Triple Vessel Coronary Artery Disease Needs a Consistent Definition for Management Guidelines
Abstract
For over forty years, coronary artery bypass grafting (CABG) has been recommended to patients with triple vessel disease (TVD) with the aim of providing a survival benefit compared to medical therapy. Generally, the survival benefit of CABG is determined by (a) the volume of myocardium at risk of infarction according to the extent of coronary artery disease (CAD), (b) the impairment of coronary flow reserve according to severity of coronary stenoses, severity of symptoms, or objective evidence of regional ischemia, and (c) the impairment of myocardial reserve according to left ventricular function and viability. The most frequently used index of survival benefit is the extent of CAD as described by the terms of the left main coronary stenosis and TVD. However, TVD has been inconsistently defined in randomised controlled trials. Furthermore, international guidelines do not provide a specific definition of TVD. This impacts a substantially sized and high-risk population. Here, we argue that the definition of TVD should include diseases in the major artery in each of the three coronary territories in order to estimate the survival benefit provided by CABG.
1. Introduction
Patients with stable ischemic heart disease (SIHD) and triple vessel disease (TVD) have been recommended coronary artery bypass grafting (CABG) with a view to derive a survival benefit compared to medical therapy [1]. Initially, high-risk patient groups with stable angina were classified as having more than 50% narrowing of the major coronary vessels including the main left, the left anterior descending, the circumflex or its marginal branch if it was the principal continuation, and the right coronary artery [2]. This description was used in the early randomised controlled trials (RCTs) of CABG compared to medical therapy for defining subgroup analyses and survival differences. The absence of a definition of TVD in the international guidelines for revascularisation of coronary artery disease (CAD) and the interpretation of contemporary evidence upon which the guidelines have been based have created controversy in the management of the most common cardiac surgical condition in the Western world. This is a narrative review of the literature that will address the controversies related to the definition of TVD in patients with SIHD undergoing revascularisation for survival benefit.
1.1. The Definition of TVD
In the three large early RCTs, TVD was defined as “a reduction of at least 50% in the three major arteries” (Veterans Administration Cooperative Study (VA study)) [3], “a 50% or more obstruction in three major arteries” (European Coronary Surgery Study (ECSS)) [4], and “a 70% or greater reduction in the internal diameter of the right, left anterior descending (LAD), and left circumflex coronary artery” (Coronary Artery Surgery Study (CASS)) [5]. Although the ECSS trial did not state which arteries were major arteries, it is reasonable to assume that the intent and application were consistent with the earlier definition which can be specifically described as triple territory major vessel disease (TtmVD).
The VA trial is the only RCT that has shown a survival benefit for CABG compared to medical therapy in patients with left main stenosis. Enrolment of such patients was low in the ECSS and patients with left main stenosis ≥70% were excluded in the CASS. The ECSS included only patients with good LV function (ejection fraction ≥50%) and was the only RCT that showed a survival benefit for patients with TVD and good left ventricular (LV) function [4] (Table 1). The CASS was the only RCT that used ≥70% coronary stenosis in the definition and included only patients with Canadian Class symptoms ≤ 2 [5], and although it did not show a survival benefit in patients with good left ventricular function, there was a survival benefit in patients with TVD and moderately impaired function (ejection fraction 35–49%) [8]. The absence of a survival benefit from CABG in patients with TVD and good LV function in the CASS likely reflects the protective effect of better coronary flow reserve in patients with low level symptoms. Notably, 20% of patients with TVD in the medical therapy arm in CASS crossed over to CABG within 14 months of randomisation and almost 40% did so by 5 years [5]. This suggests that patients with TtmVD, good LV function, low level symptoms, and minimal ischemia on exercise testing can be observed on optimum medical therapy but that CABG should be recommended if there is any change in symptoms or observable ischemia. A subsequent analysis of patients, who were suitable for randomisation other than by the severity of their symptom class, with TVD and normal LV function in the CASS registry showed a survival advantage provided by CABG [6], consistent with the findings of the ECSS. These RCTs demonstrated that CABG is effective in mitigating the risk of death due to CAD [9]. A summary of the findings of these three RCTs is presented in Table 1, being the only adequately powered RCTs in which survival has been reported in subgroup analyses.
