An Innovative Single-Stage Approach of High-Tension Keloid Excision and Reconstruction Using Acellular Dermal Matrix and Epidermal Skin Grafting
ADM and Epidermal Graft Keloid Treatment
Abstract
The treatment of keloids, particularly in high-tension areas, is challenging due to their extension beyond the original wound boundaries and high recurrence rates, thereby rendering traditional treatments ineffective. In this study, we investigated the effectiveness of a novel single-stage treatment approach that combined acellular dermal matrix (ADM) with keloid-specific epidermal skin grafting. To further prevent recurrence after neo-skin formation, the treatment was followed by fractionated laser and radiation therapy (LCR). Seven patients with high-tension keloids, including one with keloids at two locations, were treated and followed-up for an average of 15.9 months. The patients showed significant improvements in wound healing and skin appearance, with a marked reduction in the Patient and Observer Scar Assessment Scale (POSAS) (scores from 91.1 ± 5.6 to 23.8 ± 6.1 (p < 0.001)). This approach effectively minimizes tension, reduces the likelihood of keloid recurrence, and serves as a viable alternative to conventional methods that often involve challenges related to donor-site acquisition. No recurrence was observed during the follow-up period, indicating a promising innovation in the management of extensive keloids and offering improved healing and esthetic outcomes, particularly in high-tension areas.
1. Introduction
Keloids are hypertrophic scars extending beyond original incision margins, frequently causing functional impairment and psychosocial distress due to their esthetic impact [1, 2]. Traditional therapies, including corticosteroid injections, surgical excision, and radiation, may yield inconsistent results with a high rate of recurrence, especially for keloids in high-tension areas [3, 4]. In particular, keloids in high tension or those occupying a substantial surface area are challenging due to possible recurrence after treatment. The primary approach is wide excision; however, they may require intricate reconstructive methods, such as local flap transposition, skin grafting, and tissue expansion [5–7]. Recent advancements in regenerative medicine have introduced novel approaches, such as the combined use of acellular dermal matrix (ADM) and epidermal grafting of the keloid. In this study, we investigated the effectiveness of a novel single-stage treatment approach that combines ADM with keloid-specific epidermal skin grafting, followed by fractionated laser and radiation therapy. This single-stage treatment approach is promising and addresses the underlying wound healing response induced by high tension, potentially reducing recurrence rates and the need for donor-tissue harvesting.
2. Methodology
Seven patients with high-tension keloids were enrolled, with one having keloids at two sites. After informed consent was obtained, a thin split-thickness graft was harvested from the keloid and transplanted onto an ADM scaffold (Pelnac, Gunze Ltd., Kyoto, Japan). The keloids were surgically excised to the normal underlying tissue, and ADM was applied to the wound to ensure tension-free closure. To ensure good matrix adherence to the wound, the grafts were secured in place with 3-0 silk sutures and a tie-over dressing, which were removed after a week. After a 21-day period to allow for new dermal tissue growth, the laser combined with radiotherapy (LCR) method was implemented. LCR involves a combination of fractional carbon dioxide (CO2) laser therapy at an energy level of 504 mJ, followed by two rounds of electron beam radiotherapy (9 Gy). The first radiotherapy session was initiated within 24 h of the laser treatment, and the second session occurred on the seventh day [8]. Laser therapy causes microthermal injuries in the keloid tissue, promoting collagen remodeling and increasing tissue sensitivity to radiation.
The primary result was evaluated using the POSAS. Follow-up periods ranged from 8 to 27 months, averaging 15.9 months. POSAS data are presented as mean ± standard deviation (SD). Using a paired t-test, we conducted a longitudinal analysis of each aspect of the POSAS, preoperatively and postoperatively. Statistical significance was set at p < 0.05.
3. Results
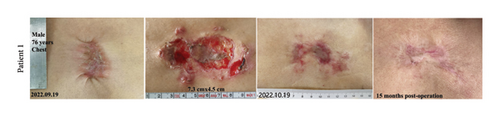
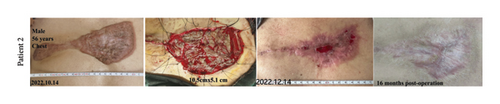
Seven patients were treated with a combination of ADM and a keloid-specific epidermal grafting method with an average follow-up period of 15.9 months (Figure 1). Significant improvements were observed, including a marked reduction in total POSAS scores from 91.1 ± 5.6 at pretreatment to 23.8 ± 6.1 posttreatment (p < 0.001) (Table 1). The patient and observer scores showed marked improvements in pain, pruritus, color, stiffness, thickness, and irregularity, with complete epithelialization achieved within four weeks post-excision. Notably, there have been no reported cases of bleeding, infection, or cellulitis to date.
