytime. However, this heightened connectivity also exposes IoT systems to potential cyber threats. To effectively integrate IoT in healthcare, it is essential to address security and privacy vulnerabilities, understand threat models, implement countermeasures and meet specific security requirements, as illustrated in Figure 25.
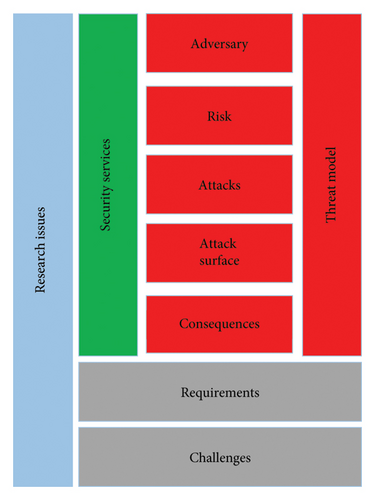
6.1. Requirements of Security
To ensure secure services, the security requirements for IoT-based healthcare solutions must align with standardised communication protocols. Key security requirements include the following.
6.1.1. Confidentiality
It ensures unauthorised users cannot access medical information. Private messages must resist exposure from attackers (eavesdroppers) [176].
6.1.2. Integrity
It guarantees that no alterations are made to medical data during transmission or storage [208].
6.1.3. Authentication
It confirms the identities of IoT devices communicating within the healthcare system [176].
6.1.4. Availability
It ensures IoT healthcare services remain accessible to authorised parties, even during denial-of-service (DoS) attacks [209].
6.1.5. Freshness of Data
It ensures all transmitted messages are recent and unique, preventing replay attacks.
6.1.6. Nonrepudiation
It prevents entities from denying the transmission of a message they sent [210].
6.1.7. Official Permission
It ensures only authorised nodes can access network resources and services.
6.1.8. Resiliency
It protects information even if some healthcare devices are compromised [136].
6.1.9. Fault Tolerance
It ensures the continuity of security services, even in the event of faults.
6.1.10. Self-Healing
It enables the remaining devices to maintain security when some fail or run out of energy [187].
6.2. Challenges of Security
Traditional security techniques often fail to meet the specific security needs of IoT-based systems, particularly in healthcare. Novel countermeasures are required to address the unique challenges posed by IoT. Some of the key challenges in securing IoT healthcare services include the following.
6.2.1. Computational Limitations
Healthcare IoT devices often have low-speed processors, lacking the capacity to handle resource-intensive computations. These devices act primarily as sensors or actuators, making it challenging to implement security solutions that require minimal resource consumption while maximising security performance [211].
6.2.2. Limitations of Memory
Many IoT-based healthcare devices have limited storage capacity and are powered by embedded operating systems and software. This restricted memory may not support complex security protocols, posing a challenge in ensuring robust security for these devices [167].
6.2.3. Limitations of Energy
Healthcare IoT devices like BP and body temperature sensors often operate on limited battery power [][212]. These devices conserve energy by entering power-saving modes when not in use and reducing CPU speed when handling noncritical tasks [213]. Developing energy-efficient security solutions for such devices remains a challenge [203].
6.2.4. Mobility
Healthcare devices typically operate in a mobile capacity, connecting to the internet via IoT service providers [214]. Wearable devices like heart rate monitors and temperature sensors are designed to link with various networks based on the user’s location, such as home or office networks, each with distinct security settings. Developing a security algorithm compliant with mobility and adaptable to various network configurations is a significant challenge [215].
6.2.5. Scalability
With the global increase in IoT devices, the design of a scalable and highly secure framework that can accommodate more devices without sacrificing security has become increasingly complex [216].
6.2.6. Media Communications
Healthcare devices connect to global and local networks via various wireless communication methods, including Zigbee, BL, GSM, Wi-Fi and 3G/4G [205]. The characteristics of these wireless channels differ from traditional wired networks, making it challenging to develop a comprehensive security protocol that addresses both wireless and wired communications [217].