| Randomisation (N) | VA trial [3] (686) | ECSS [4] (768) | CASS [5] (780) | CASS registry [6] (24, 179) | ISCHEMIA [7] (5, 179) |
|---|---|---|---|---|---|
| MT (n) | 47 | 188 | 90 | 127 | 316 |
| CABG (n) | 219 | 70 | 507 | 112 | |
| Survival% MT/CABG | 93/92 | 82.4/94 | 95/95 | 74/92 | 93.2/? |
| p value | NS | 0.0003 | 0.91 | <0.0001 | NS |
- VA = veterans’ administration, ECSS = European Coronary Surgery Study, CASS = Coronary Artery Surgery Study, ISCHEMIA = International Study of Comparative Health Effectiveness with Medical and Invasive Approaches trial, MT = medical therapy, CABG = coronary artery bypass grafting, and NS = not statistically significant (ECSS EF > 50%, VA trial and CASS EF normal. ISCHEMIA LV function not stated).
Although there have been many subsequent RCTs assessing the benefits of intervention for TVD with a variety of definitions, none have specifically analysed the cohort of patients with TtmVD and good LV function to compare the survival from CABG and medical therapy [10, 11]. Assessment of the survival benefit provided by CABG in these patients should be based on the definition used in the determination of the benefit. The international guidelines have not provided definitions of TVD, and although the term “multivessel disease” has implied involvement of more than one territory, this is frequently not stated. Terms such as quadruple vessel disease have added further confusion regarding the definition of TVD and its applicability to prognostic significance.
2. Defining a Survival Benefit from CABG
Ischemic heart disease remains the dominant cause of death in Western society. Patients with left main coronary disease or TtmVD have been shown to have a higher risk of death than those with lesser forms of coronary disease [9]. One of the reasons for the higher risk of death in patients with left main and TtmVD is the large volume of myocardium in jeopardy of infarction [12]. In addition to this, the severity of impaired coronary flow reserve also plays a role in predicting the risk of death. Lastly, it is understood that the extent of CAD is considered a good surrogate measurement of the volume of myocardium at risk and therefore is normally used to express the risk of death in patients with SIHD.
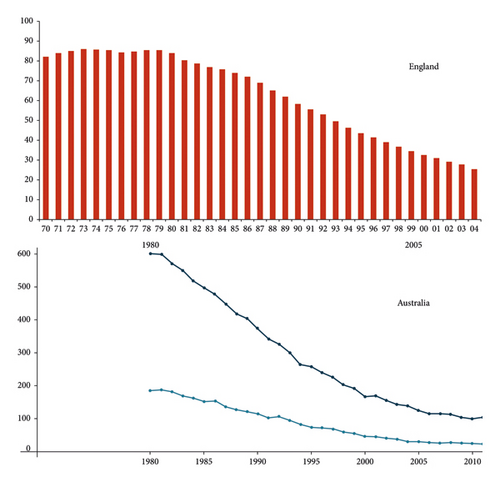
Myocardial infarction in one territory increases workload for the other territories of the heart. In patients with TtmVD, this creates a domino effect where the limited coronary flow reserve is unable to adequately meet the demands of increased workload. In 1979, the ECSS trial demonstrated a survival benefit at two years for CABG in patients with TVD and good LV function [13]. Elective CABG for TVD was widely adopted with an immediate decline in the rate of death from coronary heart disease in Western nations such as England and Australia (Figure 1) [14–16]. However, among patients who die from cardiogenic shock following acute myocardial infarction, the majority have TVD [17]. This highlights a gap in patient care. Utilizing evidence from previous RCTs and the outcomes from the implementation of that evidence will help mitigate the risk of death if elective revascularisation is appropriately recommended by the guidelines.
The patient population and extent of CAD studied in the early RCTs comparing CABG with optimal medical therapy was limited to young patients (<65 years) with discrete proximal coronary disease and TtmVD (involving the major coronary artery in each of the three coronary artery territories) mainly located in or before the proximal half of the artery in its course over the LV [9]. A stenosis in the distal third of major arteries does not subtend a large myocardial volume, and so, its prognostic significance should be related to the myocardial volume at risk.
