Follow-Up on Psoriasis Patients After Dead Sea Climate Therapy: Efficacy and Duration to Relapse
Climate Therapy and Duration to Relapse
Abstract
Studies find climate therapy (CT) at the Dead Sea of psoriasis efficient for induction therapy, but few studies address disease relapse, long-term maintenance using CT, confounders, and the patient perspective. CT combines sunlight, balneotherapy, stress reduction, and education. This study aimed to examine Dead Sea CT and relapse of psoriasis over a 2 years period, patients’ satisfaction, and treatment outcome and preference relative to other therapies. A structured questionnaire was offered to patients, who during the recent 2 years had undergone a 4 week course of CT at the Dead Sea. Patients included applied for a new CT session due to relapse of their psoriasis. Questionnaire items covered their recall of relapse, disease severity, potential triggers of relapse and patient’s preference relative to other treatment options. The study enrolled 40 patients, with an average age of 55.5 years. CT was highly effective and resulted in marked reduction in the affected skin area, from 16% to less than 1% of the body surface. The median time from CT to first visible new lesion was 4.8 months, to first bothersome relapse 6.1 months and to full blown relapse 8.0 months. Patient satisfaction with conventional therapeutic modalities, especially oral methotrexate, was reserved, and CT was generally preferred. Relapse after CT was an inclusion criterion, and patients with long-lasting healing were not assessed. CT for 4 week treatment course of moderate to severe psoriasis at the Dead Sea which was studied in patients with relapsing disease was highly efficient for induction for clearing of the skin, matching new biologicals. In the studied group, return to prestate level took median 8 months on average. Patients’ satisfaction with CT scored high, and maintenance through repeated Dead Sea treatments often is best treatment of this segment having intolerance or poor effect of other treatments, or fear of medicines as a personal attitude.
1. Introduction
Psoriasis is a chronic immune mediated inflammatory skin disease affecting 1.2%–4.5% of populations, with ethnic variation [1]. Therapies include topical medications, ultraviolet (UV) therapy, and systemic medicines. Some treatments are one-course induction therapy; others are long term treatment and maintenance. Climate therapy (CT) and UV lamps belong to the former group. CT is a special treatment for psoriasis based on natural resources, used in different forms long back in time [2, 3]. In Denmark, CT at the Dead Sea has been offered for 50 years to Danish patients who have special needs or wish to refrain from conventional medicinal therapy. CT has different forms and are also practiced in Jordan, Croatia, Gran Canaria, Tenerife etc. CT at the Dead Sea combines phototherapy by sunlight filtered in the special Dead Sea atmosphere extending 420 m under Mediterranean Sea level, balneotherapy using fully saturated salt water, mental stress reduction, and patient education with effect on epidermal and immune activation. Four-week treatment courses in spring or autumn seasons are organized under daily support on site by registered nurses. Management and quality are according to the Danish program controlled by dermatologists, who are responsible for treatment guidelines. Germany, Austria, and other countries follow similar principles.
Patients applying for CT undergo thorough evaluation. Allocation is based on national criteria developed in 2011 by the CT Committee of the Danish Dermatological Society (DDS). Assessment of psoriasis severity involves the Psoriasis Area Severity Index (PASI) score and the Dermatology Life Quality Index (DLQI) along with individual needs [4, 5]. The area of the skin with psoriasis can be measured by the palm of hand unit including the fingers representing 1% of the total skin surface of a person [6]. Past treatment experiences, including intolerance to or poor effect of medicines along with social factors such as stressful life, are considered as well.
A range of publications on the rationale and medical outcome of CT at the Dead Sea have been published. It is not possible to conduct head-to-head randomized controlled trials on CT versus medicines exemplified by methotrexate since CT is multimodal and cannot be blinded, and level I evidence of CT cannot be accomplished. Studies at evidence levels II, III, and IV have demonstrated high efficacy of CT in moderate to severe psoriasis used as induction therapy with major PASI reduction or cleared disease [2, 3]. Studies comparing PASI before and after a 4 weeks treatment course indicate that CT as induction therapy stands on par with the known effect of modern biologic therapies. The challenging question is the duration of the achieved effect of CT. CT is single course and not directly shaped for repetition and maintenance therapy albeit CT of course can be repeated depending on relapse and the individual need of the patient. Use of follow up CT sessions for maintenance of chronically relapsing psoriasis is, nevertheless, accepted common practice in a small segment of patients, who are intolerant or resistant to conventional therapies or have special attitude with fear of medicines.