6.2.7. Abundance of Devices
Healthcare IoT devices incorporate a wide variety, ranging from sophisticated systems such as personal computers to more straightforward RFID tags. These devices exhibit memory, power, software and computational capabilities variations. Developing a security framework that can effectively address the diversity of these devices presents a significant challenge.
6.2.8. A Topology of Dynamic Network
Healthcare devices can join or leave IoT networks anytime, sometimes without notification. Managing devices’ dynamic admission and exit within the network is complex and presents significant challenges for network security [218,219].
6.2.9. A Network of Multiprotocol
Healthcare devices may interact with other local devices using occupancy network protocols while communicating with IoT service providers over internet protocols [205]. Ensuring secure communication across multiple protocols is a challenging task for security experts.
6.2.10. Dynamic Updates of Security
To minimise potential security vulnerabilities, IoT healthcare devices need frequent updates to their security protocols. Developing a framework for dynamically installing security patches while maintaining system integrity is a complex challenge [220].
6.2.11. Packages of Tamper-Resistant
Physical security is vital for IoT healthcare devices, as attackers may attempt to extract cryptographic keys or alter device programs. Implementing tamper-resistant packaging to protect against such attacks is difficult but essential [221].
6.3. Threat Model
The growing complexity and breadth of IoT healthcare applications and networks make them particularly vulnerable to security breaches. As services expand across local, cloud and cloud-based platforms, the connectivity between IoT devices, networks and applications intensifies. This increased connectivity raises the risk of attacks that can exploit hardware and software limitations. Threats to a network can arise from both internal and external sources. Unauthorised access, especially from a nearby healthcare network, has the potential to cause significant damage. However, it can be difficult to identify compromised or weak points within interconnected systems. Adversaries may target static and active medical devices, gaining access through IoT devices or control tools such as tablets and laptops [222].
6.4. Attack Taxonomy
The IoT paradigm is continually evolving, and many more IoT-based healthcare devices and services are expected to integrate into this ecosystem. However, intruders will continue identifying and exploiting current and future medical devices and network vulnerabilities. Some risks are quantifiable and others can be anticipated, while some are difficult to predict [223].
6.4.1. Disruption-Based Attack on Information
- •
Interruption: DoS attacks are initiated, leading to communication breakdowns, network outages or system failures, which impact the reliability of hospitals’ network capabilities.
- •
Interception: An attacker intercepts medical data, violating privacy and confidentiality in communication channels.
- •
Modification: Unauthorised access allows the attacker to alter health records, misleading individuals and compromising the integrity of the healthcare system.
- •
Fabrication: Fake data are inserted by attackers to corrupt the integrity of the communication network.
- •
Replay: Previous communications are replayed to disrupt freshness in data exchange, causing confusion and misleading users.
6.4.2. Host Property Attacks
- •
User Compromise: Hackers steal user credentials or encryption keys by breaking into the system and exposing sensitive data [224].
- •
Hardware Compromise: Attackers tamper with devices to retrieve passwords, keys or data, potentially reprogramming devices with malicious code [225].
- •
Software Compromise: Vulnerabilities within software or applications are exploited, causing service degradation or system failure (e.g., memory overflow or resource exhaustion) [226].
6.4.3. Networking-Based Attacks
- •
Dynamic Protocol Negotiation: By deviating from standard protocols, attackers aim to compromise hardware quality, communication security and confidentiality [227].
- •
Network Protocol Stack Attacks: As shown in Figure 26, each layer of the IoT protocol stack has vulnerabilities which attackers can exploit. Ensuring security at every protocol layer is essential for enhancing IoT healthcare networks’ resilience, safety and accessibility [228].
