The Effect of Stress Ball Utilization on Dyspnea Severity and Anxiety Level in Patients Receiving Nebulizer Therapy: Randomized Controlled Study
Abstract
Aim: The study primarily aimed at examining the effect of stress ball utilization on dyspnea and anxiety during nebulizer therapy. The secondary aim was to determine the effect of stress ball utilization on the duration of therapy and vital signs.
Methods: The study has a randomized controlled experimental design. The study population consisted of inpatients receiving nebulizer therapy. A total of 80 patients, 40 in the intervention group and 40 in the control group, were included in the sample. The study was conducted between October 2023 and March 2024. Patients in the intervention group were asked to use a stress ball during nebulizer therapy. Data were collected using a Patient Information Form, the Visual Analog Scale, and the State-Trait Anxiety Inventory. Descriptive statistics, Chi-square, paired test, and one sample t-test were used in data analysis.
Results: The mean age of the patients was 65 years and over and 78% of them had COPD. Stress ball utilization caused a significant effect on the severity of dyspnea (intervention: t = 2.862, p < 0.001; control: t = 2.755, p < 0.001) and anxiety levels (intervention: t = 4.647, p < 0.001; control: t = 6.597, p < 0.001) in intragroup comparisons. In intergroup comparisons, a significant difference (tı = 4.455, p < 0.001) was obtained in anxiety level with a high effect (d = 0.70). In addition, the durations of nebulizer (minutes) administration were significantly (p < 0.001) longer in the intervention group (19.10 ± 11.95) than in the control group (13.16 ± 3.02). Stress ball utilization did not affect vital signs and saturation values (p > 0.05).
Conclusions: Utilization of a stress ball during nebulizer therapy has a positive effect on reducing anxiety levels and prolonging the duration of nebulizer use.
Trial Registration: ClinicalTrials.gov identifier: NCT06297356
Summary
-
What’s known
- •
The use of nebulizer therapy is extremely important for symptoms caused by respiratory system diseases. The use of nebulizer results in relief of symptoms.
- •
However, using a nebulizer may not always be comfortable. The treatment method may cause discomfort to the patient.
- •
The use of a stress ball is a simple and practical tool for clinical use that can change patients’ focus by distributing attention to different directions.
-
What’s new
- •
This is the first study to examine the effects of using a stress ball during nebulizer therapy.
- •
It has been observed that with the use of a stress ball, the level of anxiety that occurs during nebulizer therapy decreases and the session duration can be continued for a sufficient length of time.
- •
With the use of stress balls, rapid results were obtained in a short time and the anxiety level of the patients was taken under control. Thus, it has been observed that dyspnea and other negative symptoms that anxiety can cause can be alleviated. Due to these effects, it is recommended to use a stress ball while using a nebulizer.
1. Introduction
Among chronic diseases, respiratory diseases are the third leading cause of death [1]. Therefore, the treatment and care of respiratory diseases, which cause various symptoms, are important. Patients suffer from shortness of breath, cough, phlegm, and fatigue [2]. The most effective approach to symptom relief and prevention is inhaler and aerosol therapies [3, 4].
Airway patency must be secured for airways with obstruction and restriction to perform respiration effectively. For this purpose, bronchodilator drugs are used. These drugs are available in different forms, including short- and long-acting, and are sent directly into the patient’s airways through inhalation [2, 4]. After an appropriate time, the sedimented drug diffuses into the small airways. Thus, it helps to soften and remove the secretion obstructing the alveoli and relieve inflammation [5]. Compared to inhalers, aerosol drugs are advantageous as they can reach the lungs at high doses in a short time. For this purpose, nebulizer devices are important tools that help the patient breathe by vaporizing the drug in the aerosol form allowing him/her to continue the treatment outside the hospital as they can be used at home [6]. Furthermore, while particles larger than 5 nanomicrons in inhaled drugs accumulate in the retropharynx and are swallowed, particles sized between 2–5 nanomicrons can pass into the lungs and sediment. However, the sedimentation rate of these particles is very slow and requires long (at least 10 s) breath holding [5, 7]. In this case, instead of using inhalers, it is advantageous to use a nebulizer to deliver smaller particles of aerosolized drugs to the lungs.
