The Physiological Impacts of the Low- and Moderate-Volume-HIIT with or without Nano-Curcumin Supplement in Women in Menopause with Obesity
Abstract
Tabata exercise has been proposed as an extremely time-efficient high-intensity interval training (HIIT) method to achieve health benefits, but direct comparisons between the low-volume-HIIT (LV-HIIT), moderate-volume-HIIT (MV-HIIT) with and without nano-curcumin (NaC) supplement for 8-week on cardiovascular hemodynamic, respiratory function, muscular fitness, and physical performance in the obese menopause women are limited. In a double blind, randomized, placebo-controlled study, 53, moderately obese menopause women (average age 45–60 yrs, BMI > 30 kg/m2, WC for >85 cm, and body fat > 35%) were randomly assigned to undertake either LV-HIIT, MV-HIIT, or NaC supplement (daily 80 mg in two 40-mg capsules) for two sessions per week for 8 weeks. The maximal exercise testing after 8-week of the LV-HIIT and MV-HIIT interventions caused significantly increase in the VO2max (mean difference: 6.83 (95% CI: 25.58–43.51), p = 0.01, mean difference: 5.31 (95% CI: 23.98–39.02), p = 0.028), and oxygen pulse (mean difference: 0.02 (95% CI: 0.16–0.19), p = 0.04, mean difference: 0.04 (95% CI: 0.17–0.21), p = 0.02), respectively. Moreover, MV-HIIT with and without NaC had significant improve in muscular fitness and physical performance (hand grip in MV + NaC (mean difference: 3.8 (95% CI: 21.46–31.81), p = 0.02), quadriceps strength in MV (mean difference: 14.58 (95% CI: 52.75–69.82), p = 0.01), MQI (mean difference: 31.23 (95% CI: 112.67–197.15), p = 0.02, mean difference: 31.52 (95% CI: 159.13–184.07), p = 0.01), sit to stand test (mean difference: 1.84 (95% CI: 6.60–8.41), p = 0.02, mean difference: 1.78 (95% CI: 6.69–9.03), p = 0.01), and the running distance (mean difference: 96.95 (95% CI: 470.05–637.42), p = 0.02, mean difference: 114.53 (95% CI: 458–641.87), p = 0.02)), when compared to baseline. In compared with the LV-HIIT groups, the MV-HIIT could improve FVC (mean difference: 0.12 (95% CI: 2.21–3.26)). Our data demonstrated that both the LV-HIIT and MV-HIIT, as part of activities of daily living, maybe a time-efficient strategy to improve cardiorespiratory fitness and physical performance. Beyond the purported health benefits, the MV-HIIT with and without NaC supplement appears to be safe approach in the previously sedentary obese menopause women.
1. Introduction
Over the past decades, overweight and obesity have dramatically increased all over the world, to an extent that almost one-third of the world’s population is now classified as overweight or obese. It is associated with a chronic low-grade inflammation that might represent the main risk factor for several chronic diseases, including type 2 diabetes, cardiovascular disease, some types of cancer, and psychological disorders [1, 2, 3], all of which have an adverse impact on quality of life, work productivity, and health care costs. There is accumulating evidence that sedentary lifestyle and obesity are bidirectionally related, and the WHO’s global plan on physical activity 2018–2030 has set a target of reducing sedentary lifestyle by 10% by the year 2025 and by 15% by the year 2030 [4]. Additionally, menopausal status is associated with a natural decline in estrogen that increases visceral fat mass, decreases bone mass density, muscle mass, and strength, and also, changes in some biological factors, such as oxidative stress, inflammation, estrogen, and other hormone deficiency [5]. Several lifestyle potential strategies have been proposed to tackle overweight and obesity, including regular exercise training, restriction of energy intake, and using nonpharmacological approaches [4, 6].
While regular physical activity has been observed to play a pivotal role in cardiorespiratory health and the negative consequences of a sedentary lifestyle, most obese people are not meeting the recommended levels of moderate exercise 30–60 min per day (≥5 days per week), or vigorous exercise 20–60 min per day (≥3 days per week), or a combination of moderate and vigorous exercise per day (≥3−5 days per week) [7]. It has been widely proven that regular exercise has a positive effect on cardiorespiratory fitness and fat loss [8]. Traditionally, in most exercise prescriptions, continuous exercises with high volume are the first choice and have been recommended to improve cardiorespiratory health and fat loss [8]. However, in order to achieve such a benefit related to cardiorespiratory health, high volume-continuous exercises need to be maintained for a long time [8]. In other words, one of the reasons why overweight and obese people cannot maintain a physically active lifestyle is lack of time [8, 9]. In recent decades, well-known high intensity interval training (HIIT) protocol has been prescribed as a more time-efficient and attractive alternative exercise option than relative to traditionally higher volume continuous training in cardiorespiratory fitness and weight loss programs [7, 9, 10]. Several studies conducted over the past two decades have demonstrated that HIIT can induce similar or even higher improvements in cardiorespiratory fitness relative to traditional continuous exercises, despite substantially lower training volume and time commitment [8, 9, 10, 11]. Moreover, studies have found HIIT has excellent benefits, including considerable increases in VO2max and insulin sensitivity [12, 13]. Eather et al. [13] evaluated the effect of an 8-week HIIT program, which included a variety of aerobic and muscular fitness exercise combinations lasting 8–12 min (using 30 : 30 s rest : work intervals) on cardiorespiratory and muscular fitness and body composition in university students and reported a significant increase in cardiorespiratory and muscular fitness. No significant intervention effects were found for body composition. Similarly, in a recent meta-analysis, Wen et al. [14] reported that HIIT protocols with short intervals (≤30 s), low volume (≤5 min) and short-term (≤4 weeks) were all effective in increasing cardiorespiratory. In contrast, recent evidence showed fat accumulation in the abdominal wall in obese individuals, leading to significant changes in ventilation and, therefore, spirometry test reveals a typical restrictive respiratory response, with a reduction in the pulmonary volumes [15]. However, far less is known about the efficacy of low-volume versus high-volume-HIIT approaches to improve cardiovascular, muscular fitness, and body performance, and the pulmonary function alterations in obese women and outcomes are controversial.