Recognizing repeated CT in practice is commonly used first line maintenance treatment in a special segment of patients with recalcitrant disease, we aimed to extend the understanding of CT’s effect on psoriasis over time by measuring the relapse rate. CT is not directly comparable to narrow band UVB given in dermatology offices since CT is natural sun given 7 days a week under strict control of adherence to the 4 week fixed schedule and since CT is multimodal thus very different from UV-lamp monotherapy. No reference study on narrow band UVB applied to a comparable group under Danish dermatology clinics is available.
The primary aim of the study was to clarify time from CT to relapse of psoriasis measured as debut of the very first sign of new local activity, initiation of any medicinal treatment, and full relapse to the pre-CT level. Relapse time was measured using a questionnaire, relying on patients’ recall.
2. Materials and Methods
2.1. CT Standard Treatment Protocol
Patients with psoriasis given CT at the Dead Sea, Israel receive supervised daily treatments 7 days a week for 28 days and full body exposure to natural sun 2-3 h in the morning and 3-4 h in the afternoon omitting the middle of the day. This is combined with baths directly in the Dead Sea for about 1 h 6 week days for 28 days. The sodium chloride concentration of Dead Sea water is approximately 30% reaching full saturation. Bathing in the Dead Sea in the supine position while spontaneously floating on the surface of the sea illustrates the drift created by the salty water; salt crystals cover the bottom and the beach. The osmotic pressure gradient over the epidermis is extreme. The water is also rich in other salts and minerals. Any systemic or topical medicinal treatment of psoriasis is routinely stopped at onset of CT. Treatment is supervised on site by a team of Danish nurses with special experience, under the responsibility of dermatologists. Groups of about 25 persons are treated in the spring and in the autumn when outdoor temperature is warm and comfortable. Education is provided as group instructions and individually; learning among patients themselves also contribute. Comorbidities are screened. Facilities for physical exercise are available. The two CT sites at the Dead Sea, Kibbutz Ein Gedi, and Lot Spa Hotel in Ein Bokek, follow identical protocols.
The 4 week CT treatment course in Israel is fully paid for by the public health service if ordered by hospital dermatologist authorized to prescribe this treatment. The cost of a 4 week course is about 5.500 EUR. Travel, stay, operation, and services in Israel were delegated to two nominated companies: 1BedreLiv and Victor Health Travel. Bispebjerg University Hospital is responsible for quality control of the two centers in Israel.
2.2. Study Design
This study employed a predefined questionnaire developed for the study. Questions were simple and in lay Danish. The questionnaire had been validated in test patients with respect to clarity and uniformity of perception, precision of time estimates, openness relative to the expected range of opinions and the nonleading nature of the questions. Questions addressed type and severity of psoriasis, the local CT site in Israel, efficiency/treatment outcomes rated at start and end of CT, time to relapse by recall, treatment preference referenced to other treatment options, patients’ overall satisfaction, and potential personal triggers of early relapse. The questionnaire was on paper and operated by patients themselves after a short introduction; being filled out it was checked for completeness. It took about 15 min to fill it out.
2.3. Study Location and Period
The study was conducted in January 2020 in the out-patient clinic of the Department of Dermatology, Bispebjerg University Hospital, Copenhagen. Patients had been routinely referred by their MD for active moderate to severe degree psoriasis and wish of CT in the coming spring season. New applicants of CT along with cases, who had received CT in the past, were examined.
2.4. Inclusion Criteria
- 1.
Patients with recalcitrant psoriasis, in severity moderate or severe, independent of type of psoriasis
- 2.
Patients who had received CT at the Dead Sea within the preceding 2 years
- 3.
Willingness to participate by voluntarily verbal consent after being informed on the study
2.5. Noninclusion/Exclusion Criteria
- 1.
Patients unable to respond to the questionnaire such as patients with cognitive, neurological, ophthalmic, and psychiatric diseases including abuse of alcohol or drugs.