Nebulizers, which are frequently preferred when symptoms are exacerbated and the patient needs airway patency in a short time, provide improvement in symptoms in a short time. Approximately 4 mL of the drug is poured into the medicine cup and the treatment is continued for an average of 5–25 min [8–10]. A nasal oxygen cannula or oxygen mask is generally preferred for this purpose. An average flow rate of 6–8 L/min is recommended [9, 10]. Although nebulizers have a higher therapeutic effectiveness than inhalers, they have some disadvantages. In particular, the delivery of a drug with a certain flow rate may be uncomfortable for the patient at first [11, 12]. In previous studies, it has been reported that patients’ stress increases during the treatment and therefore they shorten the treatment than required [13]. Inhalation of the liquid drug poured into the reservoir should last an average of 10 min until it is finished [10]. The patient should stop the treatment when the vapor coming from the mask decreases or when he/she sees that the drug in the reservoir has run out. Especially outside the hospital, the patient is expected to actively continue to use this device. However, it has been reported in studies that patients are not sufficiently successful in the application, cannot extend the duration of therapy as required, and do not inhale the drug in the appropriate position [8, 11, 14]. For these reasons, the expected drug efficacy is not achieved. An important problem seen in patients with obstructed airways is fatigue, stress, and anger due to the increased amount of CO2 [15]. In this situation, the patient may not be patient enough for the treatment. The patient may feel uncomfortable with the cannula or mask that must be used during the treatment. Increased anxiety may cause the patient to feel worse, particularly shortness of breath [16–19]. For this reason, the aim should be to minimize the discomfort caused by the device by distracting the patient during nebulizer therapy and to keep the therapy time as active as possible.
A stress ball is a very practical and easily accessible tool. It can be used medically for therapeutic purposes as well as for distraction and relaxation. Nurses can use distraction techniques to benefit patients in patient care. Some procedures in hospitals are uncomfortable for most patients. In this case, the utilization of a stress ball can help the individual to feel calmer during the procedure. In some studies, it was reported that the use of a stress ball during swab sampling for polymerase chain reaction (PCR) tests reduced pain and fear in children [20] and adolescents [21]. In another study, it was stated that the use of a stress ball during endoscopy decreased pain and anxiety levels in patients [22]. Based on the studies in the literature, it was thought that stress ball utilization may be effective in distracting during applications where the patient may feel discomfort, thus alleviating the feeling of discomfort. This is considered an important nursing intervention. Since nebulizer therapy is a treatment option that requires the patient to inhale drugs at a certain flow rate for a certain period and the patient experiences discomfort due to the tools used, the effect of the stress ball has been the subject of research. Since there is no such study in the literature, it is thought that the results of the study will guide patients and health professionals. The study primarily aimed to determine the effect of stress ball utilization on dyspnea severity and anxiety level during nebulizer therapy. The secondary aim was to determine the effect of stress ball utilization on the duration of nebulizer therapy, blood pressure, respiratory rate, and saturation.
Consistent with the conceptual framework that guides our study, the following hypotheses were tested:
H0-1: Stress ball utilization during a nebulizer session has no effect on dyspnea severity in individuals receiving nebulizer therapy.
H1-1: Stress ball utilization during a nebulizer session has an effect on dyspnea severity in individuals receiving nebulizer therapy.
H0-2: Stress ball utilization during a nebulizer session has no effect on anxiety levels in individuals receiving nebulizer therapy.
H1-2: Stress ball utilization during a nebulizer session has an effect on anxiety levels in individuals receiving nebulizer therapy.
H0-3: Stress ball utilization during a nebulizer session has no effect on the duration of therapy in individuals receiving nebulizer therapy.
H1-3: Stress ball utilization during a nebulizer session has an effect on the duration of therapy in individuals receiving nebulizer therapy.
H0-4: Stress ball utilization during a nebulizer session has no effect on vital signs in individuals receiving nebulizer therapy.