Taking herbal supplements may be a useful potential strategy for managing overweight and obesity and related diseases, such as metabolic syndrome [16, 17, 18]. Curcumin a bioactive compound and polyphenol found in the Curcuma longa plant, with low toxicity and without considerable adverse effects, which exerts antioxidant, anti-inflammatory, anticarcinogenic, anticoagulant, and cytoprotective, antiapoptotic, antidiabetic, antiarthritic, and antianxiety properties and cardioprotective activity in diabetic cardiomyopathy, and benefit for chronic diseases, such as the inflammatory, pulmonary, cardiovascular diseases, and metabolic syndrome disorders [19, 20, 21]. Also, it has anti-inflammatory, antioxidant, wound healing, antimicrobial activity [16, 17], and metabolic functions, such as improving insulin resistance [18]. Despite health benefits of curcumin, its low stability, bioavailability [18], insolubility, low tissue distribution and uptake, low action, rapid metabolism, and inactivation of products in the body impact its therapeutic efficiency [17]. Various techniques have been explored recently to improve this problem by using polymeric nanoparticles called nano-curcumin (NaC), which can increase curcumin bioavailability 22-fold [18]. Ashtary-Larky et al. [22] reported that NaC supplementation may decrease cardiovascular disease risk by improving glycemic and lipid profiles, inflammation, and SBP. Many studies revealed over the past decades in order to examine the effects of HIIT exercises in men and or athletes, while there are well-recognized sex differences in physiological systems at rest and in responses to exercise, and findings observed in men may not be translatable to women [11]. In addition, most studies have explored the effects of HIIT training [7, 9, 10] or NaC supplementation [16, 17, 18] separately on the cardiovascular hemodynamic, pulmonary function, muscular fitness, and body performance. However, few studies have been done on the simultaneous impacts of NaC and HIIT on these factors. We identify gaps in our understanding of physiologic benefits to the low-volume versus high-volume-HIIT training with and or without NaC supplementation in obese women and provide recommendations for how to advance the field in this regard.
To the best of our knowledge, while there is evidence demonstrate HIIT exercise is more benefit for decrease in abdominal obesity and cardiovascular fitness than traditional endurance exercise (i.e., MICT) for various age groups, there is still no consensus on whether low-volume-HIIT is as effective as or more effective than moderate-volume-HIIT, in terms of the cardiovascular hemodynamic, pulmonary function, muscular fitness, and body performance in the obese menopause women. We examine whether changes in the aforesaid indices following low- and moderate-volume-HIIT interventions had greater improvements, when obese women taking NaC supplement. We hypothesize that moderate-volume-HIIT together with NaC supplementation has a reinforcing effect on the cardiorespiratory health and muscular fitness. As a result, the main goal of the present study was to determine which nonpharmacological approach (8-week low-volume- vs. moderate-volume-HIIT with or without NaC supplementation) had a greater effect on the cardiovascular hemodynamic, pulmonary function, muscular fitness, and body performance in the obese menopause women aged 40–60 years, who previously ran sedentary lifestyle?
2. Materials and Methods
2.1. Study Strategy
2.1.1. Study Procedures Design and Ethical Considerations
This study was conducted from September 2021 to February 2022 throughout the time of COVID-19 disease. This experimentation was planned as a double blind, randomized, and placebo-controlled trial. The present study was designed as maintained by the Helsinki Declaration of 1975 as revised in 2013 and received approval from the local institutional ethics committee (Ethical code: IR.UMZ.REC.1401.008). Before the onset of study procedures, participants had been fully familiarized about the aims and procedures of the study, protocols, and equipment detail which conformed to the aforesaid Helsinki Declaration. Then, all participants provided written consent. They were allowed to withdraw from the study at any time, and no personally identifiable information was disclosed.
2.1.2. Participants and Eligibility Criteria
Moderately obese women with an average age 45–60 years, BMI > 30 kg/m2, waist circumference > 85 cm, or body fat > 35%, through advertisements in the local information system and cyberspace were recruited. The classification of obese based on BMI was determined using the WHO international criteria, where a BMI ≥ 30 kg/m2 is considered obese [23]. In addition, given to the reports of the previous researchers [24, 25, 26, 27], central obesity and obesity were defined using cutoff points for Asians as waist circumference (WC) for males >90 cm and females >80 cm; therefore, in the present study, moderately women with central obesity (BMI > 30 kg/m2, WC for >85 cm and body fat > 35%) were invited. The subjects’ dietary status was assessed evaluated using Nutritionist-4 software, which utilized gram per day values from the 24-hr food recall. During this, all participants were explicitly advised to maintain their existing dietary routines without modification.
All study women were screened for the inclusion eligibility criteria. The survey included questions about history of the menstrual period (present, irregular, or absent). Sedentary apparently without previous comorbidities women who had passed at least 1 year since the last menstrual period and had less than 30 min of moderate-intensity physical activity 3 days a week during the past 6 months were included in the present study [28]. Due to COVID-19 pandemic and to ensure women safety and to possibility unknown bias on outcomes, all participants with a positive COVID-19 diagnosis, even by one sign/symptom of acute respiratory disease was excluded from the study either before or during intervention. Further exclusion criteria are as follows: those below the threshold of 95% SPO2, women with a chronic disease who refrained from physical activity or currently under medication for any inflammatory and psychological diseases, individuals who completed less than 85% of the total exercise sessions, examinees who intake less than 85% of the curcumin supplement or allergy to curcumin. Moreover, participants with background of smoking or other tobacco consumption were excluded.
2.1.3. Participant’s Classification
A total of 137 inactive females in the Babolsar city (adjacent to our Athletic Performance and Health Research Centre by the Caspian Sea) volunteered to participate in this study. Then, according to the above criteria, eventually, 53 sedentary women in menopause but with obesity were randomly divided into six groups: placebo (Pla), with BMI; 30.41 ± 2.56 kg/m2, body fat percentage of 38.03 ± 4.78, WHR; 94 ± 6.37, NaC, with BMI; 32.55 ± 5.15 kg/m2, body fat percentage; 40.12 ± 5.06, WHR; 95.33 ± 11.39, low volume-high intensity interval training (LV-HIIT), with BMI; 30.53 ± 4.04 kg/m2, body fat percentage; 40.14 ± 3.09, WHR; 90 ± 4.40, moderate volume-high intensity interval training (MV-HIIT), with BMI; 30.36 ± 3.66 kg/m2, body fat percentage; 38.79 ± 3.70, WHR; 86.86 ± 9.26, NaC + low volume-high intensity interval training (NaC + LV-HIIT), with BMI; 30.19 ± 3.25 kg/m2, body fat percentage; 39.33 ± 4.02, WHR; 89 ± 6.88, and NaC + moderate volume-high intensity interval training (NaC + MV-HIIT), with BMI; 29 ± 1.68 kg/m2, body fat percentage; 39.50 ± 3.51, WHR; 86 ± 5.68, groups. The subjects in the NaC, NaC + LV-HIIT, and NaC + MV-HIIT groups ingested two NaC (40 mg) capsules per day (80 mg/day) in the course of 8 weeks. Likewise, women in the Pla and Pla + HIIT groups received two placebo capsules every day.