- 2.
Patients who for any reason interrupted their previous CT course or were nonadherent to the defined day care curriculum with combined sun exposure and bath in the Dead Sea every six of a week; Sunday sun only.
- 3.
Any other major event during previous CT such as extraordinary weather conditions that might interfere with treatment outcome.
2.6. Self-Assessment of Psoriasis Severity
Patients were asked directly on inclusion to fill out the study questionnaire. Participants were requested to indicate to the very best of their recall the body surface area afflicted with psoriasis and the anatomical site of affection before and after their nearest previous CT treatment; according to inclusion criterion within a maximum period of 2 years. Disease affection was quantified using the size of palm unit, where one palm unit represented 1% of their total body surface area [6]. They had been instructed on how to estimate the affected skin surface area by palm unit while they were introduced to the questionnaire.
2.7. Measurement of Time to Relapse and Active Treatment of Relapse
- 1.
The duration (in weeks/months) until the onset of the first visible new or reoccurred lesion.
- 2.
The duration until the first bothersome or more widespread relapse.
- 3.
The duration until a full-blown relapse of severity comparable to the status before CT, or worse.
- 4.
The duration until they started self-treatment with local medicine or remedy, they themselves might have had at home, including alternative products.
- 5.
The duration until they started prescription medicine after contact with their doctor.
2.8. Registration of Patient Satisfaction and Treatment Preferences
Participants were asked to express their satisfaction with CT and other treatments such as local corticoids, D-vitamin analogues, methotrexate, biological therapy, alternative treatment, and UVB light therapy. The questions aimed to ascertain participants’ general attitudes toward these common psoriasis treatments, which could serve as alternatives to CT. It should also be indicated if patients in general or from personal experience might have a negative view on registered medicines thus seeking CT as their preferred alternative and way to refrain from undesired therapy.
2.9. Identification of Confounders and Triggers of Relapse
To identify potential confounders or triggers of relapse of psoriasis during the observation period, participants were inquired about significant life events such as loss of job, divorce, and severe diseases. Among close family members, or other stressful incidents that could exacerbate psoriasis and lead to an early relapse.
3. Ethics and Institutional Approval
The study is production control, quality control and development of hospital instituted treatment and thus according to Danish law need no formal approval. The study is conducted in Denmark on Danish citizens and CT offered to our patients is organized by the county, Region Hovedstaden. The study is according to the local embassy not in conflict with Israeli formal requirements.
4. Results
4.1. Patient History and Previous Treatment With CT
The study took place on two days in January 2020, before the Corona pandemic; a total of 40 patients were enrolled. 31 had received a treatment course in 2018 and 28 in 2019. Seven patients who applied for CT for the first time thereby having no experience on relapse from CT were not included in the study. Thus, among 47 patients examined 85% had relapsing psoriasis outbreak and wish of a new CT treatment course. In 2018 and 2019, in total, 135 patients had been prescribed CT at the Dead Sea. Many reported negative experiences with standard treatments including intolerance and poor or no effect. The assessment also included modern biologics. Some were afraid of medicines in general and preferred treatment from nature’s resort. Some appreciated the combinatory principle of CT including group experience and patient-to-patient learning.
4.2. Demography
Study participants were 20 males and 20 females. The mean age of the participants was 55.5 years (± SD 15.29), with an age range of 13–78 years. Among the participants, 27 resided in the resort Kibbutz Ein Gedi, while 13 resided in Lot Spa Hotel in Ein Bokek during their respective stay.
4.3. Affected Skin Area Before and After CT
Among patients included, 30 were diagnosed with Psoriasis vulgaris, three with guttate psoriasis, three with inverse psoriasis, two with pustular psoriasis, and two patients presented with overlap types of psoriasis.
Prior to their most recent CT in Israel, the mean total skin area affected by psoriasis were 15.9 palm units (median 9.5, range 1–55). Following their return from CT, the mean affected area reduced to 0.6 palm unit (median 4.5, range 1–8). This corresponds to approximately 16% of the total body surface area before CT and less than 1% after CT.
4.4. Time to Relapse and Reinstitution of Treatment
- •
Time until the onset of the first visible new or reoccurred lesion: 4.8 months, ranging from 1 week to 10 months.