H1-4: Stress ball utilization during a nebulizer session has an effect on vital signs in individuals receiving nebulizer therapy.
2. Methods
2.1. Study Design, Population, and Sample
Among quantitative research methods, the study was conducted as a randomized controlled experimental study.
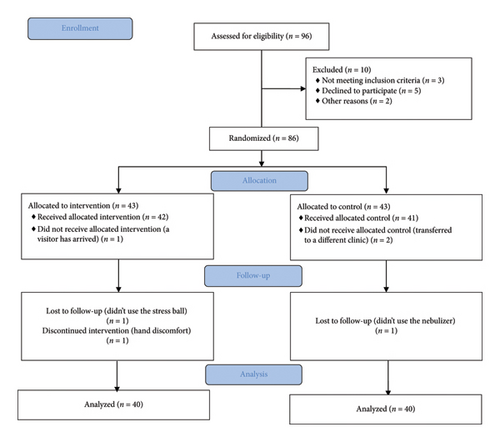
The population consisted of inpatients receiving nebulizer therapy in the pulmonology unit of a training and research hospital. The sample size was calculated in G. Power Version 3.1.9.2 (Franz Faul, Universitat Kiel, Germany) according to the two independent groups, the difference between two independent means, and the two-tail analysis of variance hypothesis test. In the power analysis performed based on the sample group of a similar study in the literature [22], the study was completed with a sufficient sample size, achieving a power of 1 − β, α = 0.05, and an effect size greater than 0.80. Accordingly, the sample size was determined as 34 patients in the intervention and control group for a power of 99%. Considering possible data loss, a total of 80 patients, including at least 40 patients in the intervention and control groups each, were reached. The sampling processes of the patients are shown in the Consolidated Standards of Reporting Trials (CONSORT) diagram (Figure 1).
In line with the inclusion criteria, having experience using an aerosol drug with a nebulizer individually at home for at least 1 year, having been hospitalized in the pulmonology unit for at least 2 days, being prescribed nebulizer drug (salbutamol 4 × 1, budesonide 2 × 1) therapy at least 2 times a day with a total of 4 mL into the reservoir at a time, using the same type of medication at home and in the hospital, being able to use the stress ball as shown during nebulizer use, and volunteering to participate in the study were included in the research.
Not using the same language as the researchers and having communication barriers, not willing to participate in the study, being aged younger than 18, having a psychiatric diagnosis, severely ill patients (those with low SpO2 levels or altered consciousness due to hypoxia), not being alone in the room during the study, having joint disorders in the hand such as arthritis, and having a history of hand surgery or prosthesis affecting the movement of the fingers and muscle strength of the hand were excluded from the study.
2.2. Randomization
The patients were randomly assigned to the groups to avoid bias. For this purpose, the computer-based https://www.random.org website was used. Accordingly, patient numbers were assigned to the intervention and control groups. The patients and the researcher could not be blinded due to the design of the study. However, during the analysis process, the groups were defined as A and B, and the evaluator was blinded to the groups. The CONSORT guidelines were adopted in this study [23].
2.3. Data Collection
After receiving the necessary approvals, the study was carried out with patients who met the inclusion criteria, between October 2023 and March 2024 using the face-to-face interview method in the patient rooms. Initially, the purpose of the study was explained to the patients and how to perform the application was demonstrated by the researchers. The researchers are academic nurses who have a PhD in this field and experience working in respiratory system diseases. A respiratory nurse also provided support at the clinic. Patients who did not have any problems using the stress ball and knew how to administer nebulizer therapy under the supervision of a nurse were told that they should start using the stress ball simultaneously when they started treatment and that they should continue to do so as long as they could. At this stage, they were especially asked to use the nebulizer as usual and not to make any changes. Patients used the stress ball once. The researchers filled out the forms before and after nebulizer therapy. The data were collected using a Patient Information Form, the Visual Analog Scale (VAS), and the State-Trait Anxiety Inventory (STAI). The application of the forms took an average of 30 min for each application.