2.1.4. Sample Size Calculation
The sample size calculation was conducted with GPower 3.1® (version 3.1.9.2; Heinrich Heine University, Düsseldorf, Germany). The minimum sample size was seven subjects per group. Considering a loss to follow-up of 20%, we obtained a minimum sample size of eight patients per group. To estimate the sample size, we calculated the effect size based on previous studies. Considering an effect size of f-value 0.4 [29], an Wilcoxon test was performed within group for baseline and 8th week with a power of 0.80% and 95% confidence interval (p < 0.05).
2.1.5. Nano-Curcumin (NaC) Supplementation
The formulation of NaC supplementation was informed by the outcomes of prior research studies [18]. According to analysis by the high-performance liquid chromatography method, NaC capsules in this study contain 85% curcuminoids including curcumin, demethoxycurcumin, and bisdemethoxycurcumin, which was developed by the Nanotechnology Research Center of Mashhad University of Medical Sciences and has been registered under IRC number 1228225765. The NaC and placebo capsules were purchased by the Exir Nano Sina Company. The sinacurcumin® dose was 80 mg/day (two 40-mg capsules per day, according to the manufacturer’s instructions: one capsule at breakfast and another at dinner). The supplements were distributed once every 2 weeks, and consumption status was assessed daily and weekly by phone. Hence, each participant in the NaC supplementation, NaC + LV-HIIT and NaC + MV-HIIT groups received the NaC capsules. Likewise, subjects in the Pla and Pla + HIIT received two placebo capsules per day, which were similar in shape, color, and size and made of an equivalent dose of starch.
2.1.6. MV-HIIT versus LV-HIIT Exercise Training Programs
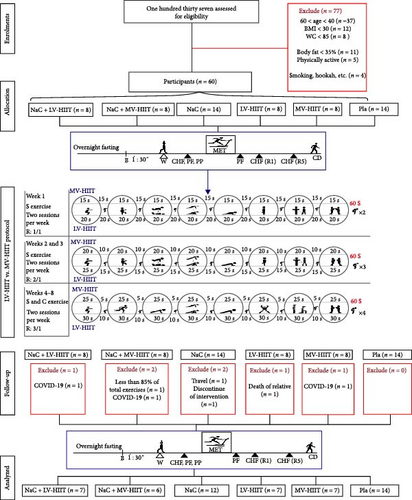
The exercise training program, which follows the principle of progressively increasing intensity based on body weight, has been derived from prior research with some minor adjustments including raising the number of sets, enhancing exercise complexity, and refining the use of the rating of perceived exertion (RPE) scale [30]. In summary, the LV-HIIT exercise program was performed with eight sequences in a series of 20 s of work and 20 s of rest (ratio 1/1) for each set was 5 min. The duration of each exercise movement was 20 s for the first week, 25 s for the second and third weeks, and 30 s for the fourth week. The MV-HIIT protocol was designed identically, with the exception that participants were asked to perform exercises with eight sequences in a series of 20 s of work and 10 s of rest (ratio 1/1) for each set was 4 min. The duration of each exercise movement was 15 s for the first week, 20 s for the second and third weeks, and 25 s for the fourth week. The details of the MV-HIIT and LV-HIIT exercise programs were explained to all participants in the preliminary. Furthermore, during practice sessions, their movements were monitored by a specialized professional throughout the 8 weeks and participants took feedback based on RPE scale to determine the intensity. An overview of both volumes HIIT exercise protocol is shown in Figure 1.
The exercise selection aimed to engage nearly all major muscle groups in every training session. Throughout the initial 4 weeks, the exercises were straightforward and aligned with sequence 8. Each set comprised eight exercises: air squats, high knee, push up to knee, mountain climber, standard plank, butt kickers, split, and skater. After the subjects’ fitness improved from baseline and in order to strengthen the same muscle groups, more complex exercises were selected for the second 4 weeks, including squat jump, skier jumping jack, push-up, mountain climber, super plank, jumping jack, lunge, and skater jump. The exercise intensity was determined by estimating the maximal heart rate (calculated as 220 minus age) and varied within the range of about 80%–90% of the maximum heart rate (~170–180 bpm).
2.1.7. The Maximal Exercise Testing (MET)
Experimental procedures were explained to all participants prior to the maximal exercise testing (MET), as previously documented in other sources [31]. In summary, MET protocol was performed on the percentage of maximum HR that was previously piloted on a separate visit and prior to the actual experiment. During MET and recovery three to 5 min following exercise termination, the operator continuously monitored the participant’s condition. Exercise electrocardiography was concluded once participants’ heart rate reached 80%–90% of the predicted maximum HR. Other criteria for terminating MET were based on the 2002 update of the American College of Cardiology and American Heart Association guidelines for MET [32].
2.2. Health and Physical Performance Examinations
2.2.1. Cardiovascular Hemodynamic
For each examination, subjects were asked to arrive to refrain from alcohol and intensive physical activity in the preceding 24 hr. Information was gathered under standard environmental conditions (temperature: 24−26°C; barometric pressure: 760 mmHg, and relative humidity of 50%–60%). Cardiovascular hemodynamic and respiratory function assessments were made at four stages, including baseline and immediately after the maximal exercise testing both before and after 8 weeks of the low- and moderate-volume-HIIT exercise and/or NaC supplementation interventions.
At the starting and finishing of the study, blood oxygen saturation (SpO2) measurements were conducted utilizing a wearable finger pulse oximeter (Brisk, Model PO16, China). Participants were received instructions to wear the pulse oximeter on the index finger of their nondominant hand. Moreover, heart rate (HR), systolic blood pressure (SBP) and diastolic blood pressure diastolic (DBP) were continuously monitored using a 12-lead electrocardiogram (custo med GmbH, 2000, XP, Vista Leibnizstr. 7. 85,521 Ottobrunn, Germany). To determine myocardial oxygen consumption (MVO2), we used the following formula: MVO2 = HR × SBP. Furthermore, VO2max was conducted by the maximal testing protocol. Besides entering age and gender, heart rate, and blood pressure information were controlled through the device. The maximal testing protocol continues until the person’s maximum oxygen consumption until reaching the plateau becomes evident, and at this time, the device automatically begins to calculate Vo2max. Following identifying the oxygen consumption, the oxygen pulses have been calculated by oxygen pulse (ml/beat) = Vo2/heart rate ratio formula based on formula in Wasserman et al.‘s [33] study.
2.2.2. Respiratory Function
Forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), forced expiratory flow (FEF), and peak expiratory flow (PEF) were measured with spirometer system (Spirolab III Colour, Italy) according to the standards specified by the European Respiratory Society [34]. Respiratory function measurements were made in a relaxed seated position with the subjects’ noses closed with a latch. Each measurement was made twice, and the device’s best value was recorded. All assessments were made at four stages, including prior to and following the MET protocol [35] in the pre and post of the 8 weeks of the moderate or low-volume-HIIT exercise and/or NaC supplementation interventions.