- •
Time until the first bothersome or more widespread relapse: 6.1 months, ranging from 1 week to 12 months.
- •
Time until a full-blown relapse of severity comparable to the status before CT, or worse: 8.0 months, ranging from 2 weeks to 30 months.
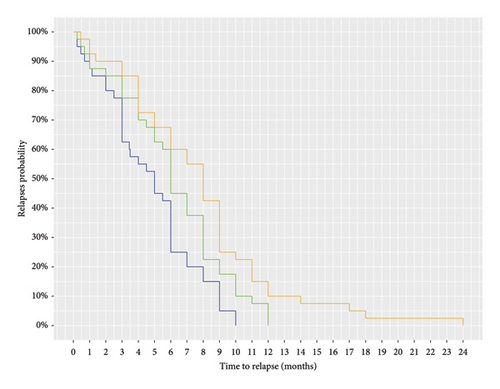
See individual patient reports of relapse, Figure 1, and Kaplan–Meier plot on relapse over time, Figure 2. Figure 1 illustrates individual variation.
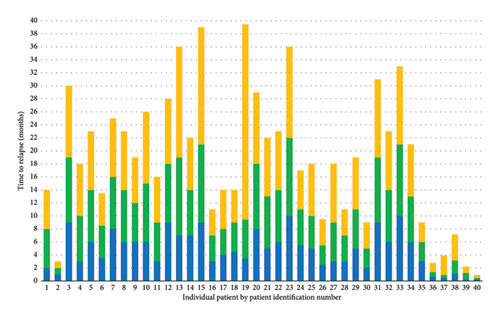
The study is descriptive. Prestudy power calculation was not performed since, obviously, detailed statistical comparison of subgroups would require a larger sample.
A few patients namely 6 reported immediate relapses. In these participants, personal factors such as life events with loss of job, death of a close family member, or high level of stress and conflict in the family or on the job were reported. Such stressful trigger factors may easily explain poorer response and hastened return of visible symptoms and active disease.
4.5. Self-Administered Treatment of Relapse and Contact With Medical Professionals
Patients’ use of previously prescribed medications took place after median 5 months, range 0–21, after CT and homecoming. The first contact with a medical professional due to psoriasis flare-up occurred after median 5 months, range 0–12. Thus, treatment of relapse was variable and mostly late.
4.6. Patient’s Opinion on Specific Treatments
Patients’ overall confidence in medicinal treatments of psoriasis showed 39% to be positive, 53% negative, and 8% indifferent; missing data in two patients. Trust in specific treatments is shown in Table 1.
| Positive (%) | Negative (%) | Indifferent (%) | |
|---|---|---|---|
| Topical corticoid | 45 | 34 | 21 |
| Topical vitamin D | 47 | 32 | 21 |
| Oral methotrexate | 5 | 82 | 13 |
| Biologics, injectable | 21 | 53 | 26 |
| Light, UVB lamp | 50 | 32 | 18 |
| Alternative remedy | 24 | 29 | 47 |
5. Discussion
Earlier research has reported varying time to relapse after CT, ranging from 3 to 8 months [2, 7, 8]. The disagreement between reports can be explained by differences in how relapse was defined and assessed across studies. Studies do not specify the condition or disease state counted as relapse.
Our study found CT highly effective with reduction of the affected skin area, from mean 16% of the total body surface area before CT to less than 1% after CT. This reduction is comparable to earlier research that also reported major reduction in PASI scores following CT. CT, thus, is concluded highly efficient as induction therapy of moderate to severe psoriasis, matching the known efficiency of modern biologicals.
CT is prescribed as single-course treatment on Doctor’s order. Reality, however, is different seen in a longer perspective. In our study 85% of patients who applied for CT had received this treatment before. They often disliked systemic treatments especially methotrexate. Some had experienced poor efficacy or drug intolerance in the past making CT a logic maintenance treatment. Patients applying for CT are special in their experience and priority of treatment.
