Erbium-YAG Laser Treatment for Recalcitrant Warts: A Retrospective Analysis
Abstract
Background: Viral warts are the result of keratinocyte infection caused by the human papillomavirus (HPV), usually represent as benign growths of epithelial tissue. Those afflicted often experience a notable decline in their quality of life due to these lesions, which can also lead to functional issues and physical discomfort. Laser technology has introduced novel approaches in treating viral warts, especially ablative lasers such as CO2 and Erbium-YAG (Er:YAG) lasers. Er:YAG laser gained recognition as a safe and effective method for addressing viral warts. Nevertheless, different recurrence rates have been reported in medical literature following treatment using Er:YAG laser, ranging from 24% to 71%. This study aimed to evaluate the recurrence rate and the risk factors that might affect it following successful treatment of warts using an Er:YAG laser.
Methods: A retrospective chart review analysis of all 245 patients who underwent an Er:YAG laser wart removal between January 2019 and July 2023 was conducted. The main outcomes measures were response rate and number of sessions required to get complete clearance.
Results: There was an overall complete resolution rate of 71.6% at 12 months follow-up. Four parameters were found to affect the response rate: the number of sessions until complete response, duration of the wart present before the laser treatment, smoking, and periungual wart location.
Conclusion: Er:YAG laser is an effective method for treating recalcitrant warts, and different risk factors were proven to effect its efficacy.
1. Introduction
Viral warts are the result of keratinocyte infection caused by the human papillomavirus (HPV) [1], usually represent as benign growths of epithelial tissue, ranging from 1 to 20 mm in diameter [2]. HPV encompasses a diverse collection of around 120 genotypes that invade the skin or mucous membranes [3]. Warts are a prevalent concern in dermatology, affecting both children and adults at an estimated rate of 5%–20%. The highest frequency of occurrence is noted during the teenage years [4, 5]. Those afflicted often experience a notable decline in their quality of life due to these lesions, which can also lead to functional issues and physical discomfort, particularly when they manifest on the palms of the hands or soles of the feet [6]. Consequently, cutaneous warts stand as one of the most commonly addressed conditions in clinical dermatology [7].
While warts might eventually vanish on their own as the immune system finds a way to eradicate the virus, the duration of this process is unpredictable and can span from months to years [8]. Many of the techniques employed today come with associated drawbacks and potential side effects. The application of topical treatments necessitates extended drug usage, making treatment success heavily reliant on the patient’s adherence [9, 10]. Surgical approaches have demonstrated moderate effectiveness, but they come with downsides such as pain, extended healing times, and the possibility of yielding incomplete and surface-level outcomes, consequently resulting in elevated rates of recurrence [9].
Laser technology has introduced novel approaches utilizing energy-based devices in the treatment of warts [2]. In our recent study, we introduced a new effective protocol for treating warts using a combination of Er:YAG laser and LP Nd:YAG laser [11]. The Er:YAG laser, similar to the CO2 laser, falls into the category of ablative lasers. Operating at a wavelength of 2940 nm, this laser is strongly absorbed by water. It has gained recognition as a secure method for addressing viral warts. Nevertheless, a considerable proportion of patients, particularly those afflicted with plantar warts, may experience a notable recurrence rate, necessitating supplementary interventions [12]. Various relapse rates were described after treatment with Er:YAG laser, ranging from 24% to 71% [11, 12]. This retrospective study aimed to evaluate the recurrence rate and the risk factors that might affect it after successful treatment of warts using Er:YAG laser.
2. Materials and Methods
2.1. Patients and Equipment
We performed a retrospective study analysis on computerized documents of patients treated for the first time with Er:YAG laser between January 2019 and July 2023. Exclusion criteria included previous laser treatments for warts and pregnancy. The study was conducted following the approval of the Helsinki ethical committee at Rambam Health Care Campus (approval no. RMB-D-0162-22).
Treatments were conducted using the Harmony XL Pro (Alma Lasers, Caesarea, Israel) platform, which utilizes a 2940 nm Er:YAG laser (iPixel Pro 2940 module). The Er:YAG laser parameters used were spot size of 1 or 4 mm, frequency of 2 Hz, fluence ranging between 700 and 2500 mJ/pulse, and a pulse duration of 1 or 2 msec. The treatment endpoint was fulgurating the verruca and 1 mm from the surrounding normal skin. Eutectic mixture of local anesthetics (EMLA) was applied, and intralesional injection of lidocaine was injected in each wart lesion prior to the procedure to avoid pain or discomfort during the procedure. All lesions were treated by the same physician.
