The Changing Incidence of Malaria in Indonesia: A 9-Year Analysis of Surveillance Data
Abstract
Objectives: This study aims to track the spatiotemporal incidence rate and endemicity of malaria in 34 provinces of Indonesia from 2014 to 2022 using surveillance data, commenting on trends observed and deriving implications for public health practice for combating malaria in Indonesia.
Methods: This paper is a longitudinal study using routinely collected public health surveillance data. We calculated the incidence rate as both total cases and the number of cases per 1000 person-years at the provincial level. The endemicity was mapped as the annual parasite index (API) per 1000 at-risk populations. Trends in malaria incidence rate and endemicity were examined descriptively in Excel Version 16.83.
Results: Nationally, malaria incidence increased by 191,503 from 2014 to 2022. The API at the national level rose by 62.63% from 0.99 cases per 1000 at-risk populations in 2014 to 1.61 in 2022. Despite the national increase, the endemicity of Sumatra Island and Kalimantan showed strong progress (API less than 1 per 1000 at-risk population). The incidence and endemicity of malaria remain high in the Eastern Islands, particularly in the provinces of Papua and West Papua. The Eastern Islands accounted for 95.73% (424,569 cases of total cases 443,530) of national cases in 2022.
Conclusions: Progress has been made in province-level malaria elimination, especially outside Papua and West Papua. To prevent the persistence of endemic malaria pockets in Papua and West Papua, there is a need for greater coordination of and further dedication of financial resources toward efforts to eliminate malaria in these provinces. These efforts should be supported by an improvement in surveillance capacity, the inclusion of information on the parasite species responsible for malaria cases in routine surveillance initiatives, and the use of culturally tailored interventions to maximize health-seeking behaviors and intervention uptake.
1. Introduction
Among the preventable and curable vector-borne diseases, malaria remains one of the greatest public health threats. Globally, it was estimated that there were 247 million cases of malaria in 2021, an increase from 245 million in 2020 [1]. In 2021, there were an estimated 619,000 deaths from malaria, of which 76% were in children under 5 years. Although the global incidence of malaria declined from 72 to 57.2 cases per 1000 population at risk between 2010 and 2019, the incidence increased by 4% to 59.4 in 2020. Then, from 2020 to 2021, there was no change in malaria incidence. The trend shows that the effort to manage malaria can prevent the worst-case scenario that was initially projected at the start of the pandemic1.
The WHO South-East Asia region accounted for 2% of global cases (5.4 million) in 2021, and the number of cases fell to 77.5% between 2010 and 2021 [1]. Within Indonesia, more than half of the districts had been certified as malaria-free by 2021, and the annual parasite index (API) (a number showing confirmed cases per 1000 population/API) was maintained at <1 per 1000 population from 2018 to 2020. However, the API increased to 1.1 per 1000 population in 2021 [2]. In 2021, the Indonesian Ministry of Health (MoH) recorded 304,607 malaria cases nationally [3].
The Government of Indonesia, via the MoH, aims to eliminate malaria by 2030, aligning with the WHO malaria elimination target at 2030 [4]. Nationally, major progress has been made toward this target—in 2018, the number of confirmed malaria cases fell by 50% from the previous year [4]. By that year, 72% of Indonesia’s 265 million inhabitants lived in malaria-free regions [4]. Since 2004, the MoH has scaled-up malaria programs considerably using an integrative approach to combating the illness, introducing artemisinin combination therapy (ACT) as a first-line malaria treatment, controlling drug procurement and distribution, enhancing prevention through outreach to remote areas to distribute bed nets, and strengthening surveillance systems. The capacity and technical quality of malaria testing have also benefited from the introduction and increased use of rapid diagnostic tests (RDTs).
Malaria studies in Indonesia have generally taken the form of case studies describing the epidemiology of malaria in endemic areas, as well as serological and clinical studies in selected geographical locales [5–10]. Although recent publications have addressed spatiotemporal patterns of malaria in the Menoreh Hills in Java [11], there has been a lack of literature concerning trends in malaria incidence over time at the national level. This study aims to fill the identified literature gap using nationwide malaria surveillance data. It aims to describe the patterns of malaria incidence and API in Indonesia from 2014 to 2022, with the aim of informing the use of preventative measures and malaria treatment.
Our study aims to answer the question: what have been the national-level and provincial-level trends in the incidence and endemicity of malaria in Indonesia from 2014 to 2022? and what implications do these trends carry for public health policy?
