Clinical Efficacy and Safety of Upadacitinib Combined With a 308 nm Excimer Laser in the Treatment of Refractory Vitiligo Complicated With Atopic Dermatitis
Abstract
Vitiligo is autoimmune-induced skin depigmentation. Phototherapy is commonly used as the basic treatment for vitiligo; however, its curative effect is limited in some cases of refractory vitiligo. This study aimed to evaluate the clinical efficacy and safety of upadacitinib combined with a 308 nm excimer laser (308 nm EL) for treating refractory vitiligo with moderate-to-severe atopic dermatitis (AD). We analyzed the treatment of 19 Chinese patients with skin diseases and found that sex, disease duration, and skin type did not affect repigmentation, whereas age was negatively correlated with repigmentation. After 4 months of therapy, the overall remission degree of the vitiligo area severity index (VASI) score reached 55.00%, and the last 2 months were better than the first 2 months. The curative effect of vitiligo on the face and neck was better, with an improvement of > 70.00%, followed by the torso, arms, and legs. The VASI scores of the hands and feet were the worst, especially the feet which scored only 28.00%. The average improvement in the SCORing of AD (SCORAD) and dermatology life quality index (DLQI) scores was 41.89% and 49.12%, respectively. No serious adverse events were observed. Overall, upadacitinib combined with 308-nm EL showed promising clinical value for the treatment of refractory vitiligo.
1. Introduction
The global incidence of vitiligo is approximately 0.5%–2.0% [1, 2]. Recently, the role of the JAK/STAT pathway in vitiligo has been widely studied [3]. The expression of JAK1 and JAK3 in vitiligo, perivitiligo, and normal skin has been reported to show a decreasing trend, and the overexpression of JAK1 was inhibited by narrowband ultraviolet B (NB-UVB) therapy [4, 5]. As a selective JAK1 inhibitor, upadacitinib has a definite effect on moderate-to-severe AD and has been approved for clinical use; however, there are few studies on its use for the treatment of vitiligo [6].
The use of 308 nm excimer laser (308 nm EL) irradiation is an important method for treating vitiligo as it stimulates tyrosinase activity, increases melanin content, and regulates immune responses, among other photobiological principles [7, 8]. Phototherapy and JAK inhibitors may exert synergistic inhibitory effects on vitiligo. Therefore, we used upadacitinib combined with 308 nm EL to treat refractory vitiligo in patients with AD and observed its clinical efficacy and safety.
2. Materials and Methods
2.1. Patients
This study analyzed 19 Chinese patients with skin diseases who were treated at The First Affiliated Hospital of Hebei University of Traditional Chinese Medicine from March 2023 to May 2024. The inclusion criteria were refractory vitiligo (defined as a failure to respond after at least 3 months of conventional treatments, including calcineurin inhibitors, systemic steroids, and phototherapy.) with moderate-to-severe atopic dermatitis (AD) (SCORing of AD [SCORAD > 40]) [6] and had not been treated again for nearly 3 months. The exclusion criteria were history of cicatricial constitution, active tuberculosis infection or hepatitis B virus, pregnancy, perinatal period, cancer, previous history of systemic immunotherapy, and allergy to upadacitinib and its compounds. All participating patients fully understand and agree to the treatment systemic steroids, calcineurin inhibitors and phototherapy.
2.2. Methods of Study
This was a single-group, a single-arm, open-label trial consisting of a baseline period (24 h prior to treatment), a treatment period (4 months), and follow-up period (3 months after treatment). Patients were assessed and recorded at baseline and 2 and 4 months, every 30 days period constituted 1 month. The VASI and SCORAD scores were used to measure the severity of vitiligo and AD. The degree of remission in vitiligo and AD was represented by the mean percentage changes of VASI and SCORAD. The impact on the patients’ quality of life (QOL) was measured using the DLQI score. Adverse events (AEs) were recorded throughout the study.