In a Danish study from Roskilde University Hospital of 49 patients with psoriasis conducted by Trøstrup et al. in 2019, the aim was to evaluate the impact of CT on psoriasis by measuring changes in PASI and DLQI scores at three scheduled visits, for example up to about 3 months before CT, 1 month after CT and 4–6-month post-CT as follow-up [9]. Thus, the gap between earliest baseline record and latest follow up visit was 9 months, with 4 weeks CT positioned variably in between; unfortunately, no record of the scheduled 1 month post CT visit took place, and relapse was assessed from two visits only. Scorings were performed by a trained nurse. The study did not define what was read as a relapse. The study provided limited information.
Our study relied on patients’ own recall, which is a continuous timeline not dictated by scheduled visits. The strength and limitation of our study is that it builds on individual recall.
Duration to relapse after CT is a critical factor for long-term maintenance of psoriasis. Our finding of median time 8.0 months to full-blown relapse is in the upper end of the broad range of previous published estimates [2, 8]. It’s noteworthy that time to relapse can be very short and skew overall findings if stressful triggers in patients personal life operate, as we observed. Our study gave examples such as loss of job and death of a family member. Another confounder minimizing measured time to relapse is inclusion bias namely that the most successful cases, who experienced nearly curative effect of CT and no relapse for years, did not apply for further CT and thus were not recorded. Time of the year after homecoming to the Danish climate is another influencer on disease severity and relapse. A review of psoriasis and seasonal variation estimates that 25% worsen in wintertime, 25% in the summer, and 50% are independent of season [10]. CT is available in spring and autumn thus prepared to meet patients’ seasonal profile. Spring is more popular since cleared skin can be freely displayed and exposed to sun in the upcoming holiday period. Disease and treatment holidays includes exit from the patient role are recognized fundamental patient needs in the adherence and skin literature [11–13]. The pleasure of treatment holiday may explain the observation that patients were late in their initiation of active treatment of relapse.
Psoriasis patients often are nonadherent to medicinal therapies [14]. Patients in our study expressed negativity toward systemic treatment, especially methotrexate but also to modern biologicals. Patients faithful to CT and having strong motivation for this treatment should be allocated to CT despite the expected decline of effect over time. CT is, from the adherence point of view, ideally controlled light therapy given 7 days a week for 4 weeks, a treatment dosing and discipline that never can be practiced under home condition. CT carries a potential risk of light induced skin cancer, which was reported in one study as a measurable albeit minor risk [7, 8]. Skin cancer resulting from CT is a potential risk but not a limiting factor in practice since sunscreens nowadays are used initially.
In Denmark 150,000 estimated citizens are diagnosed with psoriasis. CT is today given to about 300 Danish patients annually. Thus, CT is used in about 0.2% of the total patient population. Before the introduction of biologicals approximately 700 patients received CT annually, and approximately four of seven CT patients have switched successfully to this new highly efficient maintenance treatment of psoriasis, which adds prevention of co-morbidities such as cardiovascular disease and arthropathy associated with psoriasis [15, 16].
Our study was performed in a historical window with no influence of the corona pandemic and no outbreak of active war or unusual political uncertainty in this fragile region. Our study avoided such general confounders. This study describes routine Dead Sea CT as it was practiced for decennia.
Study limitations are a relatively small sample, selection bias related to allocation to CT, high percentage of patients with CT in the past thus recalcitrant disease and high risk of relapse, self-reported time to relapse based on patients’ recall, no comparative treatment group. The study is retrospective.
6. Conclusion
CT was confirmed highly efficient for induction therapy of psoriasis being on par with modern biologicals. CT is multimodal and combines intensified natural sun therapy, balneotherapy in the salty water of the Dead Sea, relief from daily stress at home and education from patient to patient and provided on site by health professionals. The reported mean time to full-blown relapse was 8 months. Patients applying for CT represent a small but distinct segment of psoriasis sufferers, about 0.2%, who have CT as their priority. CT 4 week treatment is practiced under conditions of ideal treatment adherence that cannot be achieved at home.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
The study used the facility of the university department and was not supported by any financial funding.
Open Research
Data Availability Statement
The data that support the findings of this study, including patient questionnaires on psoriasis severity, treatment outcomes, and relapse times, are available from the corresponding authors upon reasonable request. Due to privacy and ethical concerns, the raw data cannot be publicly shared but will be provided in an anonymized form where possible.