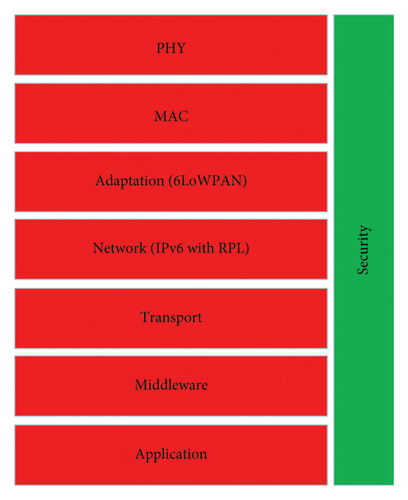
6.5. Model Proposed
Although the IoT healthcare model is still developing, identifying and predicting bugs, risks and attacks remains a challenge [229]. Security experts must take a proactive approach to address visible and recurring issues through the implementation of solutions. These experts need to integrate advanced features aimed at mitigating emerging threats, thereby ensuring robust protection within IoT healthcare environments. This strategic approach facilitates the identification and resolution of previously overlooked experiential and knowledge-based challenges. For instance, consider a scenario in which a security system is designed specifically to detect and prevent two distinct types of data integrity attacks. However, if an unauthorised individual were to initiate a different form of attack, it could undermine the security of medical data, consequently jeopardising the integrity of wider healthcare tools, networks and applications.
To effectively address emerging security threats, it is imperative to enhance existing security services with advanced intelligence-based algorithms capable of detecting new types of attacks. The model illustrated in Figure 27 incorporates three protective layers within a unified network to counter potential threats effectively.
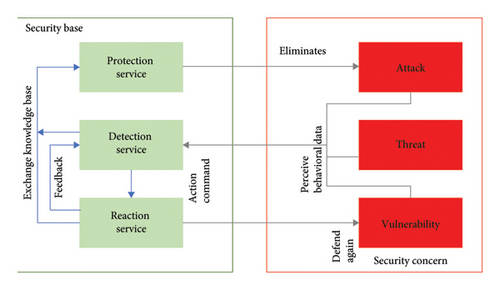
The primary objective of the model is to minimise security breaches. Monitoring systems collate activity data, analyse symptoms and track health information from IoT healthcare devices, hospitals and networks. Health authorities support response mechanisms and deploy defence protocols to counter these attacks. These protective services are underpinned by sophisticated algorithms that work in unison to protect against current, future and hidden threats.
Detection services are critical in identifying intrusions and sharing information with defence mechanisms to prevent further attacks. Response services activate error mitigation strategies when risks are identified and coordinate with monitoring and defence systems to take corrective action. This collaborative approach ensures a comprehensive defence against IoT healthcare threats, maintaining systems’ resilience and security.
7. IoT Healthcare Countries Policy
The integration of IoT into healthcare systems has been approached in various ways across different countries, with each employing distinct policies and strategies to drive its adoption, as illustrated in Table 8. These initiatives highlight the critical role of government regulations and strategic planning in improving health services worldwide. This section describes how specific countries and organisations develop and implement IoT and eHealth strategies.
| Country/region | eHealth strategy (year published) |
|---|---|
| Australia | National eHealth strategy |
| Scotland | National eHealth strategy (2011) |
| Denmark | National IT strategy 2003–2007 for the Danish health service (2003) |
| Switzerland | Swiss eHealth strategy (2007) |
| Finland | eHealth roadmap—Finland (2007) |
| The European Commission | Repository of eHealth strategies and priorities for EU member states (N/A) |
| Mauritius | National eHealth strategy: He@lth2015, seamless continuity of care (2010) |
| Saudi Arabia | National eHealth strategy (2011) |
| Kenya | National eHealth strategy (2011) |
| The European Commission, DG for Information Society and Media, ICT for Health | European countries on their journey towards national eHealth infrastructures, evidence on progress and recommendations for cooperation action (2011) |
| The U.S. | Federal health IT strategic plan (2011) |
| Australia | State eHealth strategy |
| The European Commission, Society and Media, ICT for health | eHealth priorities and strategies in European countries (2007) |
| Sweden | National strategy for eHealth (2006) |
7.1. India
India has been implementing eHealth strategies since the year 2000, with a focus on integrating information and communication technology (ICT) into the healthcare sector. In 2005, a dedicated task force on telemedicine was established to bolster these initiatives. The ‘Digital India’ initiative aims to foster the digitisation of the economy and enhance knowledge-based healthcare systems. As part of this initiative, the government allocated 70.6 billion INR for the development of 100 smart cities, to nurture a $15 billion IoT industry by 2020. This initiative seeks to increase the number of connected devices from 200 million to over 2.7 billion. However, the expansion of IoT within India’s healthcare sector presents several significant challenges [230].