2.2.3. Physical Performance
Decline of muscle strength is considered the main predictors of functional capacity decrease as well as loss of independence in older age. The two validated tests assessed to estimate muscle function were previously described in Buckinx et al. [36] The quadriceps muscle strength was assessed using a dynamometer, positioned precisely near the ankle on the front surface of the leg. The participant’s elbows and legs were extended straight. Next, lean their trunk forward by 30°, with hands in parallel and grasping the chain handle placed in front of the body with both hands. From this position, the examinees were forced on the handle to attempting straighten their trunk and hold for 3–4 s. Also, a manual dynamometer with an adjustable grip was used to measure the maximum voluntary strength of forearm and finger (handgrip). Women were standing straight with the arm along the side of the body with the extended elbow and the palm facing the thigh and squeezing the hand dynamometer as hard as possible for up to 4 s. This test was repeated three times, and the highest recorded on the screen of the device was considered as the personal record [37].
Skeletal muscle mass index (SMMI) determined by body composition analyzer system (Medigate Inc., BoCA x1, Korea). We assess MQI by ((L − 0.5) × body mass × g × 5)/Tsit-to-stand formula, L mean leg length which calculated from the inguinal crest to the patella along the midline of the thigh + heel of the leg to the anterior surface of the thigh, above the condyles of the femur (while, the legs hanged and a sliding caliper placed under the heel of the leg), body mass was determined by body composition, g represent acceleration due to gravity (9.8 m/s2), T is the height of the chair (43 cm), after all, sit to stand is the time taken to perform the sit-to-stand test by each participant by using a stopwatch to record the time it took for them to since initiated upon verbal instruction of the term “go” and concluded when the participant’s buttocks made contact with the chair’s seat after the completion of the fifth stand [38], starting from a seated position and returning to sitting again without use their arms during the test [39]. Also, we provided a demonstration of the accurate procedure for executing the test, encompassing achieving a fully upright stance, defined as the alignment of hips and knees while standing [38]. Finally, both distance and Borg were measured by the maximal exercise testing. The Borg RPE scale ranges from 0 (nothing at all) to 10 (extremely strong) and was used in this study [40, 41].
2.3. Data Analysis
All statistical analyses were performed with SPSS software (version 26.0 for Windows, IBM, Armonk, NY, USA). The Shapiro–Wilk’s test was used to assess distribution characteristics. A Friedman’s test was used to detect within-group differences (pre-MET, 1-min recovery (1R), and 5-min recovery (5R) of 8th week) for all hemodynamic parameters among groups. For both physical performance and respiratory parameters, within-group comparisons were conducted using a Wilcoxon matched pairs test. All pairwise comparisons were corrected for multiple tests using Bonferroni corrections. Also, for between-groups comparisons of all respiratory, hemodynamic, and physical performance parameters, a Kruskal–Wallis’s test with Mann–Whitney U tests for pairwise comparisons were conducted.
3. Results
After excluding the incomplete data from a sample of 137, 53 of the moderately obese menopause women were included in the final data analysis.
3.1. Effects of the LV-HIIT, MV-HIIT, and NaC Supplement on Pulmonary Function
The results of the pulmonary function parameters such as forced vital capacity (FEV), forced expiratory volume in 1 s (FEV1), forced expiratory flow (PEFR), and peak expiratory flow rate in the before and after the maximal exercise testing (pre-MET and post-MET) in baseline and 8th week of the low-volume-HIIT (LV-HIIT) and moderate-volume-HIIT (MV-HIIT) exercise training and/or NaC supplement interventions in the obese menopause women are shown in Figure 2.
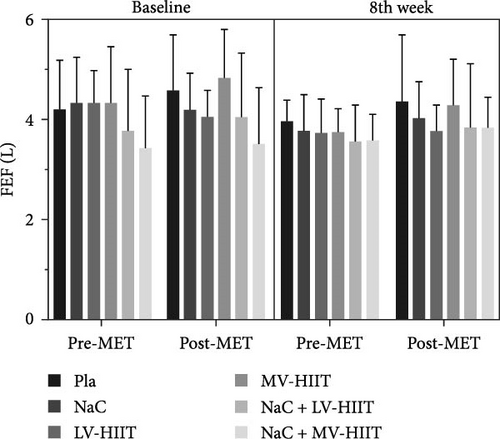
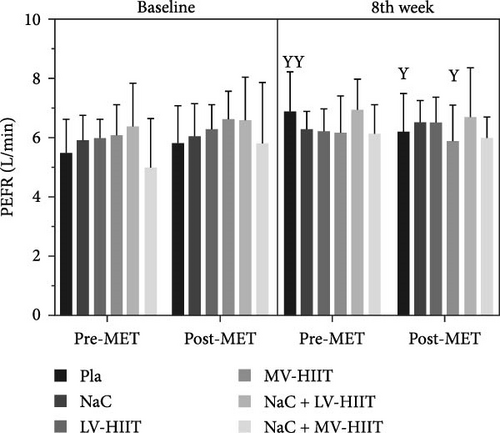
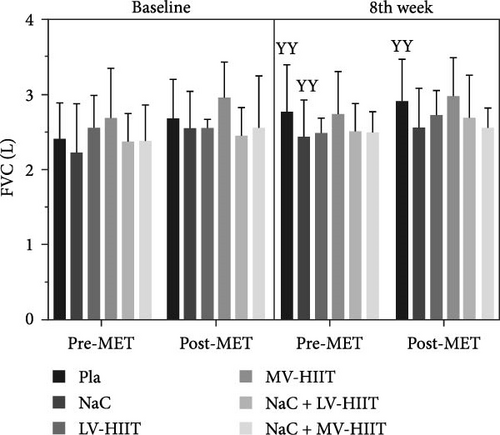
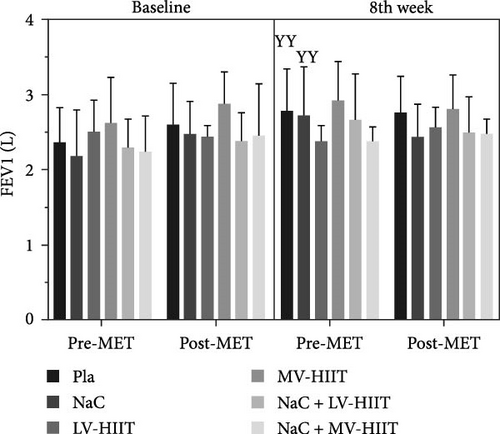
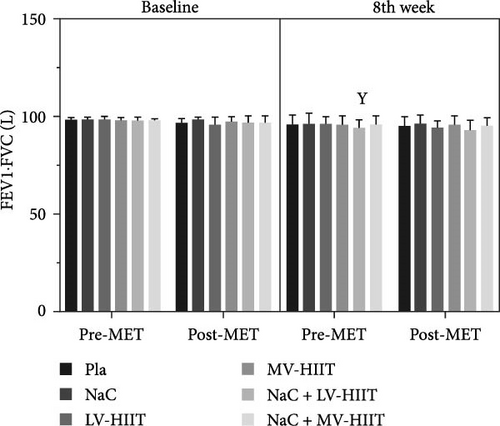
At rest status, there was no statistically significant difference in pulmonary function parameters between pre and post 8 weeks LV-HIIT and MV-HIIT exercise training interventions. However, following the maximal exercise testing in 8th week of NaC intervention, only FEV1 (p < 0.049, effect size = 0.57) and FVC (p < 0.005, effect size = 0.82) significantly increased by 20% and 11%, when compared to similar status in the baseline. Following maximal exercise testing (both pre-MET and post-MET status), the FVC, FEV1, PEFR, and peak expiratory flow rate parameters indicated a slightly increase in the obese menopause women. However, following adaptation to 8 weeks of interval training with different volumes, a significant increase in FVC values (p < 0.001, effect size = 0.54) was observed in both training groups, especially in the MV-HIIT group, when compared with baseline values. In other words, the extent of increase in FVC values following 8 weeks of intervention was significantly greater in the MV-HIIT group than in the LV-HIIT group (p < 0.026, effect size = 0.41). Although workload in post-MET after 8-week interventions was higher than baseline status, no statistically significant differences in the aforesaid parameters were found between the groups, when compared to pre-MET and before 8-week interventions.