2.3.1. Patient Information Form
The form was created by the researchers based on the relevant literature [20–22] and consists of questions regarding patients’ age, gender, diagnosis, and duration of nebulizer therapy in minutes.
2.3.2. VAS
It is a one-dimensional scale that is often preferred to measure dyspnea severity in patients. The scale can be scaled from 0–100 mm (0–10 cm). Patients are asked to mark the degree of dyspnea they feel at that moment. Zero indicates no dyspnea, and 100 mm indicates the most severe dyspnea. Responses of 0–0.4 mm are classified as no dyspnea, 0.5–40.4 mm as mild dyspnea, 40.5–70.4 mm as moderate dyspnea, and 70.5–100 mm as severe dyspnea [24]. The Cronbach’s alpha coefficient was not calculated since it is a one-dimensional scale.
2.3.3. STAI
STAI, which is a self-assessment questionnaire that enables the individual to evaluate oneself, consists of 20 items and has a four-point Likert-type rating. Ten items in the scale are reverse-scored. The total score is obtained by adding the constant number 50 to the total weighted score difference obtained. The minimum score obtainable from the scale is 20, and the maximum score is 80. A score below 36 indicates no anxiety; a score between 37 and 42 indicates mild anxiety; a score of 42 and above indicates high anxiety [25]. In our study, Cronbach’s alpha coefficient of the scale was found to be 0.71, which is within the appropriate limits.
2.4. Data Analysis
The data obtained from the study were analyzed using SPSS V25 (IBM Corp., Armonk, New York, USA). Clinical parameter distributions were tested for normality by the Shapiro–Wilk test. Descriptive statistics were expressed as number (n), percentage (%), and mean ± standard deviation (M ± SD). Chi-square analysis was used to compare categorical variables. The paired test was used for intragroup comparison, and the one-sample t-test was used for intergroup comparison. Statistical significance was accepted as p < 0.05.
2.5. Applications Performed to the Intervention Group
Initially, the patients who met the inclusion criteria were interviewed and the forms were applied after receiving patient consent. Pretest dyspnea severity, anxiety level, respiratory rate, pulse rate, blood pressure, and oxygen saturation values were recorded. The duration of therapy was observed by the researcher. The nebulizers used in the hospital were home-use devices that were not connected to the central oxygen system and were used manually (Armoline Piston Compressor Nebulizer Al200, Figure 2). Therefore, the patients included in the study were those who had been prescribed to use nebulizers at home for at least 1 year and could use the device individually. It was taken care that all patients had the same type of home nebulizer. All patients included in the sample were those using compressor type-nebulizers at home. The purpose of the stress ball utilization and how to use it were then explained to the patient. Before starting the therapy, it was evaluated whether the patient could use the stress ball appropriately. In patients who did not have any problems with the application, nebulizer therapy was initiated by the researcher, and they were told to use the stress ball simultaneously. In particular, it was emphasized that the stress ball utilization should be continued as long as the device was working. When the device started, a stopwatch was set on the smartphone and the duration of therapy was recorded. No guidance was given regarding the duration of therapy. The patient was asked to decide similarly to how many minutes he/she always used the nebulizer while receiving his/her routine treatment and when to terminate the treatment. To prevent the patient from being influenced by the researcher, the researcher waited in front of the room after completing the procedures, at a very close distance from the patient, but out of the patient’s sight. The important point here was that the researcher heard the patient’s device. The patient was expected to turn off the device on his/her own decision. When the patient turned off the nebulizer, the researcher stopped the stopwatch and recorded the time. After the treatment ended, the patient’s post-test values were measured.

2.5.1. Stress Ball Utilization
Stress balls are soft sponges with a diameter of approximately 2–4 cm (Figure 3). The lightest balls at the beginner level were used for the patients. Each patient was given a stress ball of the same brand and properties. The patients were told to take the stress ball in the hand of their choice and to squeeze and relax it in the palm of their hand at 2–3 s intervals. The duration of the application was decided by the patient. The researcher only observed whether the patient squeezed the stress ball accurately. The duration of the nebulizer procedure was monitored using a stopwatch on the researcher’s phone. If the patient did not volunteer to use the stress ball or wanted to terminate the treatment, the treatment was terminated immediately, and the results were not included in the study findings.