Treatment sessions were scheduled every 2 months and were carried on until the complete clearance of warts. Some patients did not keep up with exactly 2 months treatment interval and had longer periods between the sessions. The cessation of the treatment was determined based on the complete clearance of warts, which was defined as the absence of visible and palpable lesions 2 months after the last treatment session. All patients were assessed whether they have achieved complete response or not after 12 months.
The characteristics that collected of each patient included number of sessions until complete response, age, gender, ethnicity, wart’s location, metabolic disease history, immunological status, smoking status, and duration warts were present before laser treatment, history of previous treatment for warts, number of warts that received therapy, and number of treatment sessions needed until complete response.
2.2. Statistical Analysis
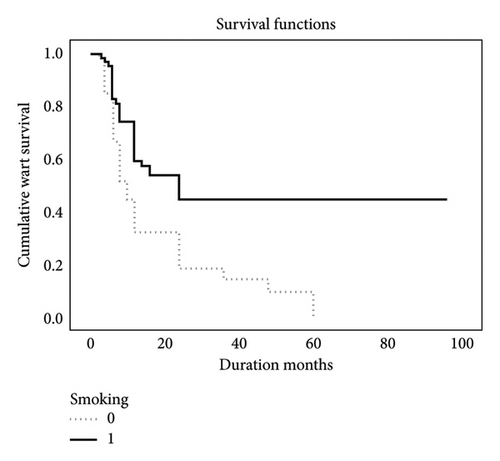
Descriptive statistics in terms of mean, standard deviation, median, and percentage were calculated for all the characteristics collected in the study. Normal distribution of the continues parameters was tested by Kolmogorov–Smirnov test. Logistic regression mode with odds ratio and 95% confidence interval was applied to predict the independent parameters that influence CR. Kaplan–Meier model was used to test the time duration to achieve CR according to smoking habits, and p < 0.05 was considered significant. SPSS version 28 was used to statistical analysis.
3. Results
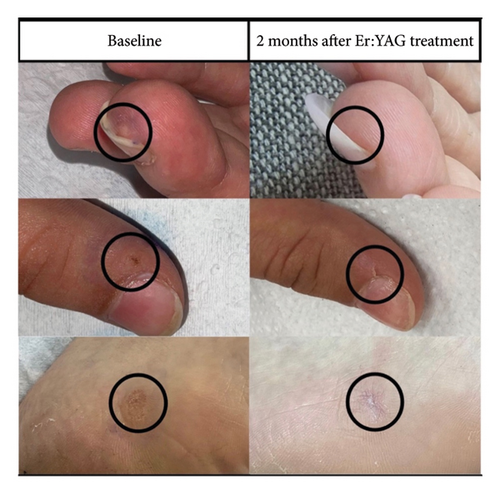
Between January 2019 and July 2023, 245 patients were treated for the first time with an Er:YAG laser for viral verruca, and out of them, 201 patients had their complete data collected and completed follow up. Cohort was age 6–80 years old, with a mean age of 33.7. The average duration and the median duration of the viral warts prior to treatment exceeded 1 year. All warts were symptomatic, causing varying degrees of pain and discomfort. The average number of warts per patient was 7.2 (range 1–23). There was an overall success rate (i.e., complete resolution of all warts treated) of 71.6% at 12 months follow-up. Table 1 provides detailed patient characteristics, and the complete response rate was achieved for each characteristic. It highlights that only three parameters were found to be statistically significant and influenced the response rate: the number of sessions at 12 months follow-up, the duration of the wart present before the laser treatment, and smoking status. Table 2 presents the response rates according to the different locations of the warts, and periungual wart location was the only location with statistical significance affecting the response type. Photomicrographic documentations of warts before and after first treatment session are presented in Figure 1.