In contrast to the early RCTs, contemporary studies comparing CABG and percutaneous coronary intervention (PCI) did not stipulate involvement of “the major arteries” in their definitions of TVD. The Fractional Flow Reserve Versus Angiography for Multivessel Evaluation (FAME) III trial defined three vessel disease as “≥50% diameter stenosis by visual estimation in each of the three major epicardial vessels or major side branches” [18] which did stipulate triple territory disease but technically permitted enrolment of patients with disease in a significant diagonal branch without involvement of the LAD. This is consistent with common practice where interventionalists who provide revascularisation to all three territories will count the number of territories rather than the number of the three major arteries revascularised, particularly if the LAD was included. In an analysis of 1,023 patients who underwent bilateral internal mammary artery composite Y grafting, 5.4% received an anastomosis to a secondary vessel in the circumflex territory in the presence of a patent larger artery in that territory. The rates were 0.4% and 0.7% for the LAD and right coronary territories, respectively (unpublished data HSP). These data are consistent with the high rate (97%) of left internal mammary artery (LIMA) use in FAME III suggesting that a negligible number of patients without LAD disease were enrolled. The number of patients with only one or two of the three major arteries revascularised is unlikely to be of little statistically significant unless subgroup analyses are performed. The synergy between PCI with TAXus and cardiac surgery (SYNTAX) trial used the definition “at least 1 significant stenosis in all 3 major epicardial territories supplying viable myocardium” [19] with the requirement that the involved artery diameter be ≥1.5 mm. Although the expression “all three major epicardial territories” rather than all three major epicardial arteries was potentially confusing, the application of the definition would have been similar to that in FAME III, particularly in those with high SYNTAX scores. However, the subgroup analyses with low SYNTAX scores might have included enough patients without TtmVD to affect the statistical significance of the outcomes. Unless specifically stated, a major artery can be considered to be any artery large enough to be suitable for intervention, including secondary branches. However, where there is another artery of similar or greater size supplying the same territory, the volume of myocardium at risk is unlikely to be prognostically significant. Multivessel CAD is a poorly defined term, and if it is used where it does not involve the major artery in any territory, it should be termed as “minor or secondary vessel disease” for prognostic estimates, despite remaining suitable for intervention for symptomatic benefit. Considering this, TVD should be defined by a volume of myocardium at risk exceeding 50% of the myocardial volume in each of the three coronary territories in order to represent an extent of coronary disease for which CABG will provide a survival benefit based on the evidence from the early RCTs [9].
3. International Guidelines
The 2011 ACCF/AHA guidelines [1] for coronary artery revascularisation in SIHD provided a Class 1 recommendation for CABG over medical therapy in patients with “>70% stenoses in 3 major arteries with or without proximal LAD disease” for a survival benefit. A modifying Class 2a “reasonable to choose CABG over PCI in patients with complex 3 vessel CAD” was added. The 2021 ACC/AHA/SCAI guidelines (AHA guidelines) [20] stratified the recommendations for CABG for a survival benefit in patients with “multivessel CAD” according to LV function with Class 1 for severe LV impairment, Class 2a for mild to moderate impairment, and Class 2b (weak) for normal function. The significant downgrades in recommendations occurred despite no change in the level of evidence B-R (one or more randomised clinical trials (RCTs)). Notably, the AHA guideline used three terms, “multivessel CAD,” “3 major coronary arteries,” and “triple vessel disease” apparently interchangeably and without specific definition [20]. The American Association of Thoracic Surgeons and the Society of Thoracic Surgeons have not endorsed these changes to the AHA guidelines [21], and representatives from numerous other international societies have questioned the reasoning [22].
This highlights the need for a clear and prognostically significant definition of TVD to inform clinical decision-making. Terms with poorly discriminatory definitions allow a wide interpretation of TVD and likely reflect popular usage but differ from the definition used that showed a survival benefit from CABG in patients with TVD.
