Comorbidities and Treatment Options for Acne Keloidalis Nuchae
Abstract
Acne keloidalis nuchae (AKN) is a condition that involves chronic inflammation of the hair follicles on the occipital scalp and posterior neck that often progresses to keloid-like plaques. AKN has most commonly been reported to affect postpubertal males of African descent. The cause of AKN has not been definitively described; however, it is likely an inflammatory response to trauma or infection of the scalp. AKN is associated with chronic scalp folliculitis, hidradenitis suppurativa, folliculitis decalvans, acne mechanica, keratosis follicularis spinulosa decalvans, cutis verticis gyrata, metabolic syndrome, acanthosis nigricans, and hypothyroidism. Treatment for AKN begins with topicals, antibiotics, and intralesional steroid injections. Refractory cases are treated with laser and surgery. Isotretinoin, cryotherapy, phototherapy, electrosection, and radiotherapy have also been effective in treating AKN but are less commonly used. In this review, we describe the existing understanding of AKN with a focus on comorbid conditions and available treatment options.
1. Introduction
Acne keloidalis nuchae (AKN) is a chronic inflammatory condition of the hair follicles, predominantly involving the occipital scalp and posterior neck. It typically begins as papules and pustules that coalesce into keloid-like plaques, resulting in scarring alopecia [1]. AKN is most prevalent and typically described in individuals of African descent, although one retrospective study reported a significant proportion of Hispanic patients diagnosed with AKN [2] and another described AKN in several Asian males [3, 4]. Thus, while the prevalence of AKN in people of color is estimated to be 0.5–13.6% and it is most common in Fitzpatrick skin phototypes V and VI, AKN should be considered in any patient with scarring folliculitis of the posterior neck [3, 5]. The condition occurs 20 times more frequently in males than females, suggesting a potentially causative role of androgens in its pathogenesis [5]. It has a typical onset after adolescence and before age 55 [1, 6]. The exact pathogenesis of AKN is unknown, but it has been hypothesized to be multifactorial, attributed to inflammation, trauma, immunosuppressive treatments, ingrown hairs, and infection after haircuts [7, 8].
1.1. Clinical Manifestations
AKN often presents after a patient receives a closely shaven haircut that results in ingrown hairs. It manifests as inflammatory pustules that progress to fibrotic papules at the site of trauma, likely driven by an inflammatory mediated deposition of collagen [9]. Secondary bacterial infections are common, presenting with pustules, sinuses, and abscesses [6]. Commonly reported symptoms are pruritis, pain, and bleeding [7]. Risk factors that may contribute to the development of AKN include curly or kinky hair, bleeding during haircuts, and frequent haircuts, especially short haircuts and head shaving [1, 10]. AKN patients do not usually have a family history of keloids, nor do they typically have keloids in other cutaneous areas; recurrence of lesions after excision is much less common than with typical keloids [11].
1.2. Histological Features
AKN presents initially with acneiform follicular dilatation and follicular rupture. This often progresses to dense hypertrophic scars or keloid-like scars, which may extend into the subcutaneous tissue [12]. Inflammation begins around the infundibulum before extending down the follicles [12]. There is initially neutrophilic inflammation, but over time, the infiltrate becomes predominantly lymphocytic with admixed plasma cells and foreign body giant cells [12]. Granuloma formation may occur around fragmented hair shafts [12]. Inflamed or destroyed follicles with the complete disappearance of sebaceous glands have also been observed [6]. Hair follicles may be replaced with connective tissue [6]. It is for these reasons that AKN is considered a form of primary scarring alopecia.
Recently, in a study of 41 patients with AKN, perifollicular infundibulo-isthmic lymphocytoplasmic infiltrates and fibrosis (PIILIF) was observed in 100% of patients and could be a subclinical precursor of AKN [13]. The authors suggest that based on various influences, such as lesion location, hormones, and trauma, PIILIF progresses to AKN. PIILIF has also been found in areas of AKN outside the scalp and other primary cicatricial alopecia conditions. Thus, the authors propose that PIILIF could be a unifying condition between these diseases [13].