2.6. Applications Performed to the Control Group
The patients in this group did not use a stress ball. The forms were applied before and after the study. The patients continued their prescribed routine nebulizer therapy. After the study was completed, the use of the stress ball was demonstrated to the patients in this group to prevent bias and the purpose of its use was explained.
3. Results
The demographic characteristics of the patients who completed the study were compared, and there was no statistically significant difference (p > 0.05). This indicated that the intervention and control groups were similar (Table 1). The mean age of the patients was over 65 years, and 64% of them were male. Of those who were prescribed nebulizer therapy, 78% were diagnosed with COPD and 22% with asthma. Of the patients, 49% had been diagnosed for 1–5 years.
| Variables | Intervention n (%) | Control n (%) | Test | p |
|---|---|---|---|---|
| Age (mean ± SD) | 72.65 ± 10.96 | 67.24 ± 11.27 | 0.234 ∗ | 0.064 |
| Gender | ||||
| Female | 15 (37.5) | 14 (35.0) | 3.739 ∗∗ | 0.053 |
| Male | 25 (62.5) | 26 (65.0) | ||
| Diagnosis | ||||
| COPD | 29 (72.5) | 33 (82.5) | 1.147 ∗∗ | 0.462 |
| Asthma | 11 (27.5) | 7 (17.5) | ||
| Nebulizer treatment duration | ||||
| 6–10 min | 5 (12.5) | 17 (42.5) | 4.287 ∗∗ | 0.056 |
| 11–15 min | 25 (62.5) | 19 (47.5) | ||
| 16–20 min | 10 (25.0) | 4 (10.0) | ||
| Do you think your time is enough? | ||||
| Yes | 38 (95.0) | 34 (85.0) | 2.315 ∗∗ | 0.128 |
| No | 2 (5.0) | 6 (15.0) |
- ∗ t-test.
- ∗∗X2 test.
The severity of dyspnea was 67.12 in the intervention group and 69.93 in the control group. After nebulizer therapy, there was a significant intragroup difference in the mean pretest–post-test total scores in the intervention (t = 2.862, p < 0.001) and control (t = 2.755, p < 0.001) groups. However, there was no significant difference between the post-test mean scores of the two groups (t = 1.599, p = 0.114) (Table 2). According to this finding, hypothesis H0-1 was accepted.
| Groups | Pretotal | Posttotal | Test | Cohen’s d | 95% CI | ||
|---|---|---|---|---|---|---|---|
| LLCI | ULCI | ||||||
| Dyspnea | Intervention (M ± SD) | 67.12 ± 16.04 | 64.67 ± 17.24 |
|
0.26 | 1.120 | 10.270 |
| t = 2.862 p < 0.001 | |||||||
| Control (M ± SD) | 69.93 ± 12.96 | 68.66 ± 12.91 | |||||
| t = 2.755 p < 0.001 | |||||||
| Anxiety | Intervention (M±SD) | 43.05 ± 12.79 | 38.20 ± 10.99 | tı = 4.455 p < .001 | 0.70 | 1.498 | 14.351 |
| t = 4.647 p < 0.001 | |||||||
| Control (M±SD) | 54.03 ± 16.02 | 47.43 ± 14.88 | |||||
| t = 6.597 p < 0.001 | |||||||
- Note: t = paired t-test; tı = independent t-test. Values with p < 0.05 are indicated in bold.
- Abbreviations: LLCI, lower limit confidence interval; ULCI, upper limit confidence interval.
The anxiety level of the patients was 43.05% in the intervention group and 54.03% in the control group. After nebulizer therapy, there was a significant intragroup difference in the mean pretest–post-test total scores in the intervention (t = 4.647, p < 0.001) and control (t = 6.597, p < 0.001) groups. In terms of the anxiety level, there was a significant difference in the mean post-test scores between the groups (t = 4.455, p < 0.001) and the effect size was high (d = 0.70) (Table 2). According to this finding, hypothesis H1-2 was accepted.