3.2. Effects of the LV-HIIT, MV-HIIT, and NaC Supplement on Cardiovascular Hemodynamic Function
The resting levels of cardiovascular hemodynamic function parameters obtained in before none-pharmacological interventions were not significantly different between the groups. As we can see in Figure 3, following the maximal exercise testing, MVO2 values (i.e., HR × SBP) were climbed sharply until 1-min recovery (1R) (p < 0.001, effect size = 0.26), in comparison to baseline levels in the both before and 8th week periods, then dropped during 5-min recovery (5R), but not as less as the level of baseline. Following 8 weeks of LV-HIIT versus MV-HIIT with and without NaC supplement, the extent of increase in MVO2 (as biomarker related to the coronary artery blood flow and the typical antianginal agent) after the maximal exercise testing was significantly higher in the combined groups than in the placebo, LV-HIIT and/or MV-HIIT groups (p < 0.001, effect size = 0.58).
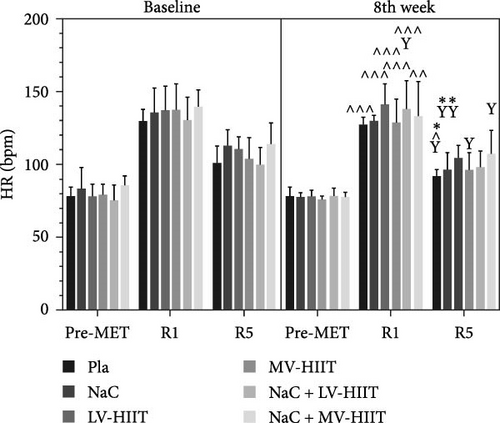
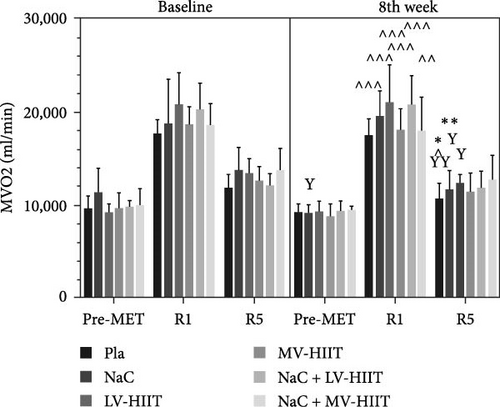
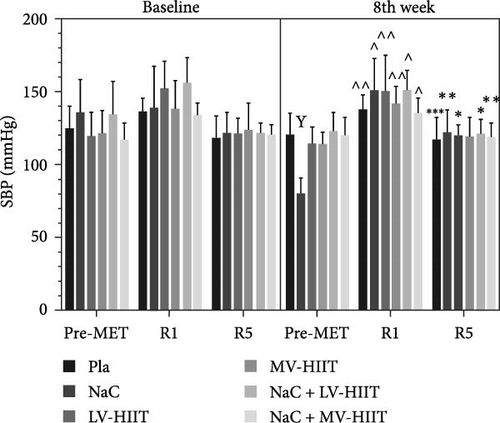
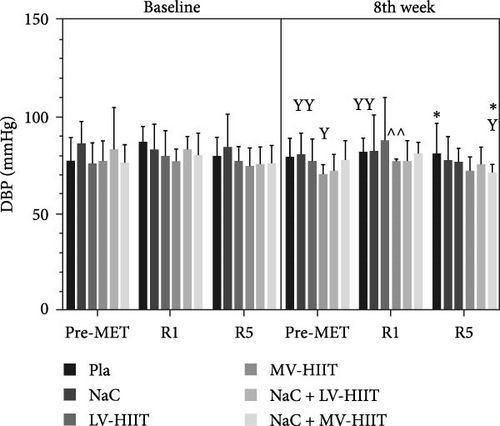
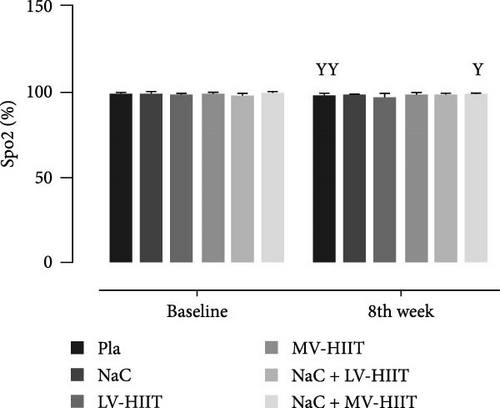
Following an 8-week adaptation to moderate- and low-volume training, despite the significantly increase the running distance reached (p < 0.001, effect size = 0.74) during the maximal exercise testing (MET) (Figure 4), there was a significant decrease in heart rate (HR) during the 1-min post-test recovery (1R) after MET protocol (p < 0.001, effect size = 0.26) and this significantly decrease after 5 min of recovery (5R) (p < 0.001, effect size = 0.14), only in the MV-HIIT with and without NaC supplement groups was more obvious, when compared with baseline period (Figure 3). In the all groups, neither exercise volumes (LV-HIIT versus MV-HIIT) nor supplementation caused changes in the SPO2 and DBP levels, with exception for NaC + LV-HIIT (Figure 3).