2. Methods
2.1. Data
This paper is a retrospective longitudinal study using routinely collected public health surveillance data. Data on the API and the number of malaria cases were obtained directly from the Sub-Directorate of Malaria under the Directorate of Vector-Borne Diseases and Zoonoses at the Indonesian MoH, covering the period between January 2014 and December 2022. Provincial population data were drawn from the 2014 to 2022 population census and projection [12].
The API data at the national and provincial levels were freely accessible from the Indonesia Annual Health Report [13]. However, data concerning the API at the district/city level was not freely accessible, and to use these, the authors obtained permission from the MoH. Our sample consisted of 306 data points—one data point for each of the 34 provinces included in the study and for each of the 9 years covered. Surveillance data were available from 2014 and thus, the latest data used were from 2022.
The reporting mechanism and variables used in this study were in accordance with the MoH 2007 guideline on malaria surveillance [14]. Data were reported at the village level and were collected from government-mandated community health centers (“puskesmas”). Cases were reported by clinicians and recorded by health care workers at the village level, who passed the data on to district/city level officials for aggregation. Included cases were categorized as “clinical diagnosis,” “suspected malaria,” or “confirmed malaria case.” Cases were categorized into the former two groups based on the individual’s presentation upon examination by a clinician and into the latter group after laboratory diagnosis. Laboratory diagnosis involved either a microscopic examination of blood samples or the use of an RDT. All three categories were included in our study.
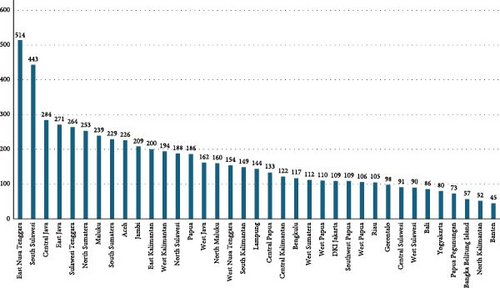
There are a total of 6201 laboratories in Indonesia that can carry out malaria testing and are distributed across 38 provinces. East Nusa Tenggara has the highest number of healthcare facilities with malaria laboratory testing (514), followed by South Sulawesi (443), Central Java (284), and East Java (271). A list of laboratory capacity across 38 provinces can be accessed from Appendix 1.
Additional sources from the authors’ knowledge and an unstructured search of databases, such as PubMed, Scopus, Web of Science, and Google Scholar, were included based on their judged relevance to the paper. The inclusion criteria were recent (within the last 10 years), relevant to malaria in Indonesia, published in an academic journal, and written in English or Indonesian.
2.2. Study Site
This study uses province-level data from the 34 provinces of Indonesia for which data were available from the MoH. These provinces can be further classified by island: Sumatra (including the provinces of Nanggroe Aceh Darussalam, North Sumatra, West Sumatra, the Riau Islands, Jambi, South Sumatra, Bangka Belitung, Bengkulu, and Lampung), Java (including the provinces of DKI Jakarta, West Java, East Java, Central Java, DI Yogyakarta, and Banten), Kalimantan (including the provinces of West Kalimantan, Central Kalimantan, South Kalimantan, East Kalimantan, and North Kalimantan), Sulawesi (including the provinces of Gorontalo, North Sulawesi, Central Sulawesi, Southeast Sulawesi, West Sulawesi, and South Sulawesi) and the Eastern Islands (including the provinces of Bali, West Nusa Tenggara, East Nusa Tenggara, Maluku, North Maluku, West Papua, and Papua). Indonesia is a tropical country where the sun shines all year, with an average of 28°C on the coast and 23°C on the higher landscape. Climatically, Indonesia is mostly hot and humid.
2.3. Analysis
We conducted a descriptive analysis of the incidence of malaria and spatiotemporal API in 34 provinces in Indonesia, categorized by island (Sumatra, Java, Kalimantan, Sulawesi, and Eastern Islands). Trends in the malaria incidence rate and endemicity were examined descriptively in Excel Version 16.83. Malaria morbidity accounted as the incidence rate was calculated as the number of cases divided by its population times 1000 at the provincial level. The endemicity level was mapped using the API per 1000 population at risk. The map was generated by mapchart.net.
3. Results
We found that malaria incidence considerably increased in the last 5 years of the study, rising from 222,085 cases nationally in 2018 to 443,530 cases in 2022 (Figure 1). Of these 443,530 cases, 393,801 were in Papua (88.79%), 15,812 were in East Nusa Tenggara (3.57%), and 13,080 were in West Papua (2.95%). The overwhelming majority of cases occurred in the Eastern Islands, with 424,569 cases (95.73% of national cases) occurring in 2022. However, comparing the percentage of cases in each province per total case showed a decrease in proportion in almost all provinces except Papua.