2.3. Treatment Methods
Upadacitinib was administered orally (15 mg daily) and patients were treated with 308 nm EL twice weekly. The initial irradiation dose was determined according to the different parts of the body (50–400 mJ/cm2), and further adjusted according to the erythema status during treatment. The relevant adjustment plans are presented in Table 1.
| Red spot condition | Adjustment plan for laser (mJ/cm2) |
|---|---|
| No or duration (< 24 h) | Add 50 |
| Duration (24–48 h) | No change |
| Duration (48–72 h) | Reduce 50 |
| Duration (> 72 h) or pain or blister | Delay treatment and reduce 50∼100 |
2.4. Statistical Analysis
SPSS version (22.0 IBM America) was used for the data analysis. Statistical methods included t-test, repeated-measures analysis of variance (ANOVA), and Spearman’s correlation coefficient calculation. The statistical results were expressed as mean ± standard deviation (mean ± SD) and percentage. p < 0.05 indicated that the differences were statistically significant. Categorical data are presented as frequencies and percentages. GraphPad Prism 9.0 was used to plot the graphs.
3. Results
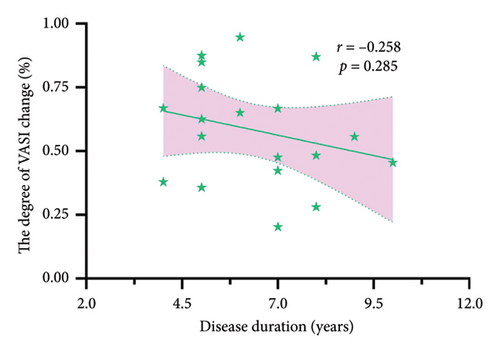
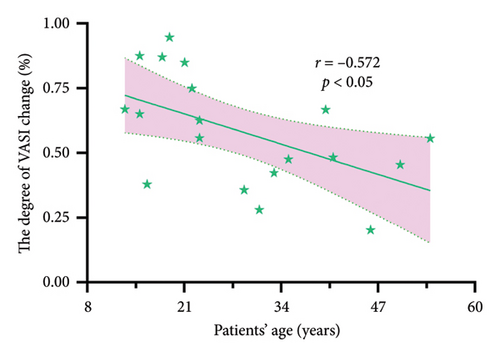
The relevant statistical information of the patient is presented in Table 2. The average age of the 19 patients was 28.63 ± 12.69 years, and the disease duration ranged from 4 to 10 years. Sex, Fitzpatrick skin type, and disease duration did not influence repigmentation (Figure 1(a) and Table 1) (p > 0.05), whereas age was negatively correlated with repigmentation (Figure 1(b)) (p < 0.05). After treatment, the leukoplakia was significantly relieved (Figures 2 and 3(a)).
| Variable | N | Percent change from baseline in VASI score at month 4 (mean ± SD) (%) | p value |
|---|---|---|---|
| Fitzpatrick skin type | |||
| III | 10 | 61.77 ± 21.09 | 0.465 |
| IV | 9 | 54.36 ± 22.08 | |
| Sex | |||
| Male | 11 | 54.24 ± 24.19 | 0.349 |
| Female | 8 | 63.79 ± 16.43 | |
- Note: Statistical analysis was performed using the t-test.
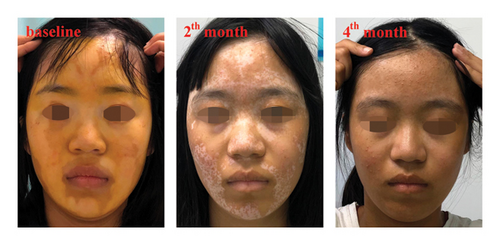
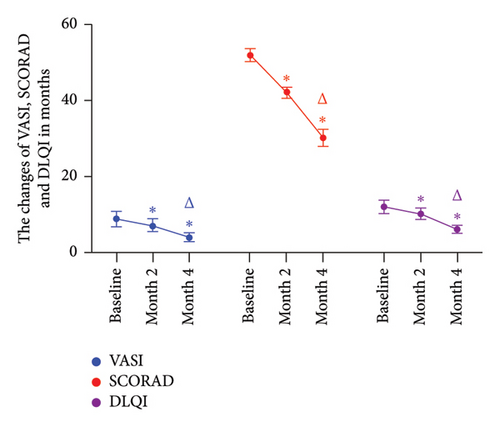
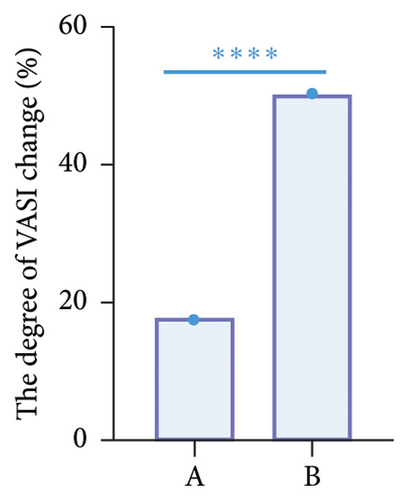
The distribution of leukoplakia and AEs in the patients is presented in Table 3. Compared to the baseline period, the VASI score of the patients decreased significantly over time (Figure 3(a)) (p < 0.05). The mean VASI score at baseline was 8.779 ± 1.980, which decreased to 4.042 ± 1.054 at month 4 of treatment, representing an average improvement of 58.26%. In addition, the reduction in VASI score during the last 2 months was greater than in the first 2 months (Figure 3(b); p < 0.0001), indicating a more pronounced remission during the final treatment phase. The improvement in facial vitiligo was better: one of the four patients had complete disappearance of facial leukoplakia, two patients had remission of > 80.00%, and one patient improved by > 70.00%. One patient with neck vitiligo showed 75.00% repigmentation. The torso, arms, and legs were followed, and the hands and feet were the worst, especially the feet, with only 28.00% recovery.
