The Nature and Quality of Support from Informal Networks for Informal Caregivers of Low-Grade Glioma Patients: A Qualitative Analysis within the Ways Ahead Study
Abstract
Objective. Those closest to the patients with low-grade glioma (LGG) often become informal caregivers (ICs). Caregiving demands can impact ICs’ wellbeing, meaning they themselves may require support. We explored the nature and quality of support from informal networks for ICs of LGG patients. Methods. In this cross-sectional qualitative study, semistructured interviews were conducted with individuals from the United Kingdom who currently, or in the past five years, informally cared for someone diagnosed with an LGG. Interviews explored ICs’ experiences of receiving support from informal networks. Thematic analysis was undertaken. Results. Nineteen ICs were interviewed (mean age 54.6 years; 5 males, 14 females). ICs received multiple forms of support from their informal networks: emotional (e.g., “opportunities to talk”), instrumental (e.g., “opportunities for relief”), information (e.g., “information from network contacts”), and appraisal (e.g., “comparisons with similar others”). Networks comprised strong/familiar (e.g., close friends) and weaker/unfamiliar (e.g., other ICs) ties. Supportive networks were perceived to help protect ICs’ wellbeing. Participants perceived challenges such as poor understanding and unsolicited advice to weaken the quality of support. Conclusion. Informal networks can provide wide-ranging support for ICs of the LGG patients. Different supports may be sought or provided from different contacts, highlighting the importance and value of extended networks.
1. Introduction
Low-grade gliomas (LGGs) are mostly diagnosed in people in their 30s and 40s, at a crucial time in individual’s working and family lives [1]. They are largely incurable and likely to progress, limiting life expectancy to 5–15 years [1, 2]. Patients with LGGs, or other brain tumours, can experience wide-ranging social and role implications (e.g., work, relationships, loss of independence) [3] as a result of varying, often co-occurring, symptoms and impairments, including fatigue, seizures, cognitive and communication impairments, personality changes, and mobility issues [4]. Living for several years with these impairments can have a profound impact on both the individual and those closest to them.
Family-members, partners, and close friends of those with cancer often assume the role of informal caregiver (IC), adopting additional responsibilities, both practical (e.g., managing finances and childcare) and psychosocial (e.g., providing emotional support) [5]. The burden associated with caregiving for someone with cancer is well-documented and can significantly impact the IC’s wellbeing and ability to maintain standards of day-to-day living [6]. Brain tumour patients have indicated a preference for support from ICs over the healthcare system [7]. However, following a brain tumour diagnosis, ICs may feel inadequately prepared to take on caregiving responsibilities [8]. The incurable nature of an LGG diagnosis means that ICs face distinct challenges with psychological burden (e.g., fear of progression) [9] and adjustment (e.g., acceptance of prognosis and changes in family roles) [10]. The impact of personality changes, fatigue, and cognitive and communication impairments on relationship dynamics means many ICs of the brain tumour patients report relationship decline [11]. Consequently, ICs can experience difficulties with anxiety, depression, trouble sleeping, or physical health strain [12, 13].
Caregiving burden may vary across different cancers and across the illness pathway. These demands may be such that ICs themselves may require support [14], underlining the importance of understanding the distinct needs of ICs for different cancers and at different times since diagnosis. Informal networks (e.g., friends and family) are often cited as an essential source of that support [15]. In 1981, House [16] proposed a four-dimensional framework of social support, consisting of emotional, instrumental, information, and appraisal support, that, when received, can influence IC self-esteem and self-efficacy [17]. In cancer, ICs’ informal networks can provide them with instrumental or emotional support [18] and be a powerful tool to help combat negative experiences and feelings [19]. Indeed, some ICs report that the value of social relationships increased following a cancer diagnosis [20]. This points to the importance of ICs having a strong and effective informal support network in order to protect their wellbeing. It is, therefore, important to examine whether the dimensions of House’s framework [16] are relevant to the wellbeing and supporting self-esteem and self-efficacy in ICs of people living with a brain tumour.
This is the first study to explore the experiences of informal support for the ICs of the LGG patients. We aimed to investigate the nature and quality of the support from informal networks for the ICs of the LGG patients, exploring the potential to protect the ICs’ wellbeing.
2. Methods
2.1. Design
This cross-sectional qualitative study was nested within the wider Ways Ahead study. The study [21] was reviewed and approved by the Wales Research Ethics Committee (REC ref: 20/WA/0118). This study was reported in accordance with the Critical Appraisal Skills Programme (CASP) checklist for quality assessment of qualitative studies (Supplementary file 1). The present study focused specifically on the nature and quality of support from informal networks for ICs of LGG patients.