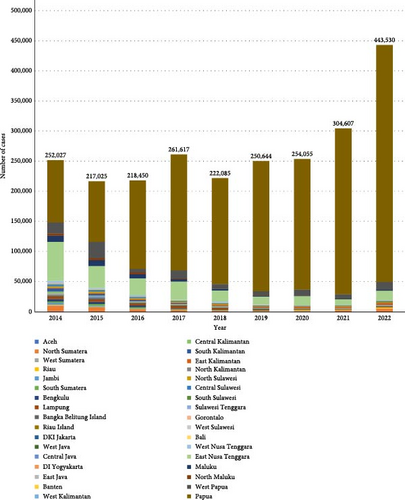
The API at the national level increased from 0.99 cases per 1000 at-risk populations in 2014 to 1.61 in 2022, with the highest annual rise observed in 2022. Figure 1 depicts the national annual caseload, separated by province.
Nationally, over the 9 years of the study period, the number of malaria cases fluctuated. The lowest incidence was found in 2015, with 217,025, and the highest incidence was in 2022, with 443,530 cases. Then, it was recorded that, nationally, malaria cases rose by 45.61% or 138,923 cases in 2022 compared to 2021. The number was 304,607 in 2021 to 443,530 in 2022. Over the 9 years, the province with the highest number of cumulative cases by far was Papua (1,821,908 total cases), followed by East Nusa Tenggara (231,403) and West Papua (111,045). In 2022, these three provinces, respectively, accounted for 88.79%, 3.57%, and 2.95% of national malaria cases. These provinces are part of the Eastern Islands region. Comparing the proportion of the cases per province with the total cases nationally, Papua showed a doubling proportion from 40.99% (103,298 of total cases 252,027) in 2014 to 88.79% (393,801 of total cases 443,530) in 2022. Meanwhile, some other provinces showed a considerable proportion decline from 2014 to 2022. In contradiction with Papua, the provincial proportion of malaria cases compared to national cases from 2014 to 2022, East Nusa Tenggara showed a substantial fall from 25.77% (64,953 of total cases 252,027) in 2014 to 3.57% (15,812 of total cases 443,530) in 2022.
Nationally, malaria testing volume (Figure 2) showed an increasing trend from 2020 to 2022, especially from 2021 to 2022; there was a doubling increase in the number of malaria tests. Of the increasing volume of testing provinces, four provinces are showing a decrease in volume from 2021 to 2022, including West Java, Banten, South Kalimantan, and Central Sulawesi. On the contrary, three provinces showed the highest increase in testing, namely East Nusa Tenggara, Papua, and West Papua.
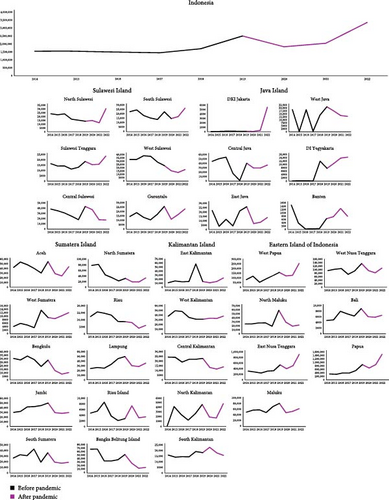
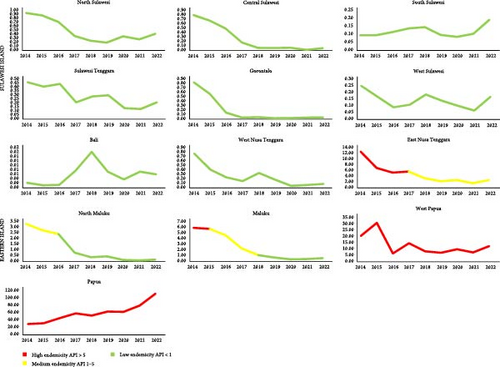
Over the study period, the Eastern Islands of Indonesia showed a stable increase that can be seen in Figure 3. The disproportionate contribution of the Eastern Islands, especially Papua, East Nusa Tenggara, and West Papua, with high numbers, becomes apparent. In detail, these three provinces showed a decrease between 2017 and 2019. However, all of those provinces saw a considerable increase in the number of annual cases in the last 2 years of study (2021–2022). Although Papua saw annual cases fall from 192,648 to 176,070 between 2017 and 2018, an enormous rise was observed from 2019 to 2022 (from 216,380 to 393,801). Meanwhile, West Papua saw cases fall from 13,706 to 7079 between 2017 and 2019; an increase was observed from 7628 in 2021 to 13,080 in 2022. Then, East Nusa Tenggara saw cases fall from 30,451 in 2017 to 12,909 in 2019; an increase was observed from 9419 in 2021 to 15,812 in 2022; among the increasing number of cases in the Eastern Islands, North Maluku, and Maluku presented a steady decrease. East Nusa Tenggara, West Nusa Tenggara, and West Papua rose last year.