| Not CR; N = 57 | CR; N = 144 | p | |
|---|---|---|---|
| Age | 34.6 ± 17.2 | 32.9 ± 16.8 | p = 0.55 |
| Gender | p = 0.41 | ||
| Male | 26 (46%) | 75 (52%) | |
| Female | 31 (54%) | 69 (48%) | |
| Ethnicity | p = 0.29 | ||
| Jew | 30 (53%) | 64 (44%) | |
| Not jew | 27 (47%) | 80 (56%) | |
| Mean of the number of sessions at 12 months | 4.0 ± 1.2 | 3.21 ± 1.16 | p < 0.001 |
| Duration months when wart was present before laser treatment | 24.8 ± 16.6 | 11.44 ± 9.4 | p < 0.001 |
| Number of warts treated | 8.04 ± 3.6 | 7.62 ± 4.6 | p = 0.54 |
| Smoking | 34 (60%) | 32 (22%) | p < 0.001 |
| Immunosuppressed | 3 (5.3%) | 1/(0.7%) | p = 0.071 |
| Other disease | 19 (33%) | 41/142 (29%) | p = 0.54 |
| Metabolic disease BMI MORE 28 | 8 (14%) | (11%) | p = 0.59 |
| Previous treatment | p = 1.00 | ||
| Cryotherapy | 57 (100%) | 142 (98.6%) | p = 0.26 |
| Topical | 44 (77%) | 121 (84%) |
- Note: Mean of the number of sessions at 12 m = 0.000047. Duration months when wart was present before laser treatment = 0.000000000011. Smoking = 0.00000041.
| Location | Not CR; N = 57 | CR; N = 144 | p |
|---|---|---|---|
| Palmar | 19 (33%) | 45 (31%) | p = 0.78 |
| Plantar | 19 (33%) | 67 (46.5%) | p = 0.88 |
| Both palmar and plantar | 5 (8.8%) | 7 (4.9%) | p = 0.33 |
| Periungual | 20 (35%) | 7 (4.9%) | p < 0.001 |
| Others location | 23 (40%) | 50 (35%) | p = 0.52 |
- Note: Periungual = 0.000000014.
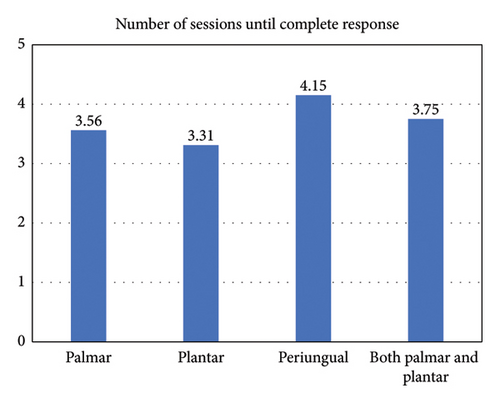
Different response rates for each wart location are demonstrated in Table 2, if we look at the periungual location, for example, we can see that only 4.9% of the patients who achieved complete response had periungual lesions, while 35% of the patients who did not achieve it had periungual lesions. This difference was statistically significant, and it indicates that periungual location significantly reduces the likelihood of a complete response, with a p-value of 0.005 in multivariate analysis and p-value < 0.001 in univariate analysis. Figure 2 also presents the mean number of sessions required for different wart locations.
For better understanding of the results, we made Figure 3 in which we divided all of the 201 patients into 6 groups according to the number of sessions every patient took until the 12 months checkpoint. Each column is divided into two colors to represent the portion of CR and non-CR at every session group. For example, 6 patients completed only one session during the 12 months, one of them (17%) had no complete response, and 5 of them (83%) had complete response.
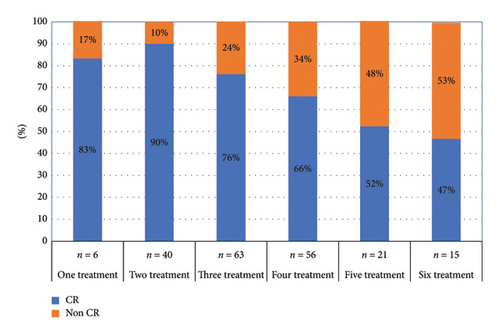
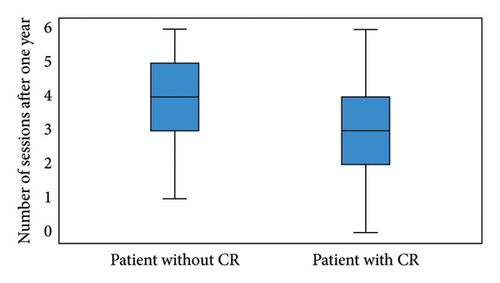
Figure 4 reveals a higher median number of treatment sessions in the group that did not achieve a complete response. The results also demonstrate the impact of smoking on treatment response, Figure 5 presents the duration required for achieving a complete response in both smokers and in nonsmokers. The median time until complete response in nonsmokers was 10 months, significantly shorter than the 24 months observed in smokers.