2. Methods
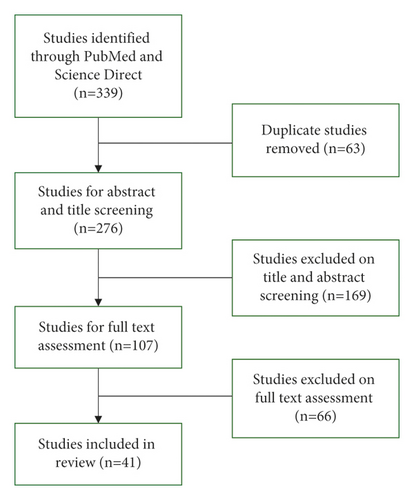
A literature review of the National Library of Medicine PubMed database and the Elsevier ScienceDirect database was performed in March 2023. The search term “acne keloidalis nuchae” was used in both databases. This returned 339 unique references published from 1959 to 2023. Article titles and abstracts were screened for relevance to AKN comorbidities and treatment options (Figure 1).
3. Results
3.1. Associated Comorbidities
AKN has been observed in patients who have other comorbid inflammatory conditions (Table 1). Severe AKN is associated with chronic scalp folliculitis [14] and hidradenitis suppurativa (HS) [15], supporting the role of chronic inflammation in the development of keloid-like plaques [14]. Folliculitis decalvans (FD) has been observed alongside AKN with FD lesions occurring proximal to AKN in the occipital scalp, suggesting a pathogenic association between the two conditions [16].
|
|
|
|
AKN has also been documented in patients with trauma to the skin of the nuchal region. Acne mechanica, which is characterized by pustules, cysts, and nodules in areas of mechanical trauma, has been described as a precursor to AKN in adolescent male football players [17]. Keratosis follicularis spinulosa decalvans (KFSD), which is characterized by widespread keratosis pilaris of the scalp and eyebrows, may have associated AKN when it occurs in the nuchal area since this location is prone to keloid-like scarring [18, 19]. An association between AKN and cutis verticis gyrata (CVG), which is a thickening of the scalp with excessive folds, has also been described [20, 21]. Both CVG and AKN are the result of dermal fibroblast hyperactivity and may be caused by upregulated TGF-β activity [21].
AKN is associated with all four components of metabolic syndrome (diabetes mellitus, hypertension, obesity, and dyslipidemia) [4, 14, 22, 23]. Regarding hypertension, the association with AKN may be partially explained by the increase in the renin-angiotensin system that causes arterial vasoconstriction and consequent hypertension. An increase in angiotensin II concurrently leads to increased expression of TGF-1, which promotes fibrogenesis [22]. Regarding obesity, increased body mass index (BMI) often results in increased skin folds on the neck and occipital scalp, which can induce mechanical trauma to the area, potentially causing AKN [22, 24]. AKN has also been reported in patients with acanthosis nigricans, a cutaneous marker of obesity and metabolic syndrome [25]. Regarding diabetes, insulin resistance has been implicated in the pathogenesis of AKN [4, 14]. Patients with AKN are also much more likely to develop new-onset hypothyroidism, which may be driven by a change in autoimmunity related to the pathogenesis of AKN [26].
Although further studies are necessary to support these associations, physicians should be aware of these possible comorbidities when evaluating patients with AKN to better manage their overall health.
3.2. Prevention
Prevention is of utmost importance given the often traumatic nature of the development of AKN. Barbers can be informed about haircutting techniques that reduce the risk of development of AKN, such as limiting close shaving, recommending reduced frequency of haircuts, and avoiding injury to the skin during haircuts [10]. Barbers can also refer individuals suspected of having AKN to local healthcare providers. Barbers have a personal connection with the community members that they serve and are trusted by them. Thus, if educated properly about AKN, barbers can serve as liaisons between community members and healthcare professionals. Barbers have shown a willingness to provide health education, making this a promising method for AKN treatment facilitation and prevention [27].