On the contrary, Sumatra Island and Sulawesi Island displayed a stable decrease over the last 8 years, from 26,724 in 2014 to 8433 in 2021 (by 68.44%) and 7521 in 2014 to 2198 in 2021 (by 70.78%), respectively. However, in the last year, both islands showed a rise. Despite the progress in the last 8 years on Sumatra Island, North Sumatra, Riau, Jambi, and West Sumatra showed an alarming rise in 2022; 106.48% (2695 cases), 101.9% (914 cases), 576.92% (225 cases), and 173.61% (125 cases), respectively. Meanwhile, Sulawesi Island, Central Sulawesi, and West Sulawesi showed rapid increases above 100%; 208.93% (117 cases) and 159.14% (148 cases), respectively.
Java Island and Kalimantan Island showed a fluctuating trend. Despite having the lowest malaria cases compared to other regions, provinces in Java Island indicated a rise in the last 2 years. The increase for the last 2 years was shown by DKI Jakarta, Banten, DI Yogyakarta, and Central Java province. Although DI Yogyakarta and Banten had the lowest malaria cases in 2022, the increase of both cases was more than 200% (DI Yogyakarta is 488% [122 cases] and Banten is 260.87% [60 cases]). Meanwhile, provinces in Kalimantan Island indicated the same trend as provinces in Java Island, where all the provinces increased in 2022.
Figure 4 shows the incidence rate of malaria in 34 provinces. The Eastern Islands consistently had the highest incidence rate of all the island groups throughout the 9-year surveillance period. The highest endemic peak occurred in 2022, with 19.96 cases per 1000 person-years. After a period of the lowest point in 2015, the incidence rate of 8.53 per 1000 person-years rose considerably between 2016 and 2022 and remains high at over 10 per 1000 person-years. On the contrary, Sumatra, Java, Kalimantan, and Sulawesi Islands showed the lowest incidence rate under 1 case per 1000 person-years during the study period. However, having the lowest incidence rate per 1000 person-years, followed by Sumatera Island among other Islands, Java Island and Sumatra Island presented two points of time increase in incidence rate consecutively (2021 and 2022). On the other hand, Sulawesi Island showed an increase in incidence rate in the last year of the study.
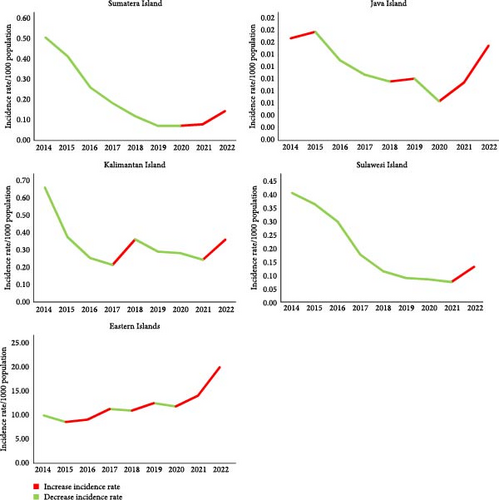
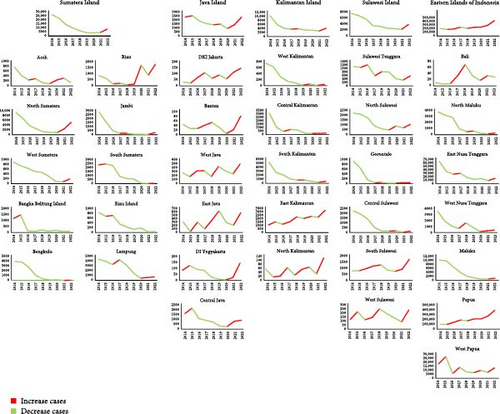
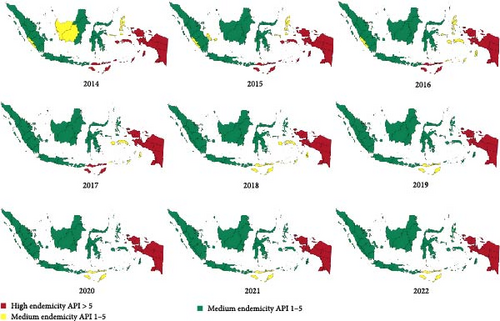
Figure 5 maps the endemicity rate by province over time, measured as the API per 1000 at-risk population. Provinces are classified as being low endemicity (API per 1000-at-risk population is less than 1), medium endemicity (between 1 and 5), or high endemicity (above 5). Generally, the endemicity rate has decreased consistently over time. Progress was seen in provinces on Kalimantan Island and Sumatra Island. In 2014, there were two out of five provinces on Kalimantan Island with medium endemicity. Within a year of progress, all provinces reached low endemicity. Meanwhile, in the provinces on Sumatra Island, in 2014 and 2015, there were two provinces with medium endemicity. Then, in 2017, all provinces in Sumatra Island were declared to be low endemicity. Java Island and Sulawesi Island showed consistent