To provide a more precise representation of the survival benefit of CABG in patients with TtmVD and normal LV ejection fraction, it is necessary to incorporate additional criteria such as “Canadian symptom class ≤2 and mild or no regional ischemia on exercise tests or perfusion scans” to justify the class 2b recommendation in the AHA guidelines. Without these descriptors, the survival benefit should not be considered indeterminate. However, such a recommendation would be relevant for only a highly selected group of patients and not applicable across the spectrum of patients with TtmVD. On the other hand, an appropriate definition of TVD that would support prognostic significance would be greater than 50% stenosis in or before the proximal half of the ventricular course of the major artery to each of the three coronary artery territories, where the severity of stenosis is at least 70% in two of those arteries, thus similar to the modified Duke classification for severity of CAD [7, 23]. In cases where codominant arteries exist in one territory, >50% stenoses must exist in the two largest arteries. Logically, this would describe a myocardial volume at risk exceeding 55% of the total normal volume, as in the Bypass Angioplasty Revascularisation Investigation 2 Diabetes (BARI 2D) trial which showed an improved combined outcome (death, stroke, and MI) for CABG versus medical therapy in diabetic patients with >55% myocardium in jeopardy [12].
- (1)
There is no better way to demonstrate this
- (a)
Left main stenosis >50%
- (b)
Proximal left anterior descending artery stenosis >50%
- (c)
Two or three vessel disease (>50% stenoses) with impaired LV EF ≤ 35%
- (d)
Single remaining patent coronary artery with stenosis >50%
- (a)
-
And with documented ischemia or physiologically significant stenoses or visual assessment of a major artery >90%
- (2)
A large area of ischemia detected by functional testing (10% LV) and invasive FFR <0.75
Notably, TVD with good or moderately impaired LV function was excluded from the “for prognosis” list (unless two of the three major arteries were occluded) despite the requirement for documented evidence of ischemia. A proximal left anterior descending artery stenosis >50% (presumably including single vessel disease) was included on that conditional basis. No definition of TVD was provided nor was it stated that there was a correlation between extent of vessel disease and extent of myocardial territory involvement, i.e., TVD equals triple territory myocardial risk.
Both the AHA and ESC guidelines acknowledged diabetes as a prognostic modifier driving better outcomes from CABG compared to PCI. The ESC guidelines provided a separate set of recommendations for either PCI or CABG when revascularisation was considered appropriate for survival or symptomatic benefit. As the symptomatic benefit is similar, it is presumed that the recommendations for CABG compared with PCI are based largely on survival benefit, but these were not included in the “for prognosis” recommendations.
In nondiabetic patients with three vessel disease and a low SYNTAX score, the ESC guidelines provided PCI and CABG class 1 recommendations. In those with intermediate and high SYNTAX scores, the recommendation for PCI was reduced to 2a and 3, respectively, while the recommendation for CABG remained class 1. In contrast to the ESC guidelines’ recommendation for three vessel disease, the AHA guidelines disregarded the findings of the SYNTAX trial, instead stratifying patients according to LV function regardless of severity of symptoms or objective evidence of ischemia. For patients with TVD and good LV function, the class 2b recommendation was provided for both CABG and PCI with “may be reasonable” for CABG and “usefulness…to improve survival is uncertain” for PCI.
A class 2a recommendation was provided “in selected patients with SIHD and multivessel CAD appropriate for CABG and mild-to-moderate left ventricular systolic dysfunction (ejection fraction 35%–50%), CABG (to include a left internal mammary artery (LIMA) graft to the LAD) is reasonable to improve survival.” As it is generally accepted that almost all stenosed LADs should receive a LIMA graft, the recommendation for a LIMA graft is an unnecessary duplication and implies that multivessel CAD does not necessarily involve the LAD. However, multivessel disease with LAD involvement is not specific enough to define TtmVD. If the AHA guidelines had used a more specific definition of multivessel disease such as TtmVD according to the early RCTs, this recommendation would cover a substantially sized and high-risk population for whom it would be difficult to demonstrate an adequate mitigation of risk by guideline-directed medical therapy alone.