3.3. Treatment
The goal of AKN treatment is to prevent further destruction and scarring of hair follicles and improve the appearance of keloid-like scars. Current treatment options for AKN include topicals (corticosteroids, calcineurin inhibitors, other immunomodulators, antibiotics, and retinoids), oral antibiotics, isotretinoin, intralesional steroid injections, cryotherapy, phototherapy, laser procedures, surgical excision, electrosection, and radiotherapy. Most treatment begins conservatively with topicals but often requires progression to more systemic or procedural modalities if there is a lack of response to treatment. In addition, some patients may require adjuvant therapy to achieve the best possible outcome.
3.3.1. Topicals
Topical treatments are used for mild to moderate cases of AKN. Topical corticosteroids and topical retinoids are often prescribed and have been effective in managing AKN; they are particularly useful as preventative therapy [1]. Imiquimod 5% cream once daily for 8 weeks versus pimecrolimus 1% cream twice daily for 8 weeks specifically has also been reported to be effective in reducing the number of AKN lesions and improving the cosmetic appearance of AKN [28]. For patients treated with imiquimod, the average number of lesions decreased from 12.5 to 9, and with pimecrolimus, the average number of lesions decreased from 10.3 to 8.5 in one study [28]. Topical antibiotics, such as clindamycin 1% twice daily and mupirocin ointment, have also been used to treat mild inflammatory AKN [12, 29].
3.3.2. Oral Antibiotics
Oral antibiotics are another first-line treatment option for AKN and are recommended if lesions are purulent or draining; no study exists examining their actual efficacy though long-term oral tetracyclines are effective in reducing inflammation in AKN [29]. Cultures can be obtained to determine the causative bacteria and ensure an appropriate antibiotic is prescribed [30].
3.3.3. Isotretinoin
Oral isotretinoin (0.25–1.0 mg/kg/d) has been used to treat severe AKN, often in combination with other treatment methods such as cryotherapy, topical and oral antibiotics, and intralesional triamcinolone [1, 31]. In one study using isotretinoin alone, inflammation was improved, although the number of fibrotic papules remained unchanged [1].
3.3.4. Intralesional Injections
Intralesional (IL) corticosteroid injections of triamcinolone acetonide (Kenalog) are used in AKN to decrease inflammation and flatten scars [32]. The recommended concentration is 5–10 mg/mL, and larger lesions should be injected using larger needles [32].
3.3.5. Cryotherapy
Cryotherapy, performed in at least 3 sessions four weeks apart, has been shown to flatten AKN lesions. It works best on early, vascularized lesions [32].
3.3.6. Phototherapy
One study showed that narrowband UVB phototherapy 3 times per week for 16 weeks has been shown to improve AKN appearance and reduce the number of lesions present. It may also induce collagen matrix remodeling [33]. Treatment was started using the patients’ minimal erythema dose (MED) and increased by 20% each week until week 8, as tolerated. For weeks 9–16, a maintenance dose equivalent to that given at week 8 was used [33].
3.3.7. Laser
Laser treatment can be a highly effective long-term treatment option for AKN [5]. The success of AKN treatment often depends on the removal of the hair within lesions. Diode lasers can be used for hair epilation in patients with AKN, which was shown to prevent new AKN lesions from forming due to thinning and softening of the hair [34]. In these two cases, diode laser treatment was shown to be effective in Fitzpatrick IV and V skin types, without producing unwanted hypo- or hyperpigmentation [34]. Given the location of AKN, a good cosmetic outcome is often achievable with a laser [35]. Long-Pulsed 1064 nm Neodymium-Doped Yttrium-Aluminum-Garnet (Nd: YAG) laser and Erbium: YAG laser treatment have been shown to improve AKN by reducing the number of papules and size of plaques without producing skin dyspigmentation [36, 37]. Treatment with Nd: YAG laser has even been shown in one study to decrease sclerosis and the inflammatory infiltrate found in AKN lesions [38]. The 755-nm alexandrite laser has also been shown to reduce the number and size of AKN lesions, without major side effects [39]. Carbon dioxide (CO2) laser excision has also been used to successfully treat AKN with minimal pain and a low incidence of lesion recurrence. However, unlike other lasers, treatment is complicated by the creation of wounds that resolve by secondary intention healing which can lead to a prolonged recovery time [40].