| No. | Sex | Age (years) | Wound site | Approximate area (cm2) the longest × the widest | Observation time (months) |
|---|---|---|---|---|---|
| 1 | Male | 38 | Abdomen | 10 × 4.8 | 8 |
| 2 | Male | 37 | Abdomen | 3.6 × 2.3 | 27 |
| 3 | Male | 24 | Chest | 5.4 × 3.8 | 16 |
| 4 | Male | 76 | Chest | 7.3 × 4.5 | 15 |
| 5 | Female | 31 | Shoulder | 6.1 × 3.9 | 12 |
| 6 | Male | 24 | Chest | 9.3 × 5.5 | 17 |
| 4.3 × 2.4 | |||||
| 7 | Male | 56 | Chest | 10.5 × 5.1 | 16 |
The ADM scaffold significantly improved through neovascularization and extracellular matrix deposition, leading to an improved scar appearance with minimal hypertrophic growth or widening. However, the treated scars appeared primarily white compared to the surrounding skin. Continuous follow-up is recommended to monitor any localized elevations within the reconstructed areas observed to be nonproliferative and soft.
4. Discussion
Keloids have aggressive tumor-like characteristics and continually increase in size [9]. For large keloids in areas of high tension, a traditional surgical removal or skin flap transfer is not the optimal choice. This novel approach combining ADM with keloid epidermal skin grafting has created new modalities for the management of keloid scarring. By addressing the underlying source of this problem, the wound healing response induced by high-tension treatment may lower the chance of recurrence [10]. This is a significant improvement over traditional treatments because it avoids secondary injuries by preventing tissue harvest from other areas [11].
The use of ADM as a scaffold supports the grafted skin, assists with neovascularization, and helps in modulating the healing process [12]. The excision of the original keloid tissue removes inflammatory cells and abnormally active dermal fibroblasts; therefore, the graft minimizes both primary and secondary contractions on the underlying wound bed, promoting tension-free wound healing [13]. Controlling the healing environment may suppress the overactive inflammatory response and abnormal fibroblast proliferation observed during keloid formation. The component of wound healing modulation separates this method from other conventional methods. In addition, the application of epidermal skin grafting with the patient’s keloid epidermis reduces donor site morbidity and contributes to esthetic improvement and reduction in recurrence rates. This is crucial due to the significant psychosocial impact of keloids, stemming from their visible and often distressing appearance.
The integration of ADM and epidermal skin grafting is promising; however, the combination of this approach with existing treatment options is important. The application of LCR after ADM is important for optimizing treatment outcomes for keloid scars. ADM provides a robust scaffold that promotes tissue regeneration and reduces mechanical tension, while LCR enhances this process by further modulating the wound healing environment. The fractional CO2 laser creates microthermal zones that assist in remodeling collagen, which helps with tissue responsiveness to subsequent radiotherapy. This dual mechanism of ablative laser therapy and targeted radiation helps minimize abnormal residual fibroblast activity, thereby significantly reducing the risk of keloid recurrence. Therefore, the integration of LCR and ADM is a comprehensive approach that addresses the structural integrity of the repair and provides a targeted intervention to prevent the recurrence of keloids, leading to superior long-term outcomes for patients.
It is plausible that the best outcomes for certain patients may be achieved through an individualized approach combining this method with traditional treatments. Hence, exploring the potential of complementary strategies is another avenue for future research. As with any new therapeutic approach, affordability is crucial. While ADM and skin grafting might be more expensive than some traditional therapies, their ability to reduce recurrence makes them more cost-effective in the long run. However, a comprehensive cost-benefit analysis is necessary to confirm this hypothesis. In addition, a key limitation of this study is the absence of a control group without laser and radiotherapy, which limits our ability to isolate the specific effects of these treatments on keloid recurrence.
In summary, the combination of ADM and keloid epidermal skin grafting introduces a novel approach to keloid management. This represents a paradigm shift from symptom management to addressing the basis of the condition. Early results are promising; however, comprehensive research is required to validate these findings and optimize treatments for broader use. This innovative treatment modality offers possibilities for improving our understanding of wound healing and may impact the treatment of other scarring conditions.
Ethics Statement
All procedures were performed according to the principles of the Declaration of Helsinki. The IRB approval number is SH9H-2024-T275-1.
Consent
Informed consent was obtained from all the participants included in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Wenbo Wang and Boya Zhou contributed equally to this study.
Funding
This study received no grants from funding agencies in the public, commercial, or not-for-profit sectors.
Open Research
Data Availability Statement
All data generated or analyzed during this study are included in this article.




