Risk Factors for Acute Kidney Injury after Moderate Hypothermic Circulatory Arrest in Hemiarch Replacement
Abstract
Background. The aim of this study was to clarify the incidence and risk factors for acute kidney injury (AKI) in patients undergoing hemiarch replacement (HAR) under moderate hypothermic circulatory arrest (MHCA) with retrograde cerebral perfusion (RCP). Methods. We retrospectively analyzed patients who underwent HAR under MHCA with RCP at our institution between April 2015 and July 2022. Exclusion criteria were preoperative dialysis, single kidney, and lack of preoperative plasma creatinine data. The study endpoint was the incidence of postoperative AKI, defined using the Kidney Disease: Improving Global Outcomes criteria. Multivariate logistic regression analysis was performed to identify the risk factors for postoperative AKI. Results. One hundred and seventy-nine patients were included in this study. The most common indications for HAR were thoracic aortic aneurysm (n = 107) and acute aortic dissection (n = 57). Concomitant procedures, most frequently aortic valve surgery, were performed in 104 (60.5%) patients. Median circulatory arrest time and minimum rectal temperature were 15 minutes (interquartile range, 11 to 19) and 27.4°C (interquartile range, 25.9 to 28.1), respectively. Operative mortality was 1.1%. The incidence of postoperative AKI was 37.8%. Multivariate analysis showed that acute aortic dissection (odds ratio, 4.57; 95% confidence interval (CI), 2.13–10.14; P < 0.001) and longer operating time (odds ratio, 1.01; 95% CI, 1.00-1.01; P = 0.001) were independent predictors for postoperative AKI. Conclusions. Acute aortic dissection and longer operating time were risk factors for postoperative AKI in patients undergoing HAR under MHCA with RCP. In contrast, neither circulatory arrest time nor minimum rectal temperature was a risk factor for AKI. This may be due to the short duration of circulatory arrest.
1. Introduction
Acute kidney injury (AKI) is a common complication of cardiovascular surgery and is associated with prolonged intensive care unit stay and increased perioperative mortality [1–3]. The incidence of AKI after thoracic aortic surgery is high compared with other cardiac surgeries. Previous reports found that the incidence of AKI after thoracic aortic surgery ranged from 17.7% to 54% [4–6]. Several risk factors were identified as predictors for postoperative AKI [7–9]. However, most of these studies included patients who had undergone total aortic arch replacement with branch reconstruction, requiring a relatively long circulatory arrest time. Although we exclusively used moderate hypothermic circulatory arrest (MHCA) with retrograde cerebral perfusion (RCP) when performing hemiarch replacement (HAR) without reconstruction of aortic arch branches, some of our patients developed postoperative AKI. Therefore, we hypothesized that the duration of MHCA or the patient’s core temperature during MHCA might influence the incidence of postoperative AKI.
The aim of this study was to investigate the risk factors for postoperative AKI after MHCA with RCP, focusing on circulatory arrest time and minimum rectal temperature, in patients undergoing HAR.
2. Patients and Methods
This retrospective observational study was approved by the institutional review board of the Kumamoto University Hospital and was conducted according to the principles of the Declaration of Helsinki. The requirement for informed consent was waived because of the retrospective nature of the study.
2.1. Patient Population
Between April 2015 and July 2022, 179 patients underwent HAR with or without a concomitant procedure under MHCA with RCP at Kumamoto University Hospital, Kumamoto, Japan. Of these, 172 (96.1%) patients were included in this retrospective study. The exclusion criteria were as follows: patients on preoperative hemodialysis (n = 3), those with a single kidney (n = 2), and those without postoperative serum creatinine data (n = 2). Patients’ preoperative characteristics are summarized in Table 1. The most common indications for HAR were thoracic aortic aneurysm (n = 107; 61.6%), acute type A aortic dissection (AAD, n = 57; 33.1%), and chronic aortic dissection (n = 7; 4.1%). Mean preoperative glomerular filtration rate was 63.3 ± 22.1 ml/min/1.73 m2. Ten patients (5.8%) had a history of previous cardiac surgery, and 8 of these 10 patients had undergone aortic valve replacement. We reviewed the preoperative, intraoperative, and postoperative data of the study patients and investigated the incidence and risk factors of postoperative AKI, especially focusing on circulatory arrest time and minimum rectal temperature.
