Effects of Water Bathing on Atopic Dermatitis Are Determined by the Constituents in the Water
Abstract
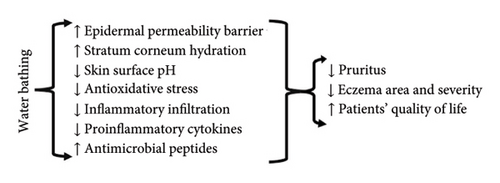
Atopic dermatitis (AD) is a common skin disorder. Although a wide range of therapeutic regimens are available, they have some limitations, including high medical costs. However, evidence suggests that adjuvant regimens such as water bathing are inexpensive and effective approaches for the management of AD. Bathing with either tap water or seawater alone can improve AD symptoms and signs. Combination of water bathing with topic emollient or corticosteroids can synergically alleviate AD. The underlying mechanisms by which water bathing benefits AD include improvements in epidermal function, inhibition of mast cell and Langerhans cell function, reductions in serine protease expression and activity, inhibition of cytokine expression, and upregulation of expression levels of antioxidant enzymes, as well as antimicrobial peptides. In this review, we summarize the effects of water bathing on AD in both humans and murine models as well as the underlying mechanisms.
1. Introduction
Atopic dermatitis (AD) is an immune-mediated skin disease, with a prevalence as high as 24% in the general population [1] and direct annual medical cost of up to US$7000/patient for moderate to severe AD in Europe [2, 3]. Although the results are controversy, a number of studies demonstrate an association of AD with extracutaneous disorders, including obesity and cardiovascular and psychological disorders [4–6]. Moreover, AD negatively impacts the quality of patients’ lives, which is correlated negatively with disease severity [7, 8]. Thus, development of regimens that can effectively mitigate AD is becoming emergent.
Currently, immunosuppressants, including biologics, glucocorticoids, vitamin D analogs, and calcineurin inhibitors, are primarily used to treat AD [9, 10]. Indeed, these agents can effectively alleviate AD, particularly in individuals with moderate to severe AD. But there are limitations in use of these drugs. For example, the high cost of biologics is a barrier to their wide use [11], particularly in developing countries. While glucocorticoids are effective and cheap, they can induce a variety of cutaneous and systemic adverse reactions, including skin atrophy, compromised epidermal permeability, hypertension, obesity, and osteoporosis [12, 13], which limit their usage, especially for long term. Even calcineurin inhibitors can induce renal fibrosis, disruption of epidermal permeability barrier, and other cutaneous disorders, such as rosacea, hyperpigmentation, skin burning, and erythema [14–16]. However, a great bulk of evidence indicates the benefits of water bathing or showering in the management of AD. A previous study demonstrated that once-daily shower for 2 weeks markedly lowered the AD symptom score in children [17]. Interestingly, shower-induced significant reduction in the scoring atopic dermatitis index (SCORAD) was only observed in children with severe or most severe AD [18]. Another study showed that lathering the skin lesions with 0.006% sodium hypochlorite for 2 min once daily significantly improved multiple abnormalities, including investigator’s global assessment (IGA), eczema area and severity index (EASI), SCORAD and body surface area scores, and reduction in glucocorticoid usage at week 3 in AD children [19]. Thus, shower with either regular tap water or water with additives benefits AD.
In addition, numerous studies demonstrate the benefits of water bathing for multiple health-related conditions, such as cardiovascular function, mental health, the quality of sleep, and cutaneous inflammation, in both murine models and humans [20–24]. In this review, we brief the benefits of water bathing in AD and the underlying mechanisms (see Figure 1).