7.2. Australia
In 2008, the Australian government established a national strategy for eHealth that emphasises collaboration among federal, state and territory governments, healthcare professionals and experts in medical information. This strategic framework is designed to foster cooperation and support the integration of IoT within the healthcare system. Australia has also undertaken significant initiatives aimed at enhancing the capabilities of IoT through targeted government efforts [231].
7.3. Japan
In 2004, Japan’s Ministry of Internal Affairs and Communications initiated the ‘u-Japan programme’ to enhance internet accessibility and promote the adoption of healthcare information technologies. This programme aimed to integrate IoT solutions within the healthcare sector, to improve medical outcomes and reduce costs through the extensive implementation of eHealth technologies [232].
7.4. France
In 2004, France established a comprehensive telemedicine framework at the local level, successfully integrating eHealth solutions into its healthcare system [233]. In 2008, the government further advanced IoT by implementing Object Naming Services (ONS) core servers. This initiative facilitated access to product data through a national system of sensors and gateways, thereby promoting accuracy and consistency in data management [234]. Telemedicine services are now widely utilised across the country, and continuous efforts are being made to enhance hospital IT infrastructure [235].
7.5. Sweden
Through GS1 and SE in 2010, Sweden developed an ONS core controller to facilitate IoT networking. The country’s ‘General Policy for Electronic Health’ outlines comprehensive strategies for promoting eHealth across various regions. This policy supports IoT development in healthcare by enhancing internet connectivity for health-related products [236].
7.6. Germany
Germany began its eHealth initiatives in 2003, implementing regulatory policies aimed at enhancing the healthcare sector and establishing a leadership position in the development of IoT. The Industry 4.0 strategy, introduced as part of the High-Tech Policy in 2020, further supports the nation’s digital transformation by integrating IoT technologies into healthcare infrastructure, thereby enhancing the quality of medical services. These initiatives exemplify how governments can utilise regulatory frameworks and strategic initiatives to promote the adoption of IoT in healthcare, highlighting the potential for improved health outcomes through digital innovation [237].
7.7. Canada
Healthcare in Canada is provided by publicly funded provincial and territorial Medicare systems, guided by the Canada Health Act of 1984. Medicare ensures universal primary healthcare to all citizens, regardless of location. However, 30% of Canadians opt for private medical treatment outside the public system [238].
7.8. Korea
South Korea has made significant investments in the development of IoT to expand the market from KRW 2.3 trillion in 2013 to KRW 30 trillion ($28.9 billion) by 2020. In May 2014, the government unveiled a national strategy to establish an IoT ecosystem which includes infrastructure, frameworks, devices and IT security. South Korea also actively supports eHealth initiatives such as e-medical records, e-prescriptions and telemedicine [239].
7.9. China
In 2010, China’s Ministry of Industry and Information Technology (MIIT) laid out a comprehensive plan for IoT development. The strategy includes timelines, goals and research and development efforts to drive IoT progress. China’s eHealth Improvement Policy (2003–2010) has led to significant investments in IoT and healthcare infrastructure [240].
7.10. Pakistan
Pakistan’s healthcare policy evolved from the Lunacy Act of 1912 to the Mental Health Ordinance in 2001. The country has a complex healthcare system with federal and provincial subsystems. While provinces like Punjab and Sindh have better healthcare infrastructure, mental health and emergency policies were last revised in 2003 and 2006, respectively [241].