When the intervention and control groups were compared in terms of the durations of nebulizer therapy, there was a statistically significant difference between the groups (p < 0.001) and the duration of therapy was shorter in the control group than in the intervention group (Table 3). According to this finding, hypothesis H1–3 was accepted.
| Groups | Treatment durations (minutes) (M ± SD) | Test | p |
|---|---|---|---|
| Intervention | 19.10 ± 11.95 | 234.490 | p < 0.001 |
| Control | 13.16 ± 3.02 |
- Note: Values with p < 0.05 are indicated in bold.
The vital signs of the patients in the intervention and control groups were compared. According to the analysis, there was no statistically significant difference in the breathing rate/min, pulse/min, systolic blood pressure/mmHg, diastolic blood pressure/mmHg, and SpO2 (%) values of the patients in intragroup and intergroup comparisons (Table 4). According to this finding, H0-4 was accepted.
| Vital signs | Intervention | Control | p∗ | |
|---|---|---|---|---|
| Breathing rate (min) | Before | 15.32 ± 3.67 | 14.94 ± 2.98 | 0.317 |
| After | 16.12 ± 3.7 | 15.24 ± 3.71 | 0.664 | |
| p∗∗ | 0.420 | 0.560 | ||
| Pulse (min) | Before | 77.29 ± 11.61 | 78.34 ± 10.50 | 0.272 |
| After | 80.27 ± 11.75 | 80.58 ± 9.34 | 0.362 | |
| p∗∗ | 0.783 | 0.243 | ||
| Systolic blood pressure (mmHg) | Before | 116.25 ± 17.40 | 116.33 ± 16.47 | 0.328 |
| After | 115.41 ± 12.23 | 113.76 ± 14.83 | 0.447 | |
| p∗∗ | 0.719 | 0.124 | ||
| Diastolic blood pressure (mmHg) | Before | 71.11 ± 10.23 | 71.24 ± 12.52 | 0.901 |
| After | 71.38 ± 9.90 | 70.72 ± 10.00 | 0.446 | |
| p∗ | 0.311 | 0.179 | ||
| SpO2 (%) | Before | 91.57 ± 5.01 | 89.96 ± 6.04 | 0.136 |
| After | 93.87 ± 7.15 | 90.20 ± 4.54 | 0.172 | |
| p∗∗ | 0.538 | 0.384 | ||
- ∗Mann–Whitney U Z test.
- ∗∗Wilcoxon Z test.
4. Discussion
The majority of the participants in our randomized controlled study, in which the effect of stress ball utilization on dyspnea severity and anxiety level in patients receiving nebulizer therapy was examined, were elderly and male individuals diagnosed with COPD. Our study findings are consistent with the patient population reported in the literature [2, 26]. Increased particle exposure in the airways with advanced age, constraints in alveolar airflow, and thickening of mucus secretion lead to a higher incidence of obstructive and restrictive diseases [2]. These physiological changes cause the patient to experience various symptoms.
The main symptoms seen in patients are dyspnea, cough, phlegm, and fatigue [27]. The use of appropriate treatment methods is extremely important in the management of symptoms. The most used treatment option in COPD and asthma is inhaler drugs. These drugs have an advantage over systemic treatment in that they deliver the drug directly to the airways and have fewer side effects. Another important advantage is that they act in a short period [2–4, 6]. However, in some cases, inhaler drugs alone are not sufficient. In particular, if the patient experiences severe dyspnea, is unable to maintain hand-breath coordination (for metered dose inhalers), or is too tired to use muscle strength, this may result in an inability to exert sufficient effort to use the inhaler. In this case, the drugs must be delivered to the patient via an external airflow. In this approach, namely, aerosol therapy, inhaled drugs are delivered directly to the patient’s lungs. Another advantage of aerosol therapy is that higher concentrations of drugs compared to inhaled drugs are easily diffused through the aerosol form [5–10]. Nebulizer devices are prescribed to many patients both in cases requiring emergency treatment such as exacerbations and for out-of-hospital utilization [13]. The patients included in our study had previous experience of using nebulizers at home. This allowed the assessment of the patient’s skill in this form of treatment used in the hospital.