2. Influence of Water Bathing on AD
The benefits of water bathing in skin conditions have long been appreciated [25]. Water bathing can alleviate several skin abnormalities, including pruritus, prurigo, ichthyosis, acne vulgaris, psoriasis, and AD [25–29]. The effects of water bathing on AD are summarized in Table 1 [30–65].
| Study | Water | Study protocol | Outcomes | References |
|---|---|---|---|---|
| Positive effects | ||||
| Animal model | High mineral spring water (HMSW) | While Skh1 mice were treated topically with DNCB to induce AD-like dermatitis for 3 weeks and were bathed in a cage which is 4 cm depth for 15 min daily, additional week of bathing was given after stopping DNCB treatment. |
|
[30] |
| Animal model | Concentrated deep sea water (CDSW) | NC/Nga mice were treated topically with DNCB to induce AD-like dermatitis for 3-4 times weekly for 2 weeks, followed by immersion in mineral water for 5 min daily for 2 weeks |
|
[31] |
| Animal model | Thermomineral water | Skh1 mice were treated topically with oxazolone to induce AD-like dermatitis for 2 weeks, followed by being bathed in water for 5 min daily for 1 week. |
|
[32] |
| Animal model | Various seawaters | DNCB was used to induce AD-like dermatitis. After establishment of AD-like dermatitis, mice were bathed with seawater for 20 min daily for 6 weeks. |
|
[33, 34] |
| Retrospective study | Unspecified water | In 75 patients with AD, topical corticosteroids were given for 3 min after bathing for 15–20 min daily for 2–21 days. |
|
[35] |
| Randomized and double blinded trial | 5% dead sea salt water | In a total of 30 patients with AD, their one forearm was immersed in 5% dead sea salt, while the other forearm was immersed in tap water for 15 min daily for 6 weeks. |
|
[36] |
| Randomized trial | 10% dead sea salt water | Patients with AD took bath for 15–30 min starting at least 4 min prior to exposure to UVB. Patients irradiated with UVB alone served as controls. All patients received 3–5 treatments per week for up to 35 treatments. |
|
[37] |
| Observational study | Thermal spring water | A total of 867 children aged ≤ 16 years took bath for 2–20 min once or twice daily for a total of 12–24 baths | Significant improvement in SCORAD | [38] |
| Randomized trial | Water at Lot Spa Hotel, Israel | Forty-seven AD children were exposed to dead sea sun twice daily followed by bathing in the spa for 28 days. Forty-four AD children treated with TCS served as controls. | SCORAD: Similar to the controls | [39] |
| Observational study | Water at Lot Spa Hotel, Israel | Seventy-two AD children were exposed to dead sea sun twice daily followed by bathing in the spa for 28 days. | SCORAD: Improved by 87.5% and 71.3%, respectively, immediately after and 3 months later | [40] |
| Open label, randomized trial | Thermal spring water | Fifty-four children with AD were bathed for 20 min once or twice daily for 2 weeks, while 50 children with AD treated with TCS once daily served as controls. |
|
[41] |
| Randomized trial | Unspecified water | Twelve AD children took bath once daily, while 16 AD children took bath twice a week for 2 weeks. | ↓ SCORAD | [42] |
| Randomized trial | Unspecified water | In a total of 40 patients, one group of AD children received bath for 10 min or less + moisturizer, twice weekly over 2 weeks, followed by twice-daily bath for 15–20 min + moisturizer twice weekly, over 2 weeks. Another group of patients did the inverse. Both groups of patients received the same moisturizer and low-potency TCS. | Twice-daily bath is more effective than twice-weekly bath in reduction of SCORAD | [43] |
| Observational study | Hot spring water | Seventy patients aged 12–80 years took spring bath for 10 min at 42°C twice daily for 22–204 days. Shower with regular water served as controls. | In comparison to regular water, spring water improved skin symptoms, lowered skin surface pH, and reduced Staphylococcus aureus on the skin | [44] |
| Observational study | Hot spring water | Forty-six patients aged 13–80 years took spring bath for 10 min at 10–42°C once or twice daily for 3–28 days. |
|
[45] |
| Observational study | Hot spring water | Forty-six patients aged 13–80 years took spring bath for 10 min at 10–42°C, followed by immediate topical white petrolatum 1–2 times daily for 75 ± 46 days. |
|
[46] |
| Observational study | Tap water at pH 3.0 | Eight patients with refractory AD were treated with wet-wrap dressing (desonide and moisturizer) for 40 min twice on day 1 and moisturizer alone twice on day 2. Another ten patients took acidic water bathing for 40 min twice daily for 2 days, followed by topical moisturizer. | Both regimens displayed comparable efficacy in improving the EASI, TEWL, stratum corneum hydration, and patients’ satisfaction. | [47] |
| Observational study | Hydrogen water | Five AD patients took water bath for 30 min daily for 8 weeks. |
|
[48] |