| Age (years) | 70.7 ± 11.3 |
| Female | 83 (48.3%) |
| Body surface area (m2) | 1.58 ± 0.25 |
| Etiology | |
| Thoracic aortic aneurysm | 107 (61.6%) |
| Acute aortic dissection | 57 (33.1%) |
| Chronic aortic dissection | 7 (4.1%) |
| Aortitis | 1 (0.6%) |
| Prosthetic graft infection | 1 (0.6%) |
| Hypertension | 114 (66.3%) |
| Dyslipidemia | 46 (26.7%) |
| Diabetes mellitus | 23 (13.4%) |
| Smoking history | 77 (44.8%) |
| Coronary artery disease | 24 (14.0%) |
| Cerebrovascular disease | 28 (16.3%) |
| Left ventricular dysfunction | 11 (6.4%) |
| Peripheral arterial disease | 3 (1.7%) |
| Atrial fibrillation | 24 (14.0%) |
| eGFR (ml/min/1.73 m2) | 63.3 ± 22.1 |
| CKD stage | |
| G1 | 22 (12.8%) |
| G2 | 67 (39.0%) |
| G3a | 50 (29.1%) |
| G3b | 24 (14.0%) |
| G4 | 9 (5.2%) |
| Previous cardiac surgery | 10 (5.8%) |
| Nonelective surgery | 54 (31.4%) |
- CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate.
2.2. Surgical Procedures
All surgeries were performed via a median sternotomy. An arterial cannula was placed in the ascending aorta or femoral artery. At our institution, the axillary artery is not preferred because of the time required for exposure and there were no cases in which it was utilized in this study. After cardiopulmonary bypass (CPB) was instituted, patients were cooled to a rectal temperature of 25°C to 30°C for circulatory arrest. The target minimum rectal temperature depended on the surgeons’ discretion. After aortic cross-clamp, myocardial protection was established with a combination of antegrade and retrograde cold blood cardioplegia. The ascending aorta was transected approximately 1 cm distal to the sinotubular junction. In cases of AAD, the proximal aortic stump was repaired at the sinotubular junction using BioGlue Surgical Adhesive (CryoLife, GA, USA) and double felt strips [10]. In HAR, we used an open distal anastomosis technique with RCP using 12-Fr balloon catheter inserted into the snared superior vena cava (SVC). We perfused at a rate of 300 to 700 ml/min through the SVC, aiming to maintain central venous pressure of ≤25 mmHg. A near-infrared spectroscopy oximetry device (INVOS 5100C, Medtronic, Minneapolis, MN, USA) was used to monitor the regional cerebral oxygen saturation. The distal ascending aorta was transected just proximal to the bifurcation of the brachiocephalic artery. A single-branch vascular prosthesis (Triplex; Vascutek, Terumo, Tokyo, Japan, or J-Graft; Japan Lifeline, Tokyo, Japan) was used for HAR. In AAD cases, the distal aortic stump was reinforced with double felt strips. After the distal anastomosis, systemic circulation was resumed through the branch of the prosthesis and the patient was rewarmed to a rectal temperature of 35°C. Concomitant procedures were performed during core cooling and rewarming. After the proximal anastomosis, the patient was weaned off CPB.
2.3. Study Endpoints and Definitions
The study endpoint was the incidence of postoperative acute kidney injury (AKI). Postoperative AKI was diagnosed in accordance with the Kidney Disease: Improving Global Outcomes (KDIGO) classification (Table 2) [11]. We evaluated postoperative change in plasma creatinine (Cr) concentration during the first postoperative week and compared it with preoperative baseline value since the AKI was defined by the plasma Cr increase within 1 week in the KDIGO classification. Left ventricular dysfunction was defined as left ventricular ejection fraction of ≤40%. Nonelective surgeries included both emergency and urgent cases according to the definitions used in the Society of Thoracic Surgeons database. Delayed awakening was defined as recovery of consciousness more than 48 hours after surgery. A postoperative stroke was defined as the occurrence of a new stroke confirmed by computed tomography or magnetic resonance imaging. Operative death was defined as death occurring during the same hospitalization or after discharge from the hospital but within 30 days of the procedure.
| Stage | Plasma creatinine increase |
|---|---|
| 1 | 1.5 to 1.9 times baseline or ≥0.3 mg/dl increase |
| 2 | 2.0 to 2.9 times baseline |
| 3 | ≥3.0 times baseline or increase in plasma creatinine to ≥4.0 mg/dl or requirement of renal replacement therapy |
- Acute kidney injury is diagnosed when there is an increase in plasma creatinine concentration ≥0.3 mg/dl within 48 hours or an increase of at least ≥1.5 times baseline within 1 week. KDIGO, Kidney Disease: Improving Global Outcomes.