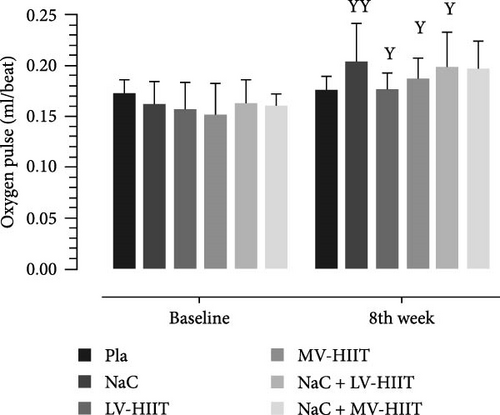
The oxygen pulse values in the obese menopause women supplemented with NaC for 8 weeks were not significantly different from that recorded at baseline. However, following adaptation to 8 weeks of LV-HIIT versus MV-HIIT with and without NaC supplement, a significant increase (p < 0.001, effect size = 0.67) was detected in oxygen pulse, as compared to the control group. These changes were completely consistent with the increase in VO2max (p < 0.001, effect size = 0.73) (Figure 4).
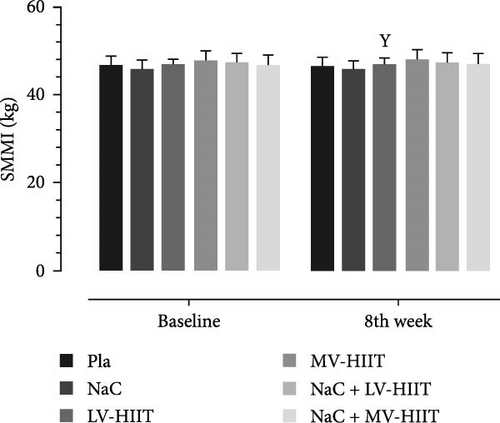
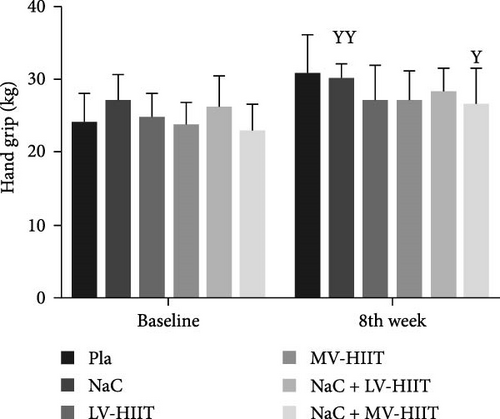
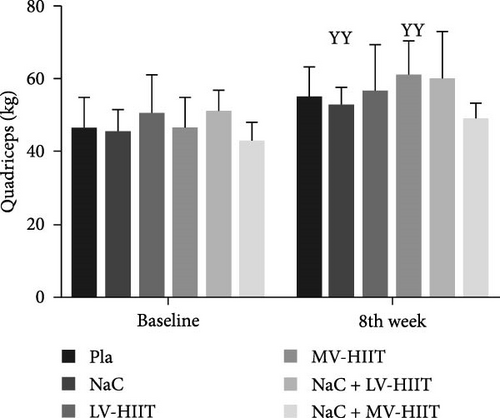
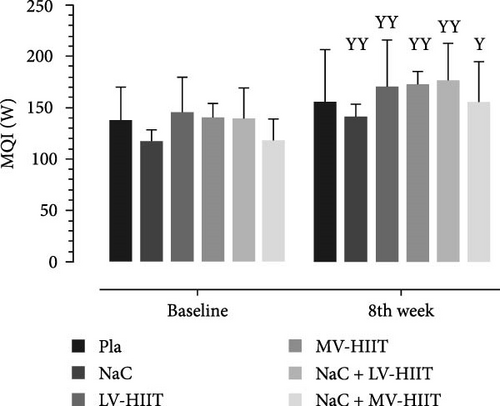
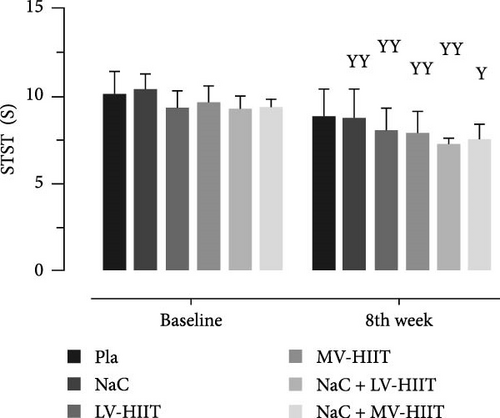
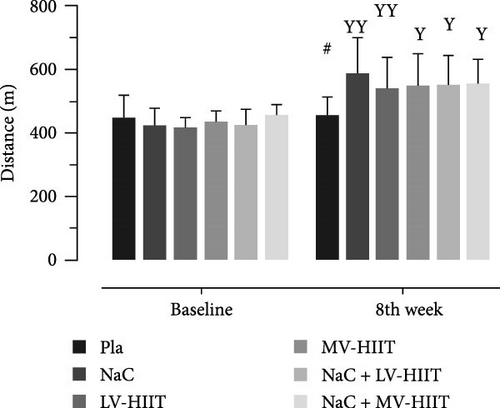
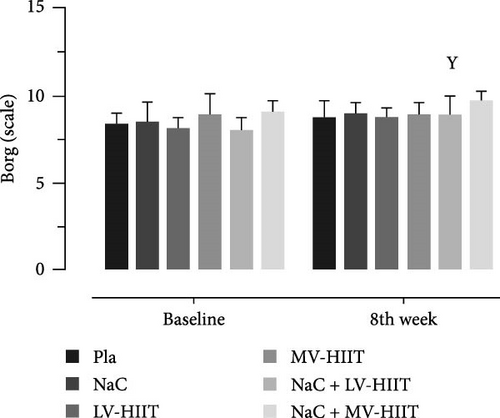
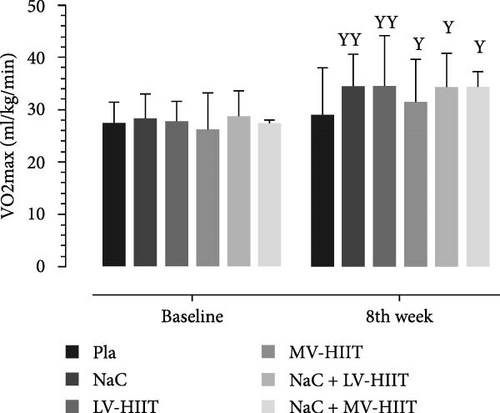
3.3. Effects of the LV-HIIT, MV-HIIT, and NaC Supplement on Physical Performance
Figure 4 shows that the 8-week interventions significantly increased the running distance reached (p < 0.001, effect size = 0.74) during the maximal exercise testing (MET) (difference in average the prior and after interventions, equal to 124.75 ± 91.07, 114.53 ± 104.61, 161.93 ± 88.85, 124.75 ± 91.07, 96.95 ± 71.14, and 9.06 ± 66.66 m in the LV-HIIT, MV-HIIT, NaC, NaC + LV-HIIT, NaC + MV-HIIT, and placebo groups, respectively). In addition, following 8-week of the LV-HIIT, MV-HIIT interventions (alone or combined with NaC) levels of VO2max significantly improve (p < 0.001, effect size = 0.73) between the intervention groups and the placebo group (difference in average the prior and after interventions, equal to 6.8 ± 6.2, 5.3 ± 4.3, 6.1 ± 3.9, 5.8 ± 4.4, 6.9 ± 3.2, and 1.5 ± 6.0 ml/kg/min in the LV-HIIT, MV-HIIT, NaC, NaC + LV-HIIT, NaC + MV-HIIT, and placebo groups, respectively). Measurements at week 8 showed that physical performance improved in the intervention groups by insignificant increase in hand grip, quadriceps, MQI, and decrease in sit to stand test. However, both the LV and MV-HIIT interventions with and without NaC led to a statistically significantly improve in the skeletal muscle mass index (SMMI) (p < 0.05, effect size = 0.25), muscle quality index (MQI) (p < 0.001, effect size = 0.83) and sit to stand test (STST) (p < 0.001, effect size = 0.82) as compared to baseline values. Moreover, after 8-week of nonpharmacological interventions, a nonsignificantly increase was detected in the Borg RPE levels in the NaC and NaC + MV-HIIT, which indicates effectiveness the combination intervention of Nac and moderate volume-HIIT in improving tolerance of exercise load during the maximal exercise testing.