| Randomized trial | Sodium hypochlorite water (0.005%) | Forty patients took bath in the dilute bleach or placebo water for 10 min 2–3 times weekly for 4 weeks. | Both baths improved AD. Regular water bath was more effective in reducing the affected area and SCORAD | [49] |
| Randomized, controlled trial | Sodium hypochlorite water (0.005%) | Thirty-one patients, 6 months to 17 years of age, received orally administered cephalexin for 14 days and were assigned randomly to receive intranasal mupirocin ointment and sodium hypochlorite (bleach) baths (treatment arm) or intranasal petrolatum ointment treatment and plain water baths (controls) for 3 months. | ↓ SCORAD | [50] |
| Observational study | Sea water | Nine AD children took bath at beach twice daily for 6 days. | Remarkable improvements in the affected area, itching, redness, lichenification, and hydration | [51] |
| Observational study | Saline groundwater | Twenty-three subjects with mild-to-moderate AD took bath for 20 min once daily for 2 weeks. |
|
[52] |
| Case report | Water with salt | Twelve-year-old boy with severe AD took bath containing MgCl, MgSO4, NaCl, urea, and allantoin for 15–20 min twice daily for 3 days, followed by once daily for 10 days. Following each bathing, a mixture of fusidic acid 2%, betamethasone valerate 0.1%, fenticonazole 2% cream, and a moisturizer was applied to the affected area covered by bandages | ↓ SCORAD from 78 to 29.5 | [53] |
| Randomized, controlled trial | Water containing sodium hypochlorite (0.005%) | Patients were soaked in diluted bleach or distilled water baths for 10 min, twice weekly for 2 months. |
|
[54] |
| Observational study | Water containing sodium hypochlorite (0.005%) | Adult AD patients took two bleach baths (0.005% NaClO, 5–10 min) weekly for a total of 12 weeks. |
|
[55] |
| Observational study | Water with mild acidic cleanser | AD children took bath for 10–15 min once daily and topical emollient thrice daily for 14 days |
|
[56] |
| Observational study | Regular water | AD patients took bath with warm water for 20 min once or twice daily for 7 days, immediately followed by topical corticosteroid. Topical emollient was given after shower in the morning. After 7 days, topical corticosteroid was given once or twice weekly. | Improvements in adult and childhood AD were 87% and 96%, respectively. | [57] |
| Observational study | Regular water | AD patients took bath with warm water for 20 min twice daily for 3 days, immediately followed by topical corticosteroid. Afterward, topical corticosteroid was given twice daily without bathing for additional 11 days. |
|
[58] |
| Retrospective study | Calcium carbonate at various concentrations | Analyses the association of prevalence of eczematous dermatitis with bathing frequency in 1638 children. | OR for bathing < 46 min/week vs. > 80 min/week (OR = 0.49, 95% CI 0.35–0.69) | [59] |
| No significant effects | ||||
| Randomized, controlled trial | Regular water | AD children were treated with topical glucocorticoids immediately after bathing once daily for 14 days. Individuals without bathing served as controls | No differences in improvements of pruritus, EASI, and sleep scores between the two groups. | [60] |
| Negative effects | ||||
| Observational study | Unspecified | A questionnaire survey in 104 children with AD, 6 months and 18 years of age. | Bath duration positively correlated with the SCORAD (OR = 3.613, 95% CI: 1.676–7.788, p = 0.001) | [61] |
| Observational study | Water with different concentrations of CaCO3 | Cross-sectional study on 358 children aged 5–6 years | Hard water and longer exposure time to water before age of 2 years increased risk of eczema | [62] |
| Controlled trial | Regular water | AD children took 10-min bath, followed by either topical moisturizer or no topical moisturizer. Or children were given topical moisturizer alone. Skin hydration was measured up to 90 min after bathing. | A more dramatic increase in hydration in individuals treated with moisturizer alone compared to bathing plus moisturizer. | [63] |
| Self-controlled trial | Water containing oilatum | One arm of each AD child was soaked in water containing oilatum for 15 min once daily for 4 weeks. The unsoaked arm served as a control. Both arms were treated with topical moisturizer and corticosteroid twice daily. | AD clinical scores were significantly higher on the bathed arms than the unbathed arms. | [64] |
| Comparative study | Water with various hardness | Questionnaire was used to collect information of AD at various regions. Data from children and their parents were analyzed. | The hardness of domestic water was positively correlated with the prevalence of AD in primary school children (p = 0.02) | [65] |
- Note: (↑): significant increase; (↓): significant decrease; DNCB: 2,4-dinitrochlorobenzene; PSGA, patients’ self-global assessment scores; SCORAD, scoring atopic dermatitis index scores.