2.4. Statistical Analysis
Continuous variables are expressed as mean ± standard deviation or median with interquartile range (IQR) according to their normality. Examination of normality of each variable was performed using the Shapiro–Wilk test. Continuous variables were compared using the unpaired Student’s t-test or Mann–Whitney U test as appropriate. Categorical variables are shown as actual numbers or percentages and were compared using Pearson’s χ2 test or Fisher’s exact test as appropriate. The association between circulatory arrest time or minimum rectal temperature and plasma Cr increase was assessed by Spearman’s rank correlation coefficient. Multivariate logistic regression analysis with forward-backward stepwise selection was performed using preoperative and operative variables to identify the independent predictors of postoperative AKI. All tests were 2-sided and differences were considered statistically significant at P < 0.05. All statistical analyses were performed using JMP 12.0 statistical software (SAS Institute, Cary, NC, USA).
3. Results
3.1. Perioperative Outcomes
Operative data are summarized in Table 3. Median operating time, CPB time, and aortic cross-clamp time were 264 minutes (IQR, 221–322), 124 minutes (IQR, 106–150), and 94 minutes (IQR, 70–117), respectively. In addition, median circulatory arrest time and minimum rectal temperature were 15 minutes (IQR, 11 to 19) and 27.4°C (IQR, 25.9 to 28.1), respectively. A total of 104 (60.5%) patients underwent concomitant procedures, the most frequent of which was aortic valve surgery.
| Operating time (min) | 264 [221–322] |
| Cardiopulmonary bypass time (min) | 124 [106–150] |
| Aortic cross-clamp time (min) | 94 [70–117] |
| Circulatory arrest time (min) | 15 [11–19] |
| Minimum rectal temperature (°C) | 27.4 [25.9–28.1] |
| Concomitant procedure | |
| Aortic valve surgery | 103 (59.9%) |
| Mitral valve surgery | 12 (6.8%) |
| Coronary artery bypass grafting | 18 (10.5%) |
| Arrhythmia correcting surgery | 7 (4.1%) |
| Intubation time (hrs) | 18 [13–20] |
| ICU stay (days) | 2 [2-3] |
| Delayed awakening | 8 (4.7%) |
| Re-exploration for bleeding | 4 (2.3%) |
| Stroke | 8 (4.7%) |
| Prolonged ventilation requiring tracheostomy | 10 (5.8%) |
| Deep sternal wound infection | 1 (0.6%) |
| AKI | 65 (37.8%) |
| Temporary hemodialysis | 7 (4.1%) |
| Operative death | 2 (1.1%) |
- AKI, acute kidney injury; ICU, intensive care unit.
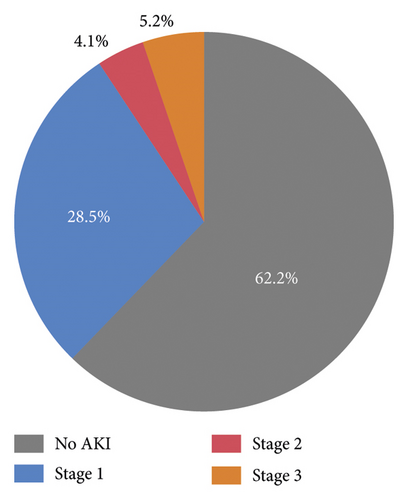
Postoperatively, 65 patients (37.8%) developed an episode of AKI according to the KDIGO classification. Of these, 7 patients required temporary hemodialysis. The incidence of other complications is shown in Table 3. One patient died of hypoxic encephalopathy due to preoperative cardiogenic shock and another patient died of postoperative stroke. Therefore, the perioperative mortality was 1.1%.