progress. Provinces in both islands could maintain low endemicity during the study period. Despite the achieved progress on other islands, the Eastern Islands of Indonesia showed fluctuating progress. A remarkable progress was shown in East Nusa Tenggara, North Maluku, and Maluku. Those three provinces have shown progress in 3 years consecutively (2016–2018). Maluku had medium endemicity in 2016 from high endemicity. North Maluku reached low endemicity in 2017 from medium endemicity in 2014. East Nusa Tenggara lowered the endemicity from high to medium in 2018 and maintained the progress until 2022. On the other hand, Papua and West Papua remained in the high endemicity category.
API is measured as the total number of positive slides for a parasite during a year per 1000 at-risk populations. The API can be seen in Figure 6. Nationally, the API for Indonesia is 1.61 per 1000 at-risk populations in 2022. The provinces with the highest API by far were Papua, West Papua, and East Nusa Tenggara during the 9 years of the study. West Papua displayed the highest API in 2015 (31.29 per 1000 at-risk populations), but this decreased sharply in 2016 and increased in 2017 then remained stable under 15 after 2017. East Nusa Tenggara also exhibited a high API of 12.81 per 1000 at-risk populations in 2014, which consistently declined until 2021. Papua’s API reached a local maximum of 113.07 in 2022. The API of the province declined enormously between 2017 and 2018 from 59.00 to 52.99 but remains 17 times higher than that of any other province outside the Eastern Islands.
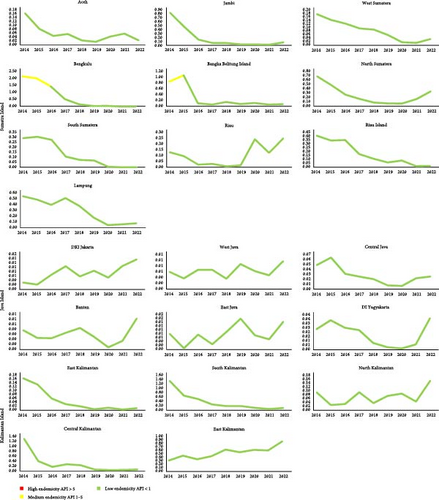
Some other provinces on Sumatra, Java, Kalimantan, and Sulawesi Islands showed a low endemicity. The API of provinces in Java, Sulawesi, Sumatra, and Kalimantan remained below 3 for the entire study period. However, some provinces on those islands had fluctuation and increased API in 2022. For example, Riau, all provinces on Java Islands, North Kalimantan, East Kalimantan, West Sulawesi, and South Sulawesi, had an increased API in 2022.
We must also touch on the changing contribution to the national caseload of the Eastern Islands, especially of Papua province. The portion of the national caseload attributable to the Eastern Islands has generally risen over time, and within this trend, the contribution of Papua over the other Eastern Islands provinces has become more salient over time. This suggests that the national strategy for malaria elimination has been less successful in the Eastern Islands than in the country as a whole and specifically that the response in Papua has been less pronounced.
4. Discussion
Our results show that over 9 years of surveillance, the incidence of malaria fluctuated. However, over the last 4 years, the incidence showed a steady increase nationally. In 2022, there were 32 provinces where malaria cases increased compared to 2021. However, the number of provinces categorized as high endemicity are two provinces, West Papua and Papua. While the decline in the API in the Eastern Islands also exhibited strong progress, endemicity remained high in Papua and West Papua with an API of over 10 per 1000 at-risk population.