- Abbreviations: AD, atopic dermatitis; CDLQI, children’s dermatology life quality index; DFB, dermatophagoides farinae body extract; EASI, eczema area and severity index; GPx, glutathione peroxidase; IGA, investigator global assessment; MDA, malondialdehyde; MED, minimal erythema dose; ND, not determined; OR, odds ratio; PGI, patients’ global impression; ROS, reactive oxygen species; SC, stratum corneum; TCS, topical corticosteroids; TEWL, transepidermal water loss rate.
2.1. In murine Models of AD-Like Dermatitis
Murine models of chronic allergic contact dermatitis are commonly used in the study of AD [66, 67]. The beneficial effects of water bathing on AD have been demonstrated in murine models of hapten-induced chronic allergic contact dermatitis, i.e, AD-like dermatitis. Both 2,4-dinitrochlorobenzene (DNCB) and oxazolone are the common haptens used to induce AD-like dermatitis. In a murine model of DNCB-induced dermatitis, mice were bathed with spring water containing high concentration of minerals, mainly Mg2+, Ca2+, Na+, Cl−, SO42−, and Li, for 15 min daily while being topically treated with 0.5% DNCB every other day for 3 weeks [30]. The results showed that either high mineral water or 10% of high mineral water significantly decreased scratching frequency, with an efficacy comparable to the mice treated with topical 0.1% tacrolimus ointment. In parallel, serum levels of IgE and proinflammatory cytokines were significantly lower in mice bathed with high mineral water than in those bathed with distilled water. Moreover, high mineral water increased the activity of glutathione peroxidase while decreasing serum levels of reactive oxygen species and malondialdehyde. Similar results were observed in other studies using oxazolone-treated mice, showing decreased inflammatory infiltrates and lower expression levels of IL-33 mRNA in mice bathed with thermomineral water than those bathed with distilled water [32]. The effects of water on AD vary with mineral concentration [34]. This line of evidence indicates the beneficial effects of water bathing on AD in mice.
2.2. In Children With AD
The 1-year prevalence of AD in children can be as high as over 20% [68]. Because of the concern of adverse reactions, systemic treatment is not the favored option for childhood AD [69]. In comparison to adults, children are at a higher risk of cutaneous adverse reactions even for topical treatments [70]. Yet, studies have demonstrated that water bathing alone or in combination with topical emollient are safe and effective in the management of AD. A study in 867 AD children showed that 20-min bathing (spring water at 27.7°C) once or twice daily for a total of 12–24 baths significantly lowered SCORAD (p < 0.0001 vs. baseline) [38]. The efficacy was inversely correlated with age. Moreover, a higher percentage of patients who positively responded to water bathing was observed in those with onset age of AD under 2 years compared to those over 3 years old (56.6% vs. 28.0%). Twenty-minute bathing with spring water at 36–37°C once or twice daily exhibited a comparable efficacy to topical corticosteroids in terms of reductions in SCORAD, IGA, and pruritus [39, 41]. The disease relapsing rate and requirement of active treatments were significantly lower while disease-free time was significantly longer in the water bathing group than in the topical corticosteroid-treated group during a 4-month follow-up [41]. Bathing with 0.005% sodium hypochlorite reduced both topical corticosteroid (p < 0.05 vs. tap water) and topical antibiotic use (p < 0.05 vs. tap water) in within-group analysis [49]. A study in a small group of patients (N = 28) showed that bathing once daily and once weekly for 2 weeks were equally effective in reduction of SCORAD [43]. Children taking bath more than 80 min/week display a lower risk of eczema (OR = 0.49, 95% CI 0.35–0.69 vs. bathing < 36 min/week) [59]. Thus, water bathing can ameliorate and delay the relapse of AD in addition to reduction in medical treatment.