Besides their advantages and positive effects, nebulizers also have some disadvantages. As stated in the Introduction section, the medicine must be inhaled for the appropriate time [8–10]. The patient must be in a sitting or semisitting position and inhale the drug through a nasal cannula or mask. It has been observed that patients experience uneasiness during the use of these devices and that inhalation becomes difficult in some cases due to the effect of pressurized air. On the other hand, the fact that the patient must be in an environment with an electrical socket for an average of 10–15 min also causes limitations in use. In some cases, drug-induced irritation of the nasal and ocular mucosa has been reported [13, 28, 29]. Considering all these circumstances, treatment with a nebulizer is advantageous, but it also poses various problems that can lead to increased anxiety and exacerbation of dyspnea. In some studies, it has been shown that dyspnea is also exacerbated in people with high levels of anxiety [16, 18, 19]. Various studies have also shown that anxiety increases in patients using nebulizers [11, 12, 29, 30].
In our study, it was observed that the dyspnea severity of the patients was high before the application. This result was expected as the patient expressed dyspnea before the treatment. The patients described dyspnea, which is a subjective feeling, as not being able to take enough breath and feeling like drowning [31, 32]. A stress ball is a simple and practical tool to distract the patient from these feelings, pain, and negative thoughts by drawing their attention to different things. Especially in young patients and adults, the procedures can cause intense anxiety and fear and may cause unwanted reactions in patients. In various studies conducted in our country, it has been reported that stress ball utilization distracts the patients and facilitates the procedures [20–22]. However, there is no research in the literature in which the effect of the use of a stress ball on dyspnea was directly examined, while O’Donnell emphasized the importance of evaluating dyspnea with new approaches and trying to alleviate it in 2020 [31]. In this context, it is obvious that our study is unique and will shed light on future studies. In our study, it was observed that dyspnea severity decreased in the intervention and control groups after the use of the stress ball compared to the pretreatment period (Table 2). This is expected due to the effect of drugs. When the groups were compared, no significant difference was found between the two groups. One of the most important factors that may have affected this result is that the stress ball may have been used for only one session. The other factor is that applications that will directly affect the airways are more effective in alleviating a symptom such as dyspnea, which is characterized by airflow restriction. The main expected effect of the stress ball is to reduce the anxiety level and alleviate the resulting dyspnea.
It was observed that the patients had high levels of anxiety before the study. Anxiety levels may increase due to factors such as receiving treatment in a hospital and moving away from routines and comfort zone. Especially respiratory system diseases such as COPD and asthma are associated with respiration, and the feeling of running out of breath triggers thoughts of death in patients [33]. Such negative thoughts may cause patients to experience high levels of anxiety. In our study, the anxiety levels of the patients decreased significantly when they used a stress ball during one nebulizer session. However, in the intergroup comparison, the decrease in the intervention group was significantly higher than in the control group. According to the effect size, it was understood that the effect in the intervention group was strong (d = 0.70). Such benefit of the stress ball showed a desirable effect in alleviating momentary anxiety. It is a pleasing result that by distracting the patients’ focus to the stress ball during the nebulizer session, the disturbing sound of the device and the physical discomfort caused by the cannulas and drugs were felt less and the anxiety due to the feeling of being dependent on the device was alleviated, albeit for a limited period. In various studies, it has been reported that stress ball utilization provides positive effects in reducing anxiety levels in patients [22]. It was thought that this result obtained from our study may contribute positively to the duration of therapy by reducing anxiety in patients.
Continuing nebulizer therapy using a stress ball had a positive effect on the adequacy of the duration of therapy in the intervention group. Thus, the patient was allowed to wait until enough time so that the drug amount in the reservoir would not be wasted. In the literature, it has been reported that patients apply nebulizer therapy for insufficient time [8–10]. In our study, thanks to the use of the stress ball, it was possible to continue nebulizer treatment for more than 19 min until the drug in the reservoir ran out. We think it is an important result.