This study benefited from being able to decompose national surveillance data by island and province and was able to track both the incidence rate and the endemicity of malaria. However, several limitations presented themselves. For one, data concerning malaria mortality were not available, so we were unable to report or analyze the severity of malaria cases. Second, data on the monthly parasite incidence (MOPI) were not available, so we relied on the API data instead, prohibiting any analysis of seasonal trends. Third, data on malaria caseloads were obtained from primary healthcare institutions and public hospitals, so cases of malaria from private clinics and hospitals were not captured. This creates a very significant risk of underreporting, especially in provinces that are highly reliant on private providers. Because of the possible endogeneity of the prevalence of private care provision, this also represents a considerable source of potential bias. Finally, information on the parasite species responsible for cases was not included in the MoH routine surveillance data and thus could not be included in our study. Given the difficulty reported in eliminating P. vivax and the different behavior of each parasite (e.g., in terms of drug resistance and response to treatment), routine surveillance initiatives must expand to include these data in the future. In addition to these concerns, sample size and power analyses were not performed.
Information about the parasite species responsible for each case is not collected as part of the MoH routine surveillance program used in this study [14], prohibiting analysis of trends by species. The Indonesian Basic Health Research survey (RISKESDAS) [15], most recently conducted in 2018, suggests that 50% of cases nationwide were caused by Plasmodium falciparum, 30% by P. vivax, 10% by P. malariae and 10% by other species.
Our results largely echo those of the wider contemporary literature in most of the provinces in Indonesia. Using surveillance data across 11 years in the Menoreh Hills, the study explained that the API of malaria had fallen over time [11]. A previous study in Purworejo found that the endemicity of malaria was low but that there remained a persistent occurrence of cases, with a change of strategy required to eliminate the disease completely [16]. In Malaysia, similarly, in several subdistricts, the incidence of malaria remains considerably high [17]. Along the border between Thailand and Myanmar, the incidence of malaria remains persistently high in certain geographical clusters [17].
A probable explanation of an increase in cases of malaria at several points in time (especially in 2015–2016 and 2019–2020) can be explained due to a better surveillance system in Indonesia. Indonesia has developed a better reporting system for malaria called “Sistem Informasi Malaria” or Malaria Informatic System (Sismal). Until 2024, the system has been updated or upgraded three times. The first version was a pilot project in three districts, including Indragiri Hilir, Rokan Hilir, and Pelalawan in Riau Province. However, the implementation of the system could not be run until 2015 [18]. Therefore, from 2016 to 2017, we can see an increase in malaria cases at the national level. The second version was launched in 2018 and implemented in 2019 until 2022. Then, we can see an increase in cases in 2019–2020 [19, 20]. By having an updated and improved malaria surveillance system, the data accuracy and timeliness can be improved. In addition, this accuracy and timeliness will increase the reported cases. In addition, another probable factor influencing the increased cases, especially in the last several years is testing volume. In 2022, it is recorded that more than a 50% increase in testing volume compared to testing volume in 2021. Lastly, climate change or temperature increase can be a factor influencing malaria cases increase [21]. In the World Malaria Report 2023, the World Health Organization mentioned the concern of climate change’s impact on malaria distribution and cases [22]. A study indicated that climatic factors, including precipitation, humidity, wind intensity, direction, and temperature, are associated with the growth of Anopheles and Plasmodium, leading to an increase in malaria prevalence [23]. A modeling study showed an increase in person-months at risk under two different emission scenarios (representative concentration pathways [RCPs]), RCP2.6 to RCP8.5, from the 2050s to the 2080s [24]. Indonesia Meteorological, Climatological, and Geophysical Agency recorded that there was an increase in temperature by 0.2°C in the 2022 observation compared to the 1991–2020 observation (26.8 and 27.0°C), respectively [25]. Therefore, an increase in temperature in 2022 can be a factor influencing the number of malaria cases.
The strong progress in reducing the incidence and endemicity of malaria may reflect the successes of the programs implemented by the MoH (especially during the first years of study), with funding support from the Global Fund. Sabang Aceh is a strong example of a province where local government intervention has achieved success in reducing the distribution of malaria cases [26]. The National Malaria Eradication Unit began the use of indoor residual spraying in Java in 1954, but the integrative approach to malaria control was not adopted until 2004. Here, ACT was introduced as a first-line treatment due to the high resistance to the previously used chloroquine. RDTs were ordered shortly after to supplement laboratory microscopic testing. In 2005, insecticide-treated bed nets were distributed in parts of Sumatra and eastern Indonesia. By 2009, this had been expanded to include the entirety of Sumatra as well as Kalimantan and Sulawesi. Since then, routine immunization and antenatal care have been combined with the distribution of insecticide-treated bed nets in highly endemic districts and villages on a biennial basis.