7.11. EU
The EU has made significant strides in promoting IoT and eHealth. In June 2010, the European Parliament backed IoT development, emphasising medical, privacy and data security measures. The Electronic Health Act Strategy, approved in 2004, marked the first formal commitment by EU member states to collaborate on eHealth initiatives [235].
7.12. Russia
Russia offers free healthcare through a state health programme, but the public system suffers from insufficient government funding, outdated equipment and poorly paid staff. Many Russians, therefore, seek private medical treatment [242]. Despite these challenges, the Russian constitution guarantees free healthcare to all citizens [243].
7.13. World Medical Association
Since 2011, the World Health Organisation (WHO) has promoted the use of eHealth to control smoking and improve health outcomes in developing countries. Many eHealth initiatives in these regions have used SMS for communication and awareness campaigns, mainly focusing on HIV, maternal and child health, and malaria [207].
This global push towards IoT and eHealth reflects the growing recognition of how technology can revolutionise healthcare delivery, improve patient outcomes and create more efficient healthcare systems.
8. IoT Healthcare Challenges and Issues
The integration of IoT in the healthcare sector presents several challenges that must be carefully addressed to ensure successful implementation and operation. This section summarises the key challenges identified by researchers, which include regulation, platform requirements, cost analysis, application development, technology integration, low-power protocols, network types, scalability, continuous monitoring, emerging diseases, identification, business models, QoS, data security, flexibility, control analysis and environmental impact [244].
8.1. Regularisation
In the healthcare industry, various vendors develop various products, and new entrants consistently join, intensifying industrial competition. However, adherence to standardised guidelines and procedures is frequently lacking, resulting in interoperability challenges in managing diverse devices. This necessitates prompt attention [245]. IoT-based healthcare technologies are subject to regulation by specialised groups, which should address aspects such as transport layers, encompassing physical (PHY) and media access control layers, device interfaces, data integration interfaces and gateway interfaces. Furthermore, administering value-added services, such as automated health records, necessitates robust access controls and registration for healthcare professionals. Regulatory bodies such as the Internet Engineering Task Force (IETF) and the ETSI can exert significant influence in formulating standards for IoT-centric healthcare [113].
8.2. IoT Medical Care Platforms
Customised computing frameworks with runtime libraries are essential for developing IoT healthcare devices, which are more sophisticated than standard IoT hardware. These devices require real-time operating systems with specific additional requirements. Implementing a service-oriented architecture (SOA) can facilitate the development of platforms that segment services through application programming interfaces (APIs). By establishing a standardised framework, efficient platforms can be constructed to support healthcare software developers in leveraging specific forms, modules, messaging patterns and other valuable data. Integrating disorder-specific libraries can significantly improve usability [207].
8.3. Cost Analytics
While IoT healthcare solutions are often perceived as cost-effective, there is a lack of comprehensive studies providing accurate data on this. A cost analysis of a typical IoT healthcare network would be beneficial for better understanding [246].
8.4. Application Development Procedure
Developing healthcare applications typically follows four stages: design, development, testing and debugging, and deployment [247]. Certified health organisations must participate in ensuring the quality of healthcare applications. Moreover, regular updates to healthcare applications are necessary to incorporate the latest advancements in health sciences [248].
8.5. Technology Change
Integrating IoT solutions into existing healthcare systems poses a significant challenge, as healthcare organisations must update their products with the novel technology. A key issue is the smooth transition from legacy systems to IoT-based configurations, requiring adaptability and compatibility with current devices [199].
8.6. Low-Power Protocols
IoT healthcare devices operate in various modes—sleep, deep sleep, collection, transmission and others—creating challenges in power management, especially in the communication layer. It is difficult to identify a device recognition method that meets low-power requirements while maintaining service availability at the MAC level [249].
8.7. Network Type
IoT healthcare networks can be categorised into three types based on policy: data-based, service-based and patient-based models. Within a data-based model, healthcare is structured around medical records. Healthcare is organised around the features or services provided in a service-based model. In a patient-based model, healthcare is focused on the patient and their interactions with family members and healthcare providers. Selecting the appropriate network type for IoT healthcare solutions presents a significant challenge [177].