| Patient number | Body site involvement | AEs |
|---|---|---|
| 1 | Hands, arms, torso, legs | No |
| 2 | Hands, arms, torso, legs | No |
| 3 | Hands, legs, feet, face, neck | No |
| 4 | Hands, arms, torso, legs, feet, neck | No |
| 5 | Torso, legs | No |
| 6 | Arms, torso, legs | Acne |
| 7 | Hands, arms, torso | No |
| 8 | Hands, arms, torso, legs | No |
| 9 | Hands, arms, torso, legs, face | No |
| 10 | Hands, arms, torso, legs | Upper respiratory tract infections |
| 11 | Arms, torso, legs | No |
| 12 | Torso, legs | No |
| 13 | Torso, legs, face | No |
| 14 | Torso | No |
| 15 | Torso | No |
| 16 | Hands | Acne |
| 17 | Hands | No |
| 18 | Hands | No |
| 19 | Face | No |
Simultaneously, both AD and QOL were significantly improved (Figure 3(a)) (p < 0.05). The average SCORAD at the baseline was 51.895 ± 1.775, which decreased to 30.158 ± 2.300 at month 4 of treatment, indicating an average remission of 41.04%. Similarly, the mean DLQI score decreased from 12.00 ± 1.826 at baseline to 6.105 ± 0.976 at month 4 of treatment, with an overall response of 50.09%.
In our study, one patient (5.26%) showed transient mild acne, one patient (5.26%) had aggravation of previous acne, and one patient (5.26%) had mild upper respiratory tract infection symptoms, such as recurrent sore throat, all of which were common side effects of Upadacitinib. No serious AEs were observed.
4. Discussion
The pathogenesis of vitiligo is primarily induced by cell-mediated immune responses [9]. Cytotoxic CD8+ T cells induce the destruction of melanocytes, resulting in hypopigmentation plaques or white hair developing on the skin across the whole body [2]. IFN-γ plays an important role in this process; by secreting IFN-γ, T cells induce keratinocytes to produce chemokines, including CXCL10 and CXCL9, which activates the JAK/STAT pathway leading to the production of more chemokines to promote apoptosis in melanocytes [10, 11]. At the same time, CD8+ T and CXCR3+ cells are recruited to form a positive feedback loop, which aggravates melanocyte apoptosis [11].
The main treatment methods for vitiligo include phototherapy, calcineurin, topical steroids, and surgery [12]; however, their efficacy is limited, and new therapeutic methods are urgently needed. The role of the JAK/STAT pathway in vitiligo has been widely recognized, and JAK inhibitors are gradually entering into clinical use as new therapeutic drugs [13]. Upadacitinib is an oral selective JAK1 inhibitor that has been approved for moderate-to-severe AD and has the potential to treat vitiligo [14]. Therefore, we selected upadacitinib combined with 308-nm EL for the treatment of patients with vitiligo and moderate-to-severe AD who failed conventional treatment.