A 2009 ministerial decree aims to gain political commitment at the sub-national level to support the national target of eliminating malaria by 2030 [4]. However, Papua and West Papua remain high-endemicity areas with a high number of cases due to a number of unique characteristics of those provinces. Understanding the persistent prevalence of malaria in the Eastern Island provinces requires some insight into the socioeconomic and health contexts of that area. For one, Papuan and West Papuan communities tend to live in lowland, densely forested areas and are more resource-constrained than Indonesia as a whole, worsening the baseline risk of contracting malaria [7, 27, 28]. The topography and ecology of these regions result in numerous swamplands and bodies of standing water, which constitute a good breeding ground for the malaria cycle [29, 30]. Lowlands also tend to have a higher density of anopheles than highland regions [31, 32]. Further potential risk factors specific to Papua and West Papua include the prevalence of forest-related activities, poor housing conditions and infrastructure, limited access to health facilities, and the prevalence and nature of nighttime activities [7, 8]. Specifically, the limited access to health facilities may render more difficult the rollout of interventions through existing healthcare systems, and the lower quality of infrastructure relative to other regions of the country may render remote and rural areas more difficult to reach with traditional interventions.
Little is known about the social and spatial distribution of malaria in the Eastern Islands and malaria mapping [7]. Drug resistance among both P. falciparum and P. vivax is a major concern [9, 33], and considerable spatial variation in malaria incidence exists within this region [7]. P. vivax is more common for children under five here, although falciparum is more common overall [33–36]. As well as being associated with mortality and repeated infection in children and overall [33–35], P. vivax in this region has been less likely to be detected by RDTs and is less likely to respond to ACT and other malaria control policies [33, 37]. In Papua, between 1992 and 1994, chloroquine-resistant P. vivax was observed. In 1995, chloroquine treatment failure for P. falciparum and P. vivax in north-eastern Papua was found. A study conducted in Alor, Nusa Tenggara, showed chloroquine treatment failure in 2001-2002 [38]. Some authors have also called attention to the shortcomings of existing surveillance strategies in this region, noting the risk of distinct parasite subpopulations in the community remaining undetected by passive surveillance [39]. Finally, many people in these provinces seek malaria treatment from private providers who are less likely to adhere to national guidelines than public providers [40].
The composition and behavior of malaria vectors present in the Eastern Islands may help to understand the persistent disease prevalence in this region. The primary malaria vectors in the Southwest Pacific belong to the Anopheles punctulatus group, including (among other species) An. punctulatus, An. farauti, and An. farauti 4 [41, 42]. In eastern Indonesia, data suggest that An. farauti 4 enters houses at a high rate, is highly prevalent outdoors, and bites humans at a high rate during the early evening, all of which increase the chance of making contact with humans and acting as a malaria vector [43]. It is also thought that selective pressures due to indoor residual spraying and insecticide-treated bed nets contribute to the shifting of biting behavior of vectors in this group to earlier in the night [44]. A range of vector control policies have been implemented at the national level, including in the Eastern Islands. These include indoor residual spraying (recommended since 1959), larval control (used since 1990), insecticide-treated nets, and long-lasting insecticide nets (LLINs) (distributed for free since 2006) [44]. The efficacy of these policies in the Eastern Islands is still being investigated, however. For instance, the WHO is in the process of collecting and analyzing data on the efficacy of LLINs in Papua province, including the recording of sociodemographic data and household characteristics [44].
These provinces will ultimately benefit from the mobilization of significantly more resources for ongoing initiatives to combat malaria, as well as a greater degree of coordination in these initiatives. Another useful step is the continued identification of risk factors for infection, as well as the assessment of potential interventions. Recent literature from the area has identified an increased risk of infection among the poor, as well as those who live in rural, densely forested, and lowland areas [7], and a lower risk of infection among those who use measures such as insecticide-treated nets, insect repellent, electric rackets, coils, and window screens [45]. As well as continuing to improve the provision of these items as part of the ongoing program to combat malaria, public health professionals should pay particular attention to forested, poor, and lowland regions.
The Indonesia MoH reported that until 2023, there are five provinces and 381 districts/cities that have successfully eliminated malaria. Those provinces are DKI Jakarta, East Java, Bali, Banten, and West Java [46]. Since the smallest unit of this study analysis is a province, this study will not discuss at districts/cities level. Several malaria cases were found in malaria-free areas such as DKI Jakarta, East Java, Bali, Banten, and West Java. Import cases are the explanation for the situation. Import cases are contributed by several conditions, including migration from non-malaria-free areas or high endemicity to low and medium endemicity, migration surveillance failure, and natural disaster [47].