8.8. Scalability
The networks, apps, facilities and back-end databases of IoT healthcare are becoming more complex as demand grows from both patients and healthcare systems. This increase in complexity poses several challenges that need to be addressed for efficient implementation and operation [207].
8.9. Constant Monitoring
Long-term patient monitoring is necessary in many cases, such as chronic diseases. Continuous observation and data recording are essential in such situations to ensure the effectiveness of care [250].
8.10. New Diseases and Disorders
While smartphones are widely used as an interface for IoT healthcare devices, the development of applications is currently limited to certain diseases. Expanding research and development efforts to cover a broader range of infrequent and emerging disease conditions is critical. Portable devices play a vital role in the early detection of these disorders [251].
8.11. Identification
In healthcare environments, multiple caregivers may interact with the same patient across different settings. Accurate identification of patients and healthcare professionals is essential to ensure proper care and data management [247].
8.12. Business Model
The implementation of IoT in the healthcare sector necessitates the development of new business models capable of accommodating evolving requirements. This entails the revision of operational protocols, organisational frameworks and the identification of prospective clientele. The hesitance of many healthcare professionals, such as nurses and physicians, to embrace novel technologies underscores the importance of establishing business models that facilitate seamless transitions to IoT-based systems [252].
8.13. QoS
Healthcare services are critically time-sensitive and necessitate assurances of reliability, sustainability and service quality. Ensuring QoS within an IoT network is paramount, as system failures can have life-threatening consequences. Addressing the challenge of implementing alternative solutions during system failures is of utmost importance [253].
8.14. Data Security
Securing healthcare data collected from various devices and sensors is a significant concern. Strict protocols must be established to ensure that information is shared only with authorised users, applications and institutions. Key security issues include the following [229].
8.14.1. Resource-Efficient Safety
Due to resource limitations in IoT devices, security solutions must balance strong protection with minimal resource consumption.
8.14.2. Physical Security
IoT healthcare devices are vulnerable to physical tampering, which allows attackers to access cryptographic data or manipulate them [248]. Therefore, devices must be built with tamper-resistant protection.
8.14.3. Secure Routing
RPLs in IoT healthcare networks are often vulnerable to attacks. Secure routing techniques are necessary to ensure safe communication [207].
8.14.4. Data Transparency
IoT devices handle sensitive medical information, which could be misused in cloud services. Techniques ensuring transparency and control over data usage are essential [228].
8.14.5. The Safety of Managing IoT Big Data
IoT healthcare devices generate large volumes of data that must be securely stored and managed without compromising confidentiality, integrity or privacy [207].
8.15. Flexibility
IoT healthcare networks must offer flexibility, enabling patients to connect to the system anytime and anywhere. This flexibility ensures seamless healthcare services across different environments [251].
8.16. Control Analytics
Control analytics play a key role in improving the performance of IoT healthcare applications. Medical data analytics can help developers enhance system design and optimise data flow [254].
8.17. Environmental Impact
The extensive utilisation of IoT healthcare devices, frequently incorporating hazardous materials, has resulted in adverse environmental and social health impacts. To address these effects, it is imperative to adopt sustainable approaches in hardware development, usage and disposal [255].
9. Critical Analysis of Current IoT in Healthcare
IoT has made significant strides in healthcare, greatly enhancing patient care. Nonetheless, there are critical challenges that must be addressed, particularly in areas such as data integration, security, scalability and long-term data management. To fully harness the potential of IoT technologies, the healthcare industry should consider implementing innovative solutions including edge computing, 5G technology, AI integration and blockchain. Ongoing research is essential to develop robust and scalable solutions that prioritise the privacy, security and efficiency of IoT-based healthcare systems [256].