Laser treatment can be painful for patients; therefore, topical anesthetics are usually offered. One study found that topical 2.5% lidocaine/2.5% prilocaine cream resulted in significantly lower self-reported pain scores compared to 7% lidocaine/7% tetracaine cream during Nd: YAG laser treatment of AKN [41].
3.3.8. Surgery
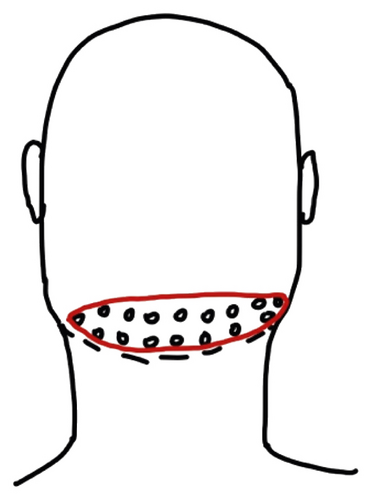
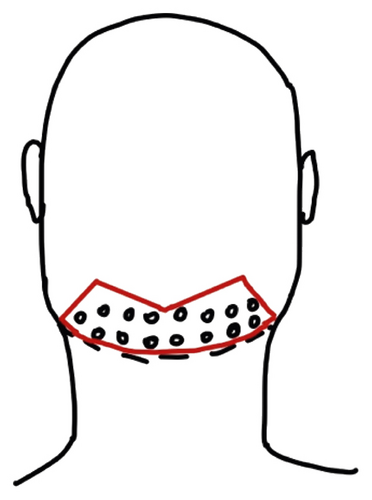
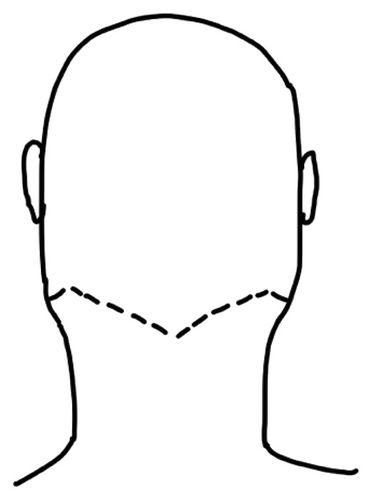
Surgery is often used when lesions are extensive or refractory to other treatment options. Because with surgery, hair follicles are removed and the likelihood of AKN recurrence in the excised areas is low. Complete surgical excision with primary closure is often used to achieve a favorable cosmetic outcome with minimal side effects [42]. Depending on the size of the lesion, a staged surgical excision with layered closures 3–6 months apart in time may be necessary [43, 44]. In single-stage excisions, a horizontal elliptical section that encompasses the posterior hairline is often removed, which allows the scar to be hidden by the newly formed hairline (Figures 2(a) and 2(b)) [42, 45]. Elliptical incisions can also be used for staged excisions, starting with the first excision at the inferior portion of the AKN lesion [43]. Another approach is a bat excision with tension sutures, which allows for different hairline patterns to be created (Figures 2(c) and 2(d)) [46]. Punch excisions are used for small papules or scattered lesions that cannot be included within the surgically resected area. These lesions can be left to heal via secondary intention [42]. Smaller lesions (<3 cm) that are located in the upper portion of the nuchal area are better suited to healing via primary closure as this area of the scalp is under less tension during head movement [47]. Hypertrophic scars secondary to surgery and recurrent AKN papules can be treated with intralesional corticosteroids, often resolving with treatment [43, 46].
Surgery on larger, deeper AKN lesions may require skin grafting. This procedure can be done in stages, allowing time for the wound to decrease in size before filling it with a split-thickness allograft. This reduces the overall size of the resulting scarring alopecia [48, 49]. In addition, negative pressure wound therapy can be used to shorten the time between the initial excision and secondary resurfacing and improve the final scar appearance [48, 49]. Complications of surgery include prolonged healing time, infection, and scarring.