The government of Indonesia planned malaria elimination in 2030 under the MoH Decree number 293/MENKES/SK/IV/2009 concerning malaria elimination in Indonesia. The malaria elimination was conducted in four stages, starting from DKI Jakarta, Bali, and Batam in 2010. Then, followed by Java Island, Aceh Province, and Riau Island in 2015. Sumatra Island, West Nusa Tenggara Province, Kalimantan Island and Sulawesi Island malaria elimination in 2020. Finally, in the provinces of Papua, West Papua, East Nusa Tenggara, Maluku, and North Maluku in 2030. There are eight strategies under the decree, including (i) early detection and effective treatment; (ii) community empowerment and mobilization for active participation in the elimination program; (iii) healthcare facility access for populations at risk; (iv) local government communication, advocacy, and education for active participation in the elimination program; (v) a coordinated partnership with local, national, and international partners including private sectors, profession organization, and social organization; (vi) surveillance, monitoring, evaluation, and health informatics; (vii) malaria elimination effort through the partnership program, and (vii) human resource capacity building and technology development [48].
A number of further interventions are suggested in the literature. Engaging with private sector treatment providers may also help to ensure access to affordable and high-quality care [40]. The adoption of different surveillance strategies should also be sought [39]: one possibility would be to use hematological markers such as platelet count, white blood cell count, and lymphocyte count, which were found to be more strongly associated with malaria diagnosis than clinical symptoms in the Eastern Islands [49]. Providing intermittent preventive treatment to pregnant mothers, rather than one-time screening and treatment, has also been deemed highly cost-effective in this geographical context [50]. Recent literature continues to support the role of socioeconomic factors in influencing the risk of infection in that region and suggests that education is associated with the rate of malaria self-reporting [51]. This reaffirms the role played by malaria-sensitive interventions that target human development outcomes.
The MoH may also explore employing a culturally tailored participatory learning and action (PLA) cycle approach to work with communities in the Eastern Islands to maximize health-seeking behaviors and intervention uptake. The PLA cycle has already shown great success in designing and codesigning interventions for resource-constrained contexts [52]. This approach could inform the design of an intervention that is tailored to the economic, cultural, and geographical context of Papua and West Papua, which should supplement the existing integrative approach which emphasizes the use of RDTs, deploys ACT as a first-line treatment, and distributes insecticide-treated bed nets. Given the prevalence of livelihood activities, which may exacerbate the spread of malaria, prevailing approaches may be difficult to implement in this locale, and a participatory approach could help to enlist residents to integrate malaria-relevant health-seeking behaviors into daily life in a way that is more acceptable to them.
Further commitment of organizational capacity and financial resources to the Eastern Island provinces will be necessary if the Indonesian MoH is to achieve its target of eliminating malaria by 2030. In addition to this, alternative public health interventions may be considered to supplement the existing approach. As indicated by the examples of Malaysia, Myanmar, and Thailand, even when malaria incidence is greatly reduced at the national level, endemicity can remain persistent in geographical pockets [17]. Although the MoH’s integrative approach to malaria control appears to have been highly effective, and there has been a considerable decline in malaria incidence and endemicity in Papua and West Papua, this approach could be augmented by a more regionally tailored approach to avoid persistent pockets of malaria in the Eastern Islands.
5. Conclusion
Using surveillance data from 34 provinces of Indonesia, we examined the spatiotemporal trends in the incidence rate (total cases and cases per 1000 person-years) and endemicity (measured as the API per 1000 at-risk population) of malaria over 9 years from January 2014 to December 2022. We found that the endemicity and incidence of malaria decreased greatly throughout the period surveyed, likely as a result of the Indonesian MoH’s integrative approach to malaria elimination. Although progress has been made in every region of the country, malaria remains stubbornly prevalent in Papua and West Papua. In order to continue progress to meet the goal of nationwide malaria elimination by 2030, additional organizational capacity and financial resources must be dedicated to malaria elimination programs in these areas. In order to prevent the persistence of endemic malaria pockets in Papua and West Papua, surveillance must also be improved, with supplementary culturally tailored interventions being considered. Data on the parasite species responsible for malaria cases should also be integrated into the routine surveillance initiatives of the MoH. In addition, further research direction is evaluating the implication of Sistem Informasi Malaria” or Malaria Informatic System (Sismal).
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
No funding was received for this research.
Acknowledgments
The authors wish to extend their gratitude to the Vector-Borne and Zoonotic Diseases Control Directorate, Indonesian Ministry of Health, who have provided the data. We also convey our gratitude to all surveillance teams in 514 districts/cities across 34 provinces of Indonesia, who have been routinely collecting malaria data to support the malaria control strategies in Indonesia.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.