9.1. Gaps in Current Research
9.1.1. Data Integration and Interoperability
Despite advancements, many IoT healthcare systems struggle with integrating data from diverse sources due to a lack of standardisation. This limits the potential for comprehensive patient care [245]. Systems often cannot easily share data between healthcare providers and devices, leading to fragmented care [257].
9.1.2. Security and Privacy Concerns
Ensuring the security and privacy of sensitive patient data remains a significant challenge. Existing systems are vulnerable to cyberattacks, which can compromise patient safety and confidentiality. Robust encryption and authentication protocols that can be efficiently implemented in resource-constrained IoT devices are needed [258].
9.1.3. Scalability and Network Management
The scalability of numerous IoT solutions presents a challenge, particularly in large healthcare networks. Managing a considerable volume of devices also creates logistical complexities. For instance, the introduction of a comprehensive IoT network in a hospital setting may result in issues related to data overload and network congestion [259].
9.1.4. Long-Term Data Storage and Analysis
Effective long-term storage and real-time analysis of the large volumes of data generated by IoT devices are still developing areas [154]. Current storage solutions may not efficiently handle the continuous data streams from wearable devices over extended periods [260].
9.2. Innovations in IoT Healthcare
9.2.1. Edge Computing
Data should be processed at the network’s edge, closer to its source, instead of relying solely on centralised cloud servers, as discussed in [261]. This will reduce latency, improves response times and enhances the real-time processing capabilities critical for applications like remote patient monitoring [262].
9.2.2. 6G Technology
Deploying 6G networks offers faster data transmission rates and lower latency [11].
This will enable more reliable and efficient communication between IoT devices, facilitating real-time health monitoring and telemedicine applications [175].
9.2.3. AI Integration
Using AI to analyse data collected from IoT devices to predict health issues and suggest preventive measures [32]. This innovation will enhance diagnostic accuracy and personalised treatment plans, improving overall patient outcomes [263].
9.2.4. Blockchain for Security
Implementing blockchain technology to secure patient data and ensure transparent and tamper-proof data transactions [260]. This will enhance data integrity and security, addressing significant privacy concerns in IoT healthcare systems [245].
9.3. Compare and Contrast
Different IoT Healthcare Systems.
9.3.1. Wearable Health Monitors Versus Remote Patient Monitoring Systems
- •
Wearable Health Monitors:
- -
Strengths: Ongoing monitoring of vital signs, including HR, activity levels and sleep patterns [264].
- -
Weaknesses: Often limited by battery life and data accuracy, especially in low-cost devices [265].
- •
Remote Patient Monitoring Systems:
- -
Strengths: Offer comprehensive monitoring of chronic conditions with higher accuracy and reliability [266].
- -
Weaknesses: Typically, it is more expensive and requires more extensive infrastructure for data management [267].
9.3.2. Cloud-Based Versus Edge-Based IoT Systems
- •
Cloud-Based Systems:
- •
Edge-Based Systems:
9.3.3. Traditional IoT Security Protocols Versus Blockchain-Based Security
- •
Traditional IoT Security Protocols:
- •
Blockchain-Based Security:
- -
Strengths: Provides decentralised and tamper-proof security measures, enhancing data integrity and transparency [272].
- -
Weaknesses: The project is currently in its initial implementation phase, and we are facing challenges related to scalability and resource consumption. These issues are being diligently assessed to ensure a successful progression [268].
- -
10. Conclusions
A comprehensive examination of IoT-based healthcare architecture and platforms reveals the ongoing global research efforts to integrate IoT into existing healthcare systems. This study delves into the technological innovations aiming to enhance healthcare delivery through the IoT. It focuses on IoT-driven healthcare services, which deal with paediatric and elderly care, chronic disease management, remote health monitoring and fitness tracking. The study also acknowledges the advancements in sensors, devices and internet applications that have led to the development of affordable healthcare gadgets, significantly expanding the scope of IoT-enabled healthcare. Addressing security concerns, the study identifies key challenges and proposes a model to mitigate risks associated with IoT healthcare systems. It also emphasises critical issues such as standardisation, network characteristics, business models, QoS and data protection, laying a solid foundation for further exploration of IoT healthcare solutions. The insights presented in this study regarding IoT and ehealth standards and guidelines are expected to benefit a wide range of stakeholders, including scientists, engineers, healthcare professionals and policymakers, in their collaborative efforts to advance IoT in healthcare automation. These findings are anticipated to guide ongoing initiatives aimed at enhancing the efficiency, security and accessibility of healthcare through IoT innovations.