However, a randomized trial showed that reductions in either EASI or pruritus scores did not differ significantly between the topical applications of corticosteroids immediately after bathing and without bathing (84.8% vs. 81.4% for EASI; 77.8% vs. 75.8% for pruritus) [60]. Such controversial results were likely attributable to the use of potent corticosteroids, such as triamcinolone ointment, in the study. In such cases, the moderate effects of bathing on AD could not be observed.
Although most of the studies demonstrated a positive impact of water bathing on AD, several studies showed a negative influence on AD in children [60–65]. A study showed that bathing duration was positively correlated with the SCORAD (OR = 3.613, 95% CI: 1.676–7.788, p = 0.001) [61]. Moreover, exposure to water (swimming) increased the risk for eczema in children under age of 2 (adjusted OR = 1.67, 95% CI: 0.88–3.19) [62]. Particularly, bathing with water containing high concentration of calcium significantly increases risk of AD in infants (adjusted OR = 1.87; 95% CI:1.25–2.80; p = 0.002) [71]. The prevalence of AD in infants is positively associated with the domestic water hardness, with 5% increase in prevalence per 5° increase in water hardness [72]. In addition, swimming in hard water (CaCO3/L−1 > 150 mg/L) increased the risk of eczema (adjusted OR = 1.59, 95% CI: 0.69–3.64). Another study showed that the clinical scores were higher in children bathed once daily for 4 weeks than in those without being bathed (p = 0.019) [64]. Although the underlying mechanisms are unclear, these results clearly demonstrate that bathing can increase the risk and severity of AD at least in some cases.
2.3. In Adults With AD
AD can be onset in either early life (the first year) or adults, with 1-year prevalence of 4.9% (95% CI: 4.6%–5.2%) in adults [73]. Successful management of AD is still a challenge in clinic. However, evidence indicates that water bathing alone or in conjunction with other therapies benefits AD. For example, significant reductions in the transepidermal water loss rate (TEWL), skin roughness, and redness were observed in subjects who submerged their forearm in water solution, containing 5% dead sea salt, at 38°C–42°C for 15 min daily for 6 weeks, while immersion of the forearm in tap water did not change the TEWL significantly (p < 0.05) [36]. In addition, stratum corneum hydration levels were also increased by immersion of the forearm into the salted water (p < 0.05 vs. tap water). Moreover, water with additives is also effective for AD. Thirty-minute bathing with hydrogen water (H2 0.9 ppb/L) at 38°C–40°C daily for 8 weeks improved the nighttime itching score by over 60% [48]. Similarly, bathing with water containing 0.005% sodium hypochlorite twice weekly for 2 months significantly decreased EASI and pruritus scores, while neither the EASI nor pruritus score was remarkedly altered, following bathing with distilled water for 2 months [54]. Similarly, bathing with 0.005% sodium hypochlorite improved multiple AD-associated abnormalities, including the EASI, pruritus, TEWL, and stratum corneum hydration [55]. However, a meta-analysis showed a comparable efficacy between water containing sodium hypochlorite and regular water for AD [74]. Furthermore, applications of corticosteroid immediately after bath can rapidly improve AD and reduce the use of corticosteroid in the maintenance phase in both adults and children [57]. Bathing followed by topical corticosteroid twice daily for 2 days lowers the IGA score by 50%, the patient self-assessment score from 3 to 1.71, and the pruritus score from 2.71 to 0.86 [58].