4. Discussion
Viral warts are frequently occurring benign growths of the skin that pose challenges in terms of treatment. Employing topical treatments necessitates extended drug application durations, and the effectiveness of the treatment relies heavily on patient compliance [9, 10]. Treatment methods involving physical removal, such as surgical excision, electrodesiccation, and cryosurgery, yield varying success rates and may result in incomplete and superficial outcomes, consequently leading to elevated recurrence rates [9].
In recent years, there has been an increased focus on laser therapy as an alternative. Ablative lasers such as Er:YAG and CO2 lasers, as well as nonablative lasers, such as the long-pulsed Nd:YAG and pulsed dye lasers (PDLs), have been in use for treating recalcitrant viral warts. The CO2 laser was the pioneer in this field [13], emitting high-energy laser light that effectively removes most of the wart, coagulates blood vessels, and induces wart necrosis [14]. A review of previous studies has shown success rates for CO2 lasers in treating stubborn warts ranging from 46.2% to 100% [1]. Yet, it is important to mention that approximately 60% of cases treated with this laser may experience scarring and pain [15–18].
Subsequently, the Er:YAG laser gained popularity, as it’s wavelength is primarily absorbed by water, and it is of limited penetration depth of just a few micrometers. Coupled with high power of short light pulses, it allows for precise ablation and cutting of soft tissue, similar to the function of conventional scalpels [19]. In one study, Wollina, Konrad, and Karamfilov [12] reported a clearance rate of 72.5% in 69 patients with warts after a single treatment session with the Er:YAG laser. The Er:YAG laser’s capability to achieve higher clearance rates while causing less damage to nearby healthy epidermal cells leads to reduced scarring and fewer pigmentary changes [12, 20].
To date, most of the studies in the literature regarding ablative lasers have primarily focused on the use of CO2 lasers, with significantly less attention given to the Er:YAG laser. In our study, we chose to investigate the application of the Er:YAG laser over the CO2 laser, as it is the newer technology with fewer associated side effects. The results revealed 71.6% overall complete response (complete resolution of the warts) at 12-month follow-up period following the utilization of the Er:YAG laser.
The results indicated an inverse relationship between the number of treatment sessions and the complete response rate among patients, suggesting that individuals who did not achieve a complete response in the early sessions may encounter challenges in achieving it later. Notably, this finding did not attain statistical significance when multivariate analysis was applied. Our interpretation of this is that the multivariate test accounts for the influence of other variables, focusing solely on the parameter being tested, which in this case is the number of sessions until complete response.
A significant characteristic to predetermine the outcome is the wart’s location. The findings demonstrated that periungual wart locations, whether on the hands or feet, significantly reduced the likelihood of achieving a complete response. This discovery underscores the complexity and resistance often associated with warts in these locations. Healthcare providers should take this into consideration when designing treatment plans, as periungual warts may necessitate more intensive or specialized approaches to achieve successful outcomes, such approaches may involve laser combination treatment as we discussed in our previous study, in which we proved that the combination of Er:YAG and Nd:YAG lasers in treating recalcitrant warts is more effective than sole treatment with Er:YAG only [11]. The discovery mentioned above also emphasizes the importance of patient education and preventive measures to minimize the development of warts in such challenging areas.
Another noteworthy finding was the significant difference in the time required to achieve complete response in wart treatment between nonsmokers and smokers. The median duration for nonsmokers was 10 months, significantly shorter than the 24 months observed in smokers. This discovery suggests that smoking may adversely affect the effectiveness of wart treatment, potentially delaying the healing process. It underscores the importance of taking lifestyle factors, such as smoking, into account when evaluating treatment outcomes and highlights the potential benefits of smoking cessation in enhancing the response to wart treatments.
Researchers and healthcare professionals should conduct further investigations into the efficacy of laser treatments, taking into account factors such as treatment intensity, patient tolerance, and treatment suitability. This understanding can lead to more refined treatment strategies and improved patient outcomes in the future.
In conclusion, the Er:YAG laser proves to be an effective method for treating recalcitrant warts. Optimal results are achieved in nonsmoker patients and for those with nonperiungual wart locations, while patients who do not achieve a complete response during the early sessions may encounter challenges in subsequent sessions and should take into consideration more intensive or specialized approaches.
Ethics Statement
The study was conducted following the approval of the local ethical committee, the Helsinki Committee, which is recognized by the FDA and the EMEA.
Disclosure
The research was conducted in Rambam Health Care Campus, Haifa, Israel.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
The authors did not receive any financial support.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