4. Use of Contemporary Literature in 2021 AHA Guidelines
4.1. Randomised Controlled Trial
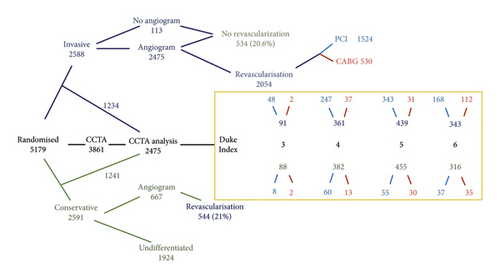
The AHA guidelines cited the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial [25] as new evidence contesting the findings of the early RCTs relating to TVD and normal LV function. The main limitations of the ISCHEMIA trial in determining the survival benefit provided by CABG have been presented elsewhere [21]. The hazard ratios for the outcomes were related to the severity and number of stenosed vessels and to the modified Duke index of severity of CAD as assessed on the coronary computed tomography angiograms (CCTAs) [7] (Table 2, Figure 2). The modified Duke coronary disease classification used >70% stenosis in each of the three major arteries or ≥70% stenosis in two vessels including the proximal left anterior descending (LAD) artery to define the highest risk category [7, 23]. Based on the CCTA findings, greater severity of CAD was associated with increased risks of all-cause death, cardiovascular death, myocardial infarction, and the primary outcome (cardiovascular death, myocardial infarction, or hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest) [7] (Table 2). In the CAD-stratified cohorts, the only outcomes for which the invasive strategy provided a significant reduction in the risk compared to the conservative strategy during the four-year period of follow-up were for myocardial infarction in the two-vessel >70% stenosis cohort and for the combination of myocardial infarction and cardiac death in the modified Duke 6 cohort [7]. Although the invasive strategy achieved a reduction in some of the risks relative to the conservative strategy, it did not remove the risks associated with CAD severity and extent that would normally be associated with a survival benefit provided by CABG (Table 2). CAD severity is a very weak predictor of outcomes following CABG. The outcomes associated with the dominance of allocation of patients with extensive CAD to PCI (Table 1, Figure 2) are consistent with the AHA guidelines which state that “there are no RCTs that have demonstrated a survival advantage of PCI over medical therapy in patients with SIHD.” However, this allocation was a violation of the study protocol which recommended “guidelines from professional societies and appropriateness criteria should be incorporated into the decision process” for allocation of patients to PCI or CABG (AHA 2011 guideline [1]: CABG class 1, PCI class 2b; ESC 2014 guideline [26]: CABG class 1 and PCI class 3 for SYNTAX score >22). Despite this, the authors appear to argue that the higher mortality in patients with extensive CAD was a disease effect immune to an interventional treatment effect. Essentially, those patients are stuck with their higher mortality risk with the implication that no treatment strategy will provide better risk mitigation than medical therapy alone; “we cannot definitively conclude that those with the most extensive CAD benefit from an invasive strategy” [7]. However, as CABG was provided to a minority of patients to whom it should have been allocated, it is logical to conclude that the multiple violations of the study protocol resulted in avoidable deaths in the invasive arm. The extent and impact of the protocol violations based on the findings of direct coronary angiography in the invasive arm have not been reported, without which the significance of the trial findings may be considered indeterminate. The need to blind clinicians to the results of the CCTAs in the conservative arm to ensure protocol adherence seems to have been validated by the extent of violations in the invasive arm which might have been predicted but not monitored. Future RCTs involving patients with TtmVD must have a definitive CABG arm to allow monitoring of the safety of randomisation of patients to the alternate strategy arm. Although this might have been the intention of the ISCHEMIA protocol, it was not the application.
| Outcome (ref Duke 4) | Duke 6 HR (95% CI) | Duke 5 HR (95% CI) | ||
|---|---|---|---|---|
| All mortality | 2.27 (1.37–3.75) | 1.46 (0.88–2.44) | ||
| Cardiovascular death | 3.53 (1.71–7.28) | 2.76 (1.35–5.64) | ||
| Primary outcome | 1.91 (1.39–2.65) | 1.43 (1.04–1.96) | ||
| Myocardial infarction (MI) | 1.69 (1.17–2.45) | 1.15 (0.8–1.67) | ||
| Cardiovascular death/MI | 1.90 (1.36–2.67) ∗ ^ | 1.43 (1.03–2.0) | ||
| Outcome (ref 1 vessel = stenosis) | 2 vessels ≥70% | 3 vessels >50% | 3 vessels ≥70% | |
| All mortality | 1.61 (1.03–2.52) | 2.08 (1.28–3.38) | 2.4 (1.54–3.76) | |
| Cardiovascular death | 2.08 (1.18–3.66) | 3.58 (1.77–7.23) | 3.26 (1.87–5.68) | |
| Myocardial infarction (MI) | 1.37 (0.98–1.93) ∗ | 2.35 (1.61–3.43) | 2.11 (1.50–2.97) | |
- Modified Duke 6 = equal or greater than 70% stenosis in each of the three major arteries or >70% two vessel stenosis with proximal LAD involvement. Duke 5 = two vessel >70% stenosis not including the proximal left anterior descending artery (LAD), single vessel >70% stenosis of the proximal LAD, or 3 vessel moderate stenosis >50%. The reference for comparisons was Duke 4 = two vessel >50% stenosis or single vessel >70% stenosis other than the proximal LAD. ∗Event rates in the invasive arm significantly lower than in the conservative arm. ^Comparison between invasive and conservative arms excluded patients with no or mild ischemia on pre-enrolment testing (n = 28).