Additionally, the beneficial effects of herbal bath on AD are also well-documented. For example, bath with pine tar for 4 weeks significantly improves multiple parameters of AD, including patient-oriented eczema measure, children dermatology life quality index, and pediatric allergic disease quality of life questionnaire along with over 20% reduction in objective SCORAD, in children [75]. Similarly, herbal bath together with oral herbal medicine mitigates AD in both children and adults who poorly respond to steroids [76, 77]. A meta-analysis of 8 studies showed that herbal bath decreases both AD severity (mean standard deviation = −0.77, 95% CI: 0.99–0.55, p < 0.0001) and recurrence rate (relative risk ratio = 0.25, 95% CI: 0.1–0.59, p = 0.0002). The commonly used herbal ingredients in herbal bath are those that exhibit anti-inflammatory, immune regulatory, anti-itching, and antiallergy properties [78]. Collectively, this line of evidence indicates that water bathing alone or in conjunction with other medications is effective for AD.
3. The Underlying Mechanisms by Which Water Bathing Benefits AD
Although studies demonstrate beneficial effects of water bathing on AD, the underlying mechanisms remain unclear. However, a line of evidence points to several possible mechanisms contributing to the improvement of AD by water bathing, including inhibition of cytokine expression and Langerhans cell function, antimicrobe, and improvements in the epidermal permeability barrier and stratum corneum hydration.
3.1. Improvements in the Epidermal Permeability Barrier and Stratum Corneum Hydration
Epidermal function is linked to the pathogenesis of AD. The compromised epidermal permeability barrier increases the risk of AD [79, 80], while reduced stratum corneum hydration levels can provoke cutaneous inflammation [81, 82]. Conversely, improvements in the epidermal permeability barrier and stratum corneum hydration ameliorate AD [83]. Evidence suggests that the beneficial effects of water bathing on AD can be ascribed to the improvements in epidermal function. In a murine model of AD, immersion of mice in mineral water at 37°C–39°C daily for 2 weeks induced a more remarkable reduction in the TEWL than distilled water (p < 0.05 vs. distilled water) [31]. In AD patients, submersion of the forearm into water containing 5% deep sea salt (high magnesium content), but not into tap water, at 38°C–42°C daily for 6 weeks lowered the TEWL by 19%, while increasing stratum corneum hydration levels by 14% [36]. Bathing with hydrogen water 30 min once daily for 4 weeks significantly lowered the TEWL (p < 0.05), with a further reduction at 8 weeks (p < 0.001), whereas the TEWL was increased over the 8 weeks on the unmerged body site [48]. Once-daily 20-min bath with underground water saline solution for 2 weeks decreased the TEWL from 18.80 ± 8.21 at baseline to 11.35 ± 4.33 (p < 0.01), while increasing stratum corneum hydration levels from 24.72 ± 16.47 at baseline to 42.67 ± 7.66 (p < 0.0001) [52]. Similarly, taking bleach baths (0.005% NaClO; 5–10 min duration) twice weekly for a total of 12 weeks significantly decreased the TEWL, while increasing stratum corneum integrity [55]. Taking together, this evidence suggests that the benefits of water bathing in AD can be attributable to the improvements in epidermal functions.