3.2. Incidence and Risk Factors of Postoperative AKI
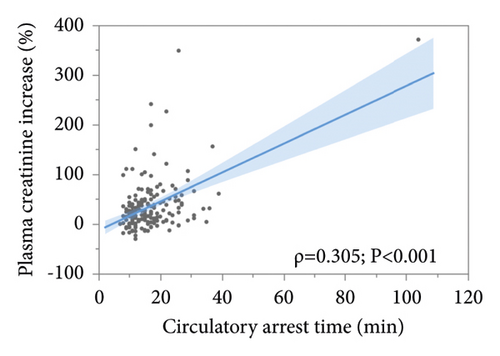
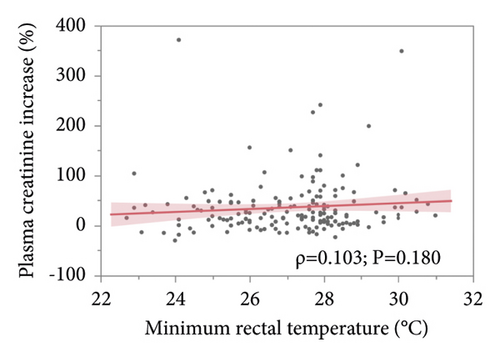
The incidence and severity of postoperative AKI are shown in Figure 1. The overall incidence of postoperative AKI was 37.8% (65 patients). Of these, 49 (28.5%) patients were in stage 1, 7 (4.1%) patients were in stage 2, and 9 (5.2%) patients were in stage 3. Seven of the 9 patients in stage 3 required temporary hemodialysis; however, no patient required permanent hemodialysis. Associations between plasma Cr increase and circulatory arrest time or minimum rectal temperature are shown in Figure 2. Spearman’s rank correlation coefficient showed that there was slight but significant positive correlation between plasma Cr increase and circulatory arrest time (ρ = 0.305, P < 0.001). However, there was no significant association between plasma Cr increase and minimal rectal temperature (ρ = 0.103, P < 0.180). Multivariate logistic regression analysis demonstrated that acute aortic dissection (odds ratio, 4.57; 95% confidence interval (CI), 2.13–10.14; P < 0.001) and longer operating time (odds ratio, 1.01; 95% CI, 1.00-1.01; P = 0.001) were independent predictors for postoperative AKI (Table 4).
| Variables | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Acute aortic dissection | 4.57 | 2.13–10.14 | <0.001 |
| Diabetes mellitus | 2.28 | 0.79–6.78 | 0.129 |
| Coronary artery disease | 2.06 | 0.72–5.94 | 0.178 |
| Cerebrovascular disease | 2.03 | 0.80–5.23 | 0.138 |
| Left ventricular dysfunction | 0.21 | 0.02–1.21 | 0.084 |
| eGFR | 0.99 | 0.97–1.00 | 0.123 |
| Operation time | 1.01 | 1.00–1.01 | 0.001 |
| Minimum rectal temperature | 1.15 | 0.93–1.43 | 0.190 |
- AKI, acute kidney injury; CI, confidence interval; eGFR, estimated glomerular filtration rate.
4. Discussion
We found that postoperative AKI occurred in 37.8% of patients who had undergone HAR under MHCA with RCP. In addition, acute aortic dissection and longer operating time were identified as risk factors for postoperative AKI. Moreover, the novel aspect of this study was evaluation of the association between circulatory arrest time or core temperature and plasma Cr increase. Although there was a significant association between duration of MHCA and plasma Cr increase, circulatory arrest time and minimum rectal temperature were not predictors for postoperative AKI.
AKI is a frequent complication of thoracic aortic surgery with the use of CPB and circulatory arrest. Previous studies demonstrated that several risk factors, such as CPB time, circulatory arrest time, and preoperative serum Cr level, were associated with postoperative AKI [5–9]. However, most of these studies included patients who had undergone total aortic arch replacement, which requires relatively long circulatory arrest time. Although we exclusively used MHCA with RCP when performing HAR without reconstruction of aortic arch branches, which does not require long circulatory arrest time, some of our patients developed postoperative AKI. Therefore, in this study, we aimed to evaluate postoperative AKI in patients who underwent HAR with MHCA, especially focusing on the duration of MHCA or core temperature during circulatory arrest.