4. Discussion
Here we tested which nonpharmacological strategy (8-week low-volume-HIIT vs. moderate-volume-HIIT with or without NaC supplementation) had a greater effect on the cardiovascular hemodynamic, the pulmonary and physical function and body composition in the moderately obese menopause women. The most important findings of this study are as follows: (1) while the maximal exercise testing (MET) protocol led to a significant increase in MVO2 values (as an index of myocardial oxygenation), adaptation to 8 weeks of LV-HIIT versus MV-HIIT with NaC supplementation caused the increase in MVO2 after MET in the combined groups to be significantly higher than the placebo, LV-HIIT, or MV-HIIT groups. This valuable change occurred in conditions that an 8-week adaptation to moderate- and low-volume training, led to the significantly increase the running distance reached and decreased RPE, which in turn indicating effectiveness the combination intervention of Nac and moderate volume-HIIT in improving tolerance of exercise load during the maximal exercise testing (MET); (2) similarly, adaptation to the LV-HIIT versus MV-HIIT with and without NaC supplement for 8 weeks in the obese menopause women cause a statistically significant increase in oxygen pulse (as the ratio of O2 consumption to HR and expresses the volume of oxygen ejected from the ventricles with each myocardial pulse), which was completely consistent with the increase in VO2max; (3) while, the 8-week interventions significantly increased physical performance indices, such as hand grip, quadriceps strength, MQI, sit to stand test, and the running distance reached in the intervention groups, only the LV and MV-HIIT interventions with and without NaC led to a significant improve in the skeletal muscle mass index (SMMI); and (4) the maximal exercise testing (both baseline and 8th week), cause an increase in the FVC, FEV1, PEFR, and peak expiratory flow rate parameters in the obese menopause women. However, following adaptation to 8 weeks of interval training with different volumes, a significant increase in FVC values was detected in both training groups, when compared with baseline values and placebo group. The extent of increase in FVC values was significantly greater in the MV-HIIT group than in the LV-HIIT group.
In line with the findings of the present study, the results from recent studies showed that HIIT can induce similar and greater improvements in cardiovascular hemodynamic function, cardiovascular fitness and glucose control, when compared to more traditional forms of endurance training including moderate intensity continuous training (MICT), despite requiring less time commitment and lower energy expenditure [42]. An increase in MVO2 suggests increase in oxygenation to myocardial. It is encouraging to compare these findings with that reported by Nagpal et al. [43] who reported that percentage increase in MVO2 was significantly more in postmenopausal women following exercise. There are several possible explanations for these findings; initially, it can be argued physiologically that an increase in MVO2 could be due to a better coronary perfusion in which there will be a gain in myocardial oxygenation following regular exercise training [44]. It is generally believed that MVO2 alterations depend on several factors, such as VO2max, intraparietal tension, contractility or myocardial inotropism, heart rate, external cardiac work/the work accomplished during the ejection phase, the energy of electrical activation, and ventricular relaxation. Based on the results of the present study, it seems that improve in VO2max and decrease in the heart rate, intraparietal tension (related to decline in respiratory muscles work), myocardial contractility, external and internal cardiac work may explain the physiological impact of regular exercise on the increased MVO2 [45]. Previous studies in humans have reported that MVO2 is a strong predictor of exercise capacity, which in turn can predict peripheral muscle function [44]. Furthermore, humans have reported that oxygen pulse during exercise reflects the maximal aerobic capacity [46]. One of the earliest studies to examine the impact of low-volume-HIIT on cardiovascular health was undertaken by Tjønna et al. [47], in which subjects, who were without previous comorbidities overweight, were calcsilicate to either high-volume-HIIT (4 × 4-min at 90% heart rate maximum) or low-volume-HIIT (1 × 4-min at 90% heart rate maximum) three bouts per week for 10 weeks. Tjønna et al. [47] reported both the high-volume-HIIT and low-volume-HIIT trails increased cardiovascular fitness, blood pressure, and fasting blood glucose levels. However, both training protocols had little effect on body weight. Recently, Poon et al. [48] showed that although low-volume-HIIT led to similar enhancements in cardiovascular fitness in adult men with overweight and obesity, as compared to higher volume-MICT, neither protocol significantly improved blood pressure and glucose control. These findings could be a result of the effectiveness of HIIT and lifestyle on the respiratory, hemodynamic, cardiovascular, and muscular systems, which play a major role in improving physical performance and quality of life in the beginning of old age. In the current study, it was observed that 8 weeks of the LV-HIIT, MV-HIIT interventions (alone or combined with NaC) led to significantly improved VO2max between the intervention groups, when compared to placebo group. Further evaluations are required to determine the precise mechanisms of involve in cardiovascular fitness (VO2max) induced by regular HIIT including; improvements are linked to function and protein content of mitochondrial enzymes and insulin sensitivity, left ventricular ejection fraction as well as greater central and peripheral arterial compliance.