3.2. Anti-Inflammation
AD is an inflammatory dermatosis. Anti-inflammatory agents, including calcitriol, glucocorticoids, and biologics, have been widely employed in the treatment of AD, whereas several studies also demonstrate the anti-inflammatory effects of water bathing on AD in both the murine model and humans. For example, bathing with high concentration mineral spring water 15 min daily for 4 weeks significantly lowered serum levels of IgE, IL-1β, IL-13, and TNF-α in a murine model of AD [30]. Moreover, bathing in mineral water, but not in distilled water, decreased the infiltration of CD1+ cells in the skin and Treg cells in the spleen of mice with AD-like dermatitis in addition to down-regulation of the CD4+/CD8+ cell ratio in spleen lymphocytes [31, 32]. Cytokines, especially IL-4 and IL-10 which are important for Th2 cell development, were also reduced by bathing with mineral water. Furthermore, topical applications of deep-sea water lowered serum levels of IgE, histamine, TNF-α, IL-1β, and IL-6 in a murine model of AD-like dermatitis [84, 85]. In vitro, spring water decreases the production of IL-12, IL-23, IFN-γ, and IL-17 in dendritic cell culture [86]. Both calcium and magnesium are major components in natural water/spring water. Previous studies demonstrated that calcium inhibits histamine release by mast cells, while magnesium inhibits alloantigen-presenting function of Langerhans cells in vitro [87, 88]. Thus, water bathing-induced improvement in AD can be due to inhibition of inflammation. However, all these studies were carried out in murine models of AD-like dermatitis and in vitro. Further studies are needed to determine whether water bathing inhibits inflammation in AD patients.
3.3. Antioxidative Stress
Patients with AD exhibit increased oxidative stress in comparison to the controls [89]. Oxidative stress can provoke and/or exacerbate inflammation [90]. Conversely, antioxidants can ameliorate inflammation, including AD [91, 92]. Several studies showed antioxidant benefits of water bathing. For instance, bathing with spring water for 4 weeks decreased serum levels of reactive oxygen species and malondialdehyde (p < 0.05 vs. distilled water), with a comparable efficacy of 0.1% tacrolimus in a murine model of AD-like dermatitis [30]. In parallel, the activity of serum glutathione peroxidase was markedly increased. Similarly, bathing mice with sea water significantly decreased cutaneous malondialdehyde levels while increasing glutathione content by over 50% compared to the unbathed controls [33, 34]. Bathing mice with hydrogen-rich water also decreases serum malondialdehyde levels (p < 0.05 vs. distilled water) [93], possibly in part due to the H2-induced reduction in hydroxyl radical [94]. Additionally, both proline and methionine are nonenzymatic antioxidants [94, 96]. Bathing pigs with spring water at 40°C increased plasma levels of both proline and methionine as compared to tap water [29]. Finally, the antioxidant property of spring has also been demonstrated in vitro, evidenced by reductions in levels of reactive oxygen species in fibroblast cultures [97]. Hence, the antioxidant effect of water bathing can contribute to the improvement of AD.
3.4. Antimicrobial
Dysbiosis of skin microbiota has been well demonstrated in AD, evidenced by the observations that early life exposure to antibiotics increases risk of AD and that the skin microbial diversity is reduced in patients with AD [98, 99]. Previous studies have shown that the Shannon diversity index of microbial communities in the AD-involved sites is negatively correlated with the EASI and that the density of Staphylococcus aureus is positively correlated with the EASI. In comparison to topical corticosteroids alone, treatments with topical corticosteroids plus water bathing induce a more dramatic increase in microbial diversity, along with a reduction in the density of Staphylococcus aureus comparable to normal skin [100]. Similarly, 28% of children with AD exhibited reduced Staphylococcus aureus colonization/infection following water bathing [49]. Similar results were observed in patients with moderate-to-severe AD, in which 1-month water bathing reduced Staphylococcus aureus density by 41.9%, with a further reduction of 53% at 2 months [54]. In addition, the washing body with 0.006% sodium hypochlorite once daily for 2 weeks markedly decreased Staphylococcus aureus infection from 86% at baseline to 50% (p = 0.0002) [19]. However, another study by the same group showed that taking baths with 0.005% sodium hypochlorite twice weekly did not significantly affect Staphylococcus aureus infection and the Shannon diversity index [55]. This discrepancy could be due to a lesser frequency of bathing in the latter study (once daily vs. twice weekly). Nonetheless, this bulk of evidence indicates that the beneficial effects of water bathing on AD are in part attributed to the antimicrobial effect.