3.3.9. Electrosection
Electrosection, which uses current to vaporize tissue, has been used to cut and coagulate large AKN lesions [50]. This procedure is quick and does not damage surrounding tissue. Wounds are left to heal via secondary intention [50].
3.3.10. Radiotherapy
Radiotherapy has been used to treat severe, refractory cases of AKN. Radiotherapy has been used to successfully reduce the size of keloidal masses caused by AKN [51, 52]. In one case, volumetric modulated arc therapy using a dose of 35 Gy in 5 weekly sessions reduced the lesion size without recurrence at 19 months [51]. Another case used 10 sessions of 3 Gy at 6 MeV every other day for a total dose of 30 Gy using a Varian linear electron accelerator [52]. Low-dose radiotherapy has been used in a severe, widespread case of AKN, in which surgery and laser were not feasible options [53]. A dose of 2 Gy at 6 MeV per session for 20 sessions of volumetric arc therapy permanently eliminated the hairs in areas of clinically inflamed AKN. By eliminating these hairs, the AKN lesions also permanently resolved and excess tissue in these areas diminished [53]. Side effects of radiotherapy include erythema, desquamation, wound infection, skin pigmentation changes, fibrosis, alopecia, and an increased risk of developing a malignancy in the treated area [51].
4. Conclusion
Acne keloidalis nuchae (AKN) is a rare, but debilitating condition that occurs predominantly in males of African descent. Patients develop fibrotic papules and keloid-like plaques on the occipital scalp/nape of the neck that cause pruritis, pain, and bleeding. The exact pathogenesis of AKN is unknown, but it is thought to be due to trauma that results in subsequent inflammation and fibrosis. AKN is associated with other inflammatory conditions, such as chronic scalp folliculitis, hidradenitis suppurativa, and folliculitis decalvans. Acne mechanica, keratosis follicularis spinulosa decalvans, and cutis verticis gyrata have preceded AKN in some cases and may have contributed to its development. AKN has also been associated with metabolic syndrome, acanthosis nigricans, and hypothyroidism. Physicians must be aware of these potential comorbidities when evaluating patients with AKN to provide comprehensive care to these patients. This is especially important as some patients may not have primary care physicians whom they follow up with regularly. Thus, screening for underlying metabolic conditions in these patients and subsequent appropriate referral is appropriate in many cases.
An important component of AKN management is prevention. This can be achieved by educating community members of higher risk populations about AKN and ways to minimize risk, such as limiting close shaving, reducing the frequency of haircuts, and avoiding injury to the skin during haircuts. Local barbers can implement these techniques in their practice and disseminate this information to their clients. In addition, barbers can be trained to recognize AKN lesions. Individuals who are suspected of having AKN may be more receptive to a referral for care if it is given by a trusted person, such as their barber.
Treatment of AKN is important because this disease can have a tremendous impact on patient’s self-esteem and quality of life. In one study, 60% of patients with AKN stated that they think about their lesions all the time [54]. Current treatment options include topicals (corticosteroids, retinoids, and other immunomodulators including pimecrolimus and imiquimod), oral antibiotics, isotretinoin, intralesional steroid injections, cryotherapy, phototherapy, laser procedures, surgical excision, electrosection, and radiotherapy. Treatment choice depends on the severity of the condition as well as patient preference. More conservative treatments, such as topical agents, oral antibiotics, and intralesional steroid injections, are often used as first-line therapies. Laser therapy and surgery are usually reserved for more advanced cases that are refractory to first-line treatments. Of the lasers discussed, Nd: YAG is often preferred because it has an increased penetration depth, making recurrence less likely [42]. However, lasers are not always able to penetrate larger AKN masses. In these cases, surgical excision is often performed. Given the substantial potential impact of treatment on patients’ quality of life, additional prospective studies comparing treatment options for AKN would be beneficial since many treatments have only been described in case reports and retrospective analyses.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Acknowledgments
Open Access funding enabled and organized by SCELC 2023.
Open Research
Data Availability
No data were used to support the findings of this study.