Another issue that was investigated in the study was the effect of 8 weeks of the nonpharmacological interventions on parameters related to muscle fitness and physical performance, such as sit to stand test (STST), muscle quality index (MQI), skeletal muscle mass index (SMMI), VO2max, and RPE in the obese menopause women. Findings from the present study show for the first time that combined training (i.e., the LV and MV-HIIT interventions with and without NaC) improved hand grip, quadriceps strength, MQI, sit to stand test, the running distance reached, and VO2max after 8 weeks of the nonpharmacological interventions. Previous evidences indicate loss of SMM is associated with persistent peripheral muscles weakness, reduced muscle strength, and impaired cardiac function that will limit the exercise performance capacity as well MVO2. Also, studies established a linear relationship between coronary blood flow and MVO2 [44]. Beyond the aforesaid purported cardiovascular advantages, it seems low-volume-HIIT had comparable results to high-volume-HIIT to improvements in the aforesaid indices and to be safe, beneficial, and well-tolerated in the overweight and obese adults, with low adverse impacts [42].
As expected, in the present study, it was observed that adaptation to 8 weeks of interval training with different volumes led to a significant increase in FVC values in both training groups, and the extent of increase in FVC values was significantly greater in the MV-HIIT group than in the LV-HIIT group. Such observations are important since they reveal that the pulmonary alterations induced by overweight and obesity can be attenuated by HIIT training, especially MV-HIIT exercise training. It seems that the increase in FVC following aerobic exercise is due to the increase in lung volume and the elastic return of the lungs. On the other hand, FVC is affected by the strength of the intercostal muscles. Therefore, improving the strength and endurance of the respiratory muscles also increases FVC, because the strength and endurance of the respiratory muscles increases due to the implementation of repeated aerobic exercises [15]. Interestingly, the combined interventions did not lead to a significant improvement in FEV1, PEFR and peak expiratory flow rate parameters in the obese menopause women, there was no significant effect on any of the respiratory parameters in obese postmenopausal women, which was consistent with previous studies results [15].
Another issue that was investigated in the current study was the effects of oral NaC supplementation alone or together with low-volume- and moderate-volume-HIIT training protocols. According to the obtained results, after 8 weeks of low-volume- and moderate-volume-HIIT and NaC treatment, we found a significant reduction in the RHR, SBP, DBP, and MVO2 in the obese menopause women of NaC group, as compared to placebo group. This reduction was more evident in the group that took the NaC supplement at the same time as moderate-value HIIT exercises than the other groups. Moreover, the effects of NaC + moderate-volume-HIIT intervention on improving respiratory function and cardiovascular hemodynamics were more evident than the separate effects of each of these interventions. Improved respiratory function and cardiovascular hemodynamics after NaC + moderate-volume-HIIT is consistent with previous studies [49]. The improvement in physical performance in our study cannot be exactly explained by changes in pulmonary function and is therefore likely due to other mechanisms. Ejection fraction (EF) has previously been shown to improve after HIIT exercise [49, 50], and the improvement found in our study to some extent may be a mechanism explaining the increased physical performance. Moreover, the anti-inflammatory effect of exercise training is a possible reason. It can be stated that regular training leads to an enhancement in lipoprotein lipase activity and the catabolism of cholesterol-rich lipoprotein and thus the negative hemodynamic pressure is reduced [19]. Findings of previous studies showed that most participants can engage in this type of exercise training protocol [8, 51, 52], as it has been performed without any cardiovascular adverse events in the overweight and obese women in the current study.
5. Limitations of the Study
Our study strengths were the successful blinding (placebo versus NaC supplement) of participants, and the high rate of compliance (all the obese menopause women reported that had taken capsules during 8 weeks). However, there are some potential limitations that should be acknowledged. First, this was a moderate-term trial, and it is unknown if longer periods of HIIT and supplementation (e.g., 12 weeks) could cause further improvements and it may effect the generalizability of the outcomes. Therefore, long-term curcumin supplementation with HIIT training is granted to establish the real impact. Second, only without previous comorbidities nonsmoker menopause women were included and therefore findings from this work cannot be generalized to clinical individuals like chronic obstructive pulmonary disease (COPD) and heart failure (HF). This is important given smoking can alter the cardiorespiratory hemodynamic and unmask the potential effects of regular exercise and NaC supplementation [53]. Third, our study was designed and performed during the SARS-CoV-2 pandemic. Therefore, the low number of postmenopausal women with specific research inclusion criteria during the pandemic is considered as a significant limitation. Therefore, by increasing the number of subjects in different groups, the external validity of more accurate findings can be increased. Fourth, while we attempted to recommend and aware of healthy and balanced diet to participates at first and during intervention, it was not completely under control. It could lead to potential biased and lies in several reasons, such as meals consumed outside the control may contain additives or personal preferences which can affect how strictly participants adhere to their overall nutrition intake that could affect health outcomes.
6. Conclusion
Our findings showed that while low-volume-HIIT had comparable results to moderate-volume-HIIT to improvements in the cardiovascular, moderate-volume-HIIT with and without NaC supplement offered greater benefits for muscular fitness and physical performance (hand grip, quadriceps strength, MQI, SMMI, RPE, sit to stand test, and the running distance), in the moderately obese menopause women. Furthermore, NaC alone has limited effectiveness on the pulmonary function and cardiovascular hemodynamic. However, tolerating the progressive overload during the maximal exercise testing (MET) protocol on cardiovascular system (as measured by MVO2, VO2max, and oxygen pulse indices) was better in those menopause women who were exposed to moderate-volume-HIIT training with NaC for 8 weeks. Therefore, in order to provide practical and universally applicable recommendations considering today’s busy lifestyle, we suggest incorporating 2 days of low-volume-HIIT workout per week, gradually increasing to moderate volume in addition to adding NaC supplement to daily routine to benefit from remarkable properties. Further studies involving long-term interventions (e.g., 12 weeks) are required to determine impact of the low- and moderate-volume-HIIT with and without the herbal inflammatory and antioxidant supplements on cardiorespiratory health in the older women and men.
Ethical Approval
The present study was designed as maintained by the Helsinki Declaration of 1975 as revised in 2013 and received approval by the University of Mazandaran Institution Ethics Committee (Ethical code: IR.UMZ.REC.1401.008). Before the onset of study procedures, participants have been fully familiarized with the aims and procedures of the study, protocols, and equipment detail which conformed to the aforesaid Helsinki Declaration.
Consent
All participants provided written consent. They were allowed to withdraw from the study at any time, and no personally identifiable information was disclosed.
Disclosure
The manuscript is only communicated to the journal, the manuscript will not be submitted elsewhere for review and publication.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Authors’ Contributions
Valiollah Dabidi Roshan contributed to research idea, conceptualization, writing—review and editing, supervision, and methodology. Sepideh Noorbakhsh contributed to writing and editing, creation of figures, data collection, and formal analysis. Seyedeh Fatemeh Ziatabar Ahmadi contributed to data collection. Mehdi Nikseresht contributed to methodology and data collection. All authors have read and agreed to the published version of the manuscript.
Open Research
Data Availability
All the data that support the findings of this study are available within the article.