4. Unsolved Puzzles
Although numerous studies have demonstrated the benefits of water bathing in AD, there are still unsolved puzzles. While study showed that living in a hard water (range: 76 to > 350 mg/L CaCO3) area is positively associated with the incidence of AD in children, domestic water softeners do not improve AD severity [101]. Moreover, combination of infant swimming and exposure to domestic hard water did not increase the prevalence of eczema compared to those exposed to hard water bath alone [62]. This evidence suggests that other factors rather than water hardness alone affect AD. It is important to note that exposure to hard water increases risk of AD only in children with filaggrin mutation (adjusted HR 2·72, 95% CI 2·03-3·66) [102]. Thus, the genetic background should be considered when determining the link between AD and exposure to water.
In addition, drinking hydrogen-water improved cutaneous inflammation in mouse models of AD-like dermatitis [103–105]. Similarly, intake of underground water for 8 weeks improves disease severity, TEWL, and pruritus in NC/Tnd mice [106]. Likewise, drinking deep sea water for 6 months improved clinical symptoms, accompanied by decrease in potassium, mercury, and lead, and increases in selenium in the hair of patients with AD [107]. Furthermore, drinking deep sea water lowered serum levels of IL-4, IL-13, IL-18, and antimite IgE. In parallel, AD severity was improved by 56% [108]. On contrary, drinking distilled water did not change either serum cytokine levels or mineral content in the hair. Thus, it is likely that the minerals in the drinking water can be delivered to the skin where minerals regulate cutaneous function. Consistent with this assumption, a previous study showed that the levels of several minerals (magnesium, calcium, and zinc), which negatively correlated with AD severity, were significantly decreased in the hair of patients with AD [109]. Oral supplement of zinc improves AD and increases zinc content in the hair [110]. Interestingly, intake of 2 litters of oligo-mineral water, but not medium-mineral water, daily for 1 month changes lipid content (58 increased and 8 decreased) in the stratum corneum of normal humans [111]. This line of evidence suggests that the effects of water bath on AD is not entirely due to the directly increased hydration of the stratum corneum rather due to the upregulation of epidermal lipid content. However, additional studies are required to delineate the interactions between water, including which components in the water, and biological function in the pathogenesis of AD. The beneficial effects of drinking water on AD also need to be validated in large cohort.
Another perplexity is whether the frequency of bathing affects AD. A study showed exacerbation of AD in individuals who took bath more than once daily compared to once daily [112]. In contrast, some studies showed benefits of once-daily bathing for AD. However, a meta-analysis did not show differences in therapeutic outcome in individuals having bath ≥ 1 vs. < 1 time daily [112]. Another study showed no significant difference in the efficacy of topical corticosteroids for AD when applying to prehydrated vs. to dry skin [60]. The underlying mechanisms whereby the frequency of water bathing or prehydration of the skin does not affect the outcome of AD are unknown. But overhydration of stratum corneum can negatively impact cutaneous function. For example, overhydration of the stratum corneum can disrupt the epidermal permeability barrier, facilitating the transcutaneous penetration of both topical medication and harmful substances (such as irritants and allergens) [114–117]. The latter can induce cutaneous inflammation. Correspondingly, wet work or frequent washing increases the risk of contact dermatitis [118]. A recent study demonstrated that bathing with hard water (high concentration of minerals) increased risk of dry skin (OR = 1.22; 95% CI: 1.03–1.45) [119]. Hence, the optimal frequency and duration time of bathing, which possibly vary with water hardness, remain to be determined.
5. Summary
Water bathing can improve AD via anti-inflammatory, antioxidant, and antimicrobial effects, as well as by improving epidermal function. The effects of water bathing on AD vary with water hardness and possibly water temperature and pH. However, constituents, optimal frequency, and duration of bathing benefit for AD remain to be determined.
Disclosure
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
All authors made a significant contribution to the work, whether that was in the conception, acquisition of data, and analysis; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. Dongyun Lei, Jiechen Zhang, and Bijun Xia contributed equally to this work.
Funding
The study was partially supported by Tianjin Health Commission Science and Technology (TJWJ2022QN088) and the Research Fund of Shanghai Tongren Hospital, Shanghai Jiaotong University School of Medicine.
Open Research
Data Availability Statement
The authors have nothing to report.