4.2. Meta-Analyses of RCTs
The AHA guideline also cited one network meta-analysis [10] and four meta-analyses of RCTs comparing CABG, PCI, and medical therapy for patients with SIHD [11, 27, 28] as additional justification for the downgrading of the recommendation for CABG. Only one of the analyses analysed outcomes according to the percent of patients with multivessel disease [11]. No analyses were performed on TVD subgroups. The network meta-analysis of 100 RCTs provided three-way comparisons of CABG, PCI, and medical therapy and showed a survival benefit provided by CABG over medical therapy [10]. The four meta-analyses combined CABG and PCI into a single revascularisation group for comparison with medical therapy, and none showed an overall survival benefit for revascularisation compared to medical therapy. One of the four meta-analyses included the early trials of the 70s, and this was the only meta-analysis to show a reduction in cardiac death in the revascularisation group [11]. All five analyses included the only two RCTs of CABG versus medical therapy for patients with multivessel CAD and good LV function undertaken since the early trials of the 70s [12, 29].
The Medicine, Angioplasty, or Surgery Study (MASS) II required multivessel CAD >70% stenosis and randomised 406 patients (mean LVEF 67.5% and TVD 58.5%) to CABG or medical therapy [29]. The outcomes for patients with TVD were not reported separately. There was a nonsignificant reduction in all-cause mortality in the CABG group at 5 and 10 years but a significant reduction in cardiac death at 10 years.
In the Bypass Angioplasty Revascularisation Investigation 2 Diabetes (BARI 2D) study, 763 diabetic patients with symptoms or evidence of myocardial ischemia that would prompt revascularisation and with multivessel CAD >50% stenosis were enrolled and randomised to either CABG or medical therapy [11]. In the subgroup of patients with three vessel disease (CABG n = 165 and medical therapy n = 156), there was a statistically significant benefit for CABG in reducing the primary combined outcome of death, myocardial infarction, and stroke (p = 0.0084), but death was not reported independently. There was also a similar benefit provided by CABG in the subgroup of patients with a high myocardial jeopardy score (>55% of total myocardial volume) (p = 0.0038). The outcomes of patients with three vessel disease and good LV function were not reported separately.
The only other RCT to compare CABG and medical therapy in patients with CAD “amenable to CABG” included only those with severe LV impairment (ejection fraction <35%) and showed a survival benefit from CABG at 10 years [30].
5. Summary
TVD is a surrogate measurement of a high myocardial volume at risk of infarction and is the most commonly used parameter to estimate the risk of death in patients with SIHD. However, impaired LV function (estimated by reduced ejection fraction), impaired coronary flow reserve (tightness of coronary stenoses, physiological testing, and myocardial perfusion scans), and severity of symptoms or ease of onset of ischemia (Canadian Class, early symptoms on exercise test) all reduce the survival of patients with SIHD and should be included in the estimate of risk that can be mitigated by CABG. TVD should be defined according to the definition used in the RCTs that have shown a survival benefit for CABG. The international guidelines should be amended to incorporate these factors in their recommendations for revascularisation of CAD.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Acknowledgments
Open access publishing was facilitated by The University of Adelaide, as part of the Wiley–The University of Adelaide agreement via the Council of Australian University Librarians.
Open Research
Data Availability
No data were used to support the findings of this study.