It has been reported that the increase in anxiety and dyspnea in patients may cause a decrease in oxygen saturation due to the fight-or-flight response, as well as physiological changes such as increased pulse, respiratory rate, and blood pressure [17]. Based on this information, the effect of stress ball utilization on some parameters was examined in our study; however, it was observed in intragroup and intergroup comparisons that it did not contribute positively (Table 4). As we mentioned before, this result showed that interventions that have a direct effect on the airways can be effective in vital signs and saturation values. However, although no significant results were obtained in our study, this application, which is easily applicable and accessible with the use of a stress ball in longer sessions, should be further tested for improvements in certain parameters of patients.
4.1. Strengths and Limitations
The strength of the study is its design. In this study conducted with a randomized control group, the effect of the stress ball was revealed. Thanks to this practical application, it was demonstrated that improvements in clinical parameters can be achieved with nonpharmacologic methods. Another important strength of this study is that there is no study in the literature in which stress ball utilization during nebulizer therapy in adults has been explored. It is thought that the results of this study will shed light on future studies.
The study has some limitations. The main one is that the stress ball was used in only one nebulizer session. The work intensity of the researchers is one of the most important reasons for this problem. However, it is considered highly important to investigate the long-term effects of stress ball use on dyspnea severity and anxiety levels in patients undergoing nebulizer therapy. Another limitation is that the study was carried out only in the hospital. Inpatients are a group of patients whose clinical parameters have already deteriorated and need to be taken under control. However, the hospital setting is the main cause of anxiety. Due to these effects, patients may not have been able to continue the application with the desired comfort and this may have affected the results. It is recommended that the study be conducted with different patient groups and in various settings (such as outpatient clinics and among individuals using home nebulizers) to enhance its generalizability. Another limitation is that the age or previous psychological experiences of the individuals may have affected the results. The results were based on the patients’ statements, and the subjective results stated by the patients were accepted as accurate.
5. Conclusions
In conclusion, it was found that the majority of our patients were individuals diagnosed with COPD and had high levels of dyspnea and anxiety. Thanks to stress ball utilization, dyspnea severity and anxiety levels decreased in the intervention and control groups. In intergroup comparisons, it was found that stress ball utilization had no effect on reducing the dyspnea level, whereas it had a great effect on reducing anxiety in the intervention group. In addition, patients in the intervention group continued nebulizer therapy for longer by using the stress ball. However, there was no difference in respiratory rate, pulse, blood pressure, and saturation parameters within and between the groups.
In line with all these results, it was determined that stress ball utilization in clinics for various diseases is very practical and accessible, causing the patient to relax by distracting and thus showing improvements in some clinical parameters. It is recommended that future studies be planned with more nebulizer sessions, with different patient groups, with large samples, and outside the hospital. Additionally, the effect of stress ball use on patients’ comfort levels can be investigated.
Ethics Statement
Ethical permission (Decision No: 1215; Decision Date: 09/27/2023) was obtained from the Izmir Bakircay University Non-invasive Clinical Research Ethics Committee to conduct the research. The institution permission (Number: E-10670833-000-212062524; Decision Date: 03/28/2023) was obtained from Kirsehir Ahi Evran University Training and Research Hospital. Furthermore, ethical principles and the Declaration of Helsinki were adhered to at all stages of the study. The patients were included in the study voluntarily, and informed consent was taken after explaining the purpose of the study.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Yasemin Ceyhan, Sevil Güler, and Seda Şahan made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; Yasemin Ceyhan carried out the implementation phase of the study; Yasemin Ceyhan, Sevil Güler, and Seda Şahan involved in the drafting of the manuscript or revising it critically for important intellectual content; and authors gave final approval of the version to be published.
Funding
The authors received no specific funding for this work.
Acknowledgments
The authors would like to thank the patients who contributed to the study. No AI software has been used in any section of the manuscript.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