Our study found that upadacitinib combined with 308 nm EL had a positive therapeutic effect on refractory vitiligo and AD, suggesting that vitiligo and AD may be related. AD is a persistent inflammatory disease of the skin, and its pathogenesis involves the co-activation of different T cell subsets, along with a sustained increase in inflammatory cytokines, including Th1 (IFN-γ), Th2 (IL-31, IL-13, IL-4), and Th22 (IL-22) [15, 16]. The progression of vitiligo is also closely associated with T cells, which possess proinflammatory Th1-like characteristics [17]. Moreover, IL-22, IFN-γ, and other inflammatory factors were continuously increased in peripheral blood of patients with vitiligo [18]. Li et al. found that IL-4, a key inflammatory factor in AD, promotes the progression of vitiligo [19]. Furthermore, both vitiligo and specific dermatitis are related to the JAK/STAT pathway [20]. Epidemiological analyses from another perspective have confirmed that specific dermatitis can increase the risk of vitiligo [21]. These results indicate a potential association between vitiligo and AD; however, the specific association between the two conditions and treatment, as well as the stability of the curative efficacy, needs to be further studied.
There may be a synergistic effect of upadacitinib and 308 nm EL in increasing pigmentation. Phototherapy is associated with the production of inflammatory cytokines, such as IL-4, IL-5, IL-17, IL-31, and TNF-α, in the treatment of skin diseases, and many inflammatory factors are gathered in the JAK/STAT pathway [22, 23]. Currently, NB-UVB and 308-nm EL are the most commonly used phototherapies for the treatment of vitiligo. OZAWA et al. proved that apoptosis of T lymphocytes induced by NB-UVB may play a key role in vitiligo repigmentation [24]. As a monochromatic, coherent, short-pulse laser, 308 nm EL is more efficient than ordinary phototherapy and can induce T cell apoptosis better than NB-UVB [25]. Lauren et al. confirmed that T cell apoptosis sensitivity is negatively correlated with JAK/STAT pathway activity [26]. In a recent clinical study on oral upadacitinib alone, the average improvement in pigmentation within 4 months was 38.65% [27]; however, with the combined use of upadacitinib and phototherapy, the mean recoloring reached 55.00%, and the area exposed daily, such as the face and neck, improved significantly, with a repigmentation rate of > 70.00%. These results indicate that JAK inhibitors and phototherapy (especially 308 nm EL) may mutually promote the treatment of vitiligo; however, the specific relationship requires further exploration.
As molecular-targeted drugs, JAK inhibitors have some problems, such as weakened effects after drug withdrawal and disease recurrence [28]. Harris et al. reported a patient with alopecia areata and vitiligo whose facial vitiligo greatly improved after 20 weeks of oral ruxolitinib, but the pigmentation decreased again after drug withdrawal [29]. However, in the present study, no significant hypopigmentation was observed during the 3-month follow-up period, which may be related to the combined use of drugs and phototherapy. Additional control studies and extended follow-up observations are required in the future.
Due to the relatively small sample size in the study, we calculated the statistic power based on the main outcome measure, the VASI score. The mean and standard deviation of VASI values at baseline, month 2, and month 4 were 8.77 ± 8.63, 7.15 ± 7.19, and 4.04 ± 4.59, respectively. With α set at 0.05 and an autocorrelation coefficient of approximately 0.96, the statistical power was calculated using the Geisser-Greenhouse F-test algorithm in PASS21 software, under the condition of n = 19. The resulting power was > 0.99, indicating a high statistical power and suggesting that the result is reliable. However, further large-sample clinical studies are still needed to confirm these findings.
5. Conclusions
Our study demonstrated that the combination of upadacitinib and 308-nm EL is effective for refractory vitiligo combined with moderate-to-severe AD. However, the short follow-up time, small sample size, and lack of controlled studies are insufficient to support the generalization of our findings. Further large-scale prospective studies are needed to determine the safety and stability of this combinatorial approach, as well as the possible synergistic relationship between the drug and phototherapy.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Xiang Liu and Fangfei Zhou designed and conceived the experiments. Fangfei Zhou, Yuhang Liu, Qiuyue Jin, Wenzhao Han collected the data. Fangfei Zhou, Jiaqi Li and Weiye Li analyzed the data. Fangfei Zhou and Xiang Liu participated in drafting the manuscript, which was strictly revised by Xiang Liu. All authors participated fully in the study and confirmed the final version of the manuscript.
Funding
This work was supported by the Natural Science Foundation of Hebei Province (H2022423355).
Acknowledgments
We thank The First Affiliated Hospital of Hebei University of Traditional Chinese Medicine for platform support and all the participants involved in this study.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