Several reports describe circulatory arrest time as a risk factor for AKI after thoracic aortic surgery. Mori et al. showed that the duration of deep hypothermic circulatory arrest was an independent risk factor for AKI after aortic arch surgery [7]. Similarly, Amano et al. reported that lower body ischemic time was a risk factor for AKI after surgery for acute aortic dissection [9]. However, these studies included patients undergoing aortic arch surgery with a relatively long circulatory arrest time of approximately 60 to 75 minutes. Nota et al. also showed that mildly hypothermic lower body circulatory arrest time >60 minutes was a risk factor for postoperative AKI in aortic arch surgery [8]. Similarly, there was significant correlation between circulatory arrest time and postoperative plasma Cr increase in our study (Figure 2(a)). However, multivariate analysis did not show that circulatory arrest time was an independent predictor for postoperative AKI. This discrepancy may be because our study included only patients who underwent HAR and, therefore, the median circulatory arrest time was short (median, 15 minutes; IQR, 11 to 19 minutes). Indeed, previous reports including patients with short circulatory arrest times (17 to 20 minutes) did not find circulatory arrest time to be a risk factor for postoperative AKI [12–14]. These results suggest that relatively short circulatory arrest time is not a risk factor for postoperative AKI.
Moreover, in this study, we also evaluated the association between core temperature and postoperative plasma Cr increase because there remains a concern that moderate hypothermia might be insufficient for nephroprotection. We found no association between minimum rectal temperature and plasma Cr increase (Figure 2(b)). These data are consistent with several previous reports showing that temperature strategy did not affect the incidence of postoperative AKI in thoracic aortic surgery. Arnaoutakis et al. reported no significant difference in AKI incidence between patients who underwent deep hypothermia (lowest temperature: 17.5°C) and those who underwent moderate hypothermia (lowest temperature: 26.4°C) in HAR [12]. Fang et al. also reported similar findings in patients who underwent total arch replacement with frozen elephant trunk procedure for acute aortic dissection [13]. Vekstein et al. found that the association between the degree of systemic hypothermia and AKI was not significant when analyzed as a continuous variable [14]. In our study, the median minimum rectal temperature was 27.4°C and our results are consistent with these previous studies. These findings suggest that moderate hypothermia is sufficient for the protection of renal function, especially in cases with short circulatory arrest time.
In the present study, multivariate analysis showed that acute aortic dissection is an independent predictor for postoperative AKI (Table 4). There are several possible reasons why acute aortic dissection is a risk factor for postoperative AKI. Patients with acute aortic dissection are generally in a critical preoperative state, such as cardiogenic shock due to cardiac tamponade or organ malperfusion, requiring emergency or salvage surgery [15]. Moreover, we have reported that preoperative renal malperfusion is a risk factor for AKI after surgery for acute aortic dissection [16]. In addition, we demonstrated that longer operating time was also a risk factor for postoperative AKI. Many reports show that longer CPB time is a risk factor for postoperative AKI. Pacini et al. reported that CPB time >180 min was the only significant risk factor for renal dysfunction after aortic arch surgery [17]. Moreover, Helgason et al. and Arnaoutakis et al. have also reported that prolonged CPB during surgery for type A acute aortic dissection was identified as a risk factor for postoperative AKI [18, 19]. However, the duration of CPB in these studies was quite long (almost over 180 minutes). We believe that CPB time was not identified as a risk factor for postoperative AKI in our study because the median CPB time was 124 minutes, which was relatively short compared with that of the aforementioned studies.
In conclusion, our finding that operating time is a risk factor for AKI indicates that surgical stress adversely affects postoperative kidney function in HAR. Furthermore, our results suggest that our strategy of MHCA with RCP in patients undergoing HAR is feasible for the prevention of postoperative AKI.
4.1. Study Limitations
This study has several limitations. First, the number of patients was relatively small. Second, this was a retrospective, observational study in a single Japanese center and, therefore, there may be an information bias. Third, patients who had undergone total aortic arch replacement with selective antegrade cerebral perfusion were not included in this study. Therefore, the results of this study may not be applicable to those patients. Finally, we could not evaluate the urine output, which was used to define AKI in the original KDIGO classification. Therefore, it is possible that some patients who did not meet KDIGO plasma Cr criteria would have been reclassified as having sustained AKI if urine output data were available. However, recent studies described that plasma Cr level was a superior predictor of AKI [20, 21]. Therefore, we do not consider that our definition used in this study was inadequate to detect postoperative AKI.
5. Conclusions
In patients undergoing HAR under MHCA with RCP, acute aortic dissection and longer operating time were risk factors for postoperative AKI. Circulatory arrest time and minimum rectal temperature were not identified as risk factors for AKI during relatively short circulatory arrest times.
Consent
The requirement for informed consent was waived because of the retrospective nature of the study.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
We thank Leah Cannon, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Open Research
Data Availability
The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study. The data underlying this article are available from the corresponding author upon reasonable request.