Nomenclature
-
- AAL:
-
- Ambient assisted living
-
- ADR:
-
- Adverse drug reaction
-
- API:
-
- Application programming interface
-
- BG:
-
- Blood glucose
-
- BLE:
-
- Bluetooth low energy
-
- BP:
-
- Blood pressure
-
- CCD:
-
- Continuity of care document
-
- CVD:
-
- Cardiovascular disease
-
- ECG:
-
- Electrocardiogram
-
- EHR:
-
- Electronic health record
-
- ETSI:
-
- European Telecommunications Standards Institute
-
- GFR:
-
- Glomerular filtration rate
-
- GSM:
-
- Global System for Mobile Communications
-
- HR:
-
- Heart rate
-
- ICT:
-
- Information and communication technology
-
- IMU:
-
- Inertial measurement unit
-
- IoT:
-
- Internet of Things
-
- IPv6:
-
- Internet protocol version 6
-
- LPWA:
-
- Low-power wide area
-
- MAC:
-
- Medium access control
-
- NAAT:
-
- Nucleic acid amplification test
-
- NFC:
-
- Near-field communication
-
- PHY:
-
- Physical layer
-
- QoS:
-
- Quality of service
-
- RPMA:
-
- Random phase multiple access
-
- RPM:
-
- Remote patient monitoring
-
- RDS:
-
- Respiratory distress syndrome
-
- RFID:
-
- Radio frequency identification
-
- SMA:
-
- Semantic medical access
-
- SOA:
-
- Service-oriented approach
-
- TCP/IP:
-
- Transmission control protocol/internet protocol
-
- UDP:
-
- User Datagram Protocol
-
- WBAN:
-
- Wireless body area network
-
- Wi-Fi:
-
- Wireless fidelity
-
- WiMAX:
-
- Worldwide Interoperability for Microwave Access
-
- WLAN:
-
- Wireless local area network
-
- WSN:
-
- Wireless sensor network
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Attiq Ur Rehman and Songfeng Lu: data curation, methodology, visualisation, formal analysis and writing–original draft; Md Belal Bin Heyat and Muhammad Shahid Iqbal: conceptualisation, formal analysis, project administration, resources, software, validation and writing–original draft; Saba Parveen: data curation, methodology, visualisation, funding acquisition, investigation, validation and writing–original draft; Mohd Ammar Bin Hayat: data curation, validation, investigation, software, visualisation and writing–original draft; Faijan Akhtar: conceptualisation, supervision, resources, visualisation, funding acquisition and writing–review and editing; Muhammad Awais Ashraf: data curation, methodology, visualisation, funding acquisition, investigation, validation and writing–original draft; Owais Khan: conceptualisation, supervision, resources, visualisation, funding acquisition and writing–review and editing; Dustin Pomary and Mohamad Sawan: data curation, supervision, resources, funding acquisition, validation and writing–review and editing. All authors read and agreed to the publication.
Funding
This work was supported by the Hangzhou Postdoctoral Research Subsidy Project (103120036582502).
Acknowledgements
The authors would like to thank Kaishun Wu, Dakun Lai, Naseem Ahmad, Shailendra Singh, V.S. Chandel, Maroof Siddiqui, Mansoor Ahmad, M.A. Ansari, Muhammad Bahri, Fateh Ullah, Zina Fredj, Zakaria Jamali, Ijaz Gul, Nasir Ilyas, Yitian and Shuyun for their help, support, guidance and motivation for this study.
Open Research
Data Availability Statement
All data used in this study are available in this paper.