2.2. Participants and Recruitment
Participants were family-members or friends of an LGG patient who lived in the United Kingdom. Individuals were eligible if they were aged ≥18 years and currently, or have in the past five years, informally cared for someone with an LGG, specifically a grade II or III oligodendroglioma or grade II astrocytoma [22].
Potentially eligible ICs were approached as “family-members or friends” and identified via three avenues. Firstly, LGG patients interviewed in the Ways Ahead study were asked to nominate someone informally involved in their support. The researchers provided a participant information sheet to be passed on to the nominated IC. Secondly, healthcare professionals at collaborating National Health Service (NHS) sites identified and provided ICs with a participant information sheet. Thirdly, the study was advertised, with the participant information sheet attached, through The Brain Tumour Charity’s networks. For all avenues, ICs were asked to contact the study team to register their interest. BR and LD subsequently telephoned the IC to confirm eligibility, provide the opportunity to ask questions, and arrange a convenient interview date and time, if willing to take part. Participants were recruited between August 2020 and March 2022.
2.3. Data Collection
Interviews were conducted by BR and LD, both trained and experienced in qualitative research, with no prior relationship with the participants. All interviews took place remotely on video-conferencing software (e.g., Zoom or Microsoft Teams) or by telephone, as per interviewee preference. Audio-recorded consent was acquired, immediately prior to each interview.
Interviews were semistructured following a topic guide (Supplementary file 2), which comprised open questions informed by existing literature and expert knowledge (JL and SW). Prior to data collection, the topic guide was discussed with a patient and public involvement panel including ICs and modified appropriately. Flexible use throughout data collection allowed any new issues raised during the interviews to be added for exploration in subsequent interviews.
To begin, participants broadly reflected on their experiences of supporting someone living with a brain tumour. Participant views on how the patient has been impacted by the tumour and its treatment, and their own impact and support needs across numerous areas (e.g., emotions, family, and transport) were then explored. For each area, we asked about the role and responsibilities involved in supporting the patient as well as what and when participants received or needed (in)formal support. Appropriate use of probe questions explored any challenges faced. Participants were allowed the opportunity to raise any additional issues they felt were important. Finally, a £20 voucher was offered to thank them for their time, and a debrief sheet was provided with details of charities and helplines, should they have questions or concerns, or experience distress following the interview. Interviews were audio-recorded and lasted on average 85 minutes (range 54 to 110 minutes).
2.4. Data Analysis
Participants were pseudonymised with a unique participant ID. Interviews were transcribed verbatim and anonymised by an external service. For accuracy, transcripts were checked against the interview audio-recordings. An inductive, data-driven approach was used in line with thematic analysis [23, 24]. Analysis was paralleled with data collection to ensure that the new issues raised were explored in subsequent interviews. This analysis focused specifically on the nature and quality of support from ICs’ informal networks.
Two trained researchers (AM and BR) independently familiarised themselves with the data and generated initial codes for a sample of transcripts (n = 5 of 19). Preliminary themes were constructed at the semantic level and discussed and modified by the researchers, following consensus on any differences. Remaining transcripts were analysed by AM; emerging findings and uncertainties were discussed with the wider research team. Findings were then deductively mapped to House’s four dimensions of social support [16] relevant to caregiving literature in other cancers [18]. We aimed to examine consistency with predetermined benefits of social support and identify how our findings support, refine, and extend their influence on IC wellbeing in a different context. Inter-relationships between dimensions were noted. We examined data saturation by assessing whether the last three interviews added anything new to the coding frame. In reporting the results, in relation to network nature, we have described types (dimensions) of support received and from whom, or where, it was received. In terms of quality, we have reported, for each dimension of support, ICs’ experiences (both positive and negative) of the support received.
3. Results
3.1. Participant Characteristics
Twenty-four ICs registered an interest in taking part; of these, 22 were eligible (n = 2 were not eligible because the care recipient’s tumour was not a LGG) and 19 were interviewed (NHS recruitment (n = 7); the Brain Tumour Charity (n = 12)). Mean age was 54.6 years (range 36–78 years) and 14 participants were female (Table 1). All except one participant was married. Fifteen were spouses, two sisters, and two mothers of the LGG patients. Six (all being spouses) had children (aged <18). At the time of interview, 13 were employed (10 in full-time employment).
| Characteristics | n |
|---|---|
| Sex | |
| Female | 14 |
| Male | 5 |
| Age | |
| ≤40 | 3 |
| 41–50 | 3 |
| 51–60 | 8 |
| >60 | 5 |
| Employment status | |
| Full-time employee | 10 |
| Part-time employee | 3 |
| Retired | 4 |
| Caring for family | 2 |
| Relationship to care recipient | |
| Wife | 10 |
| Husband | 5 |
| Mother | 2 |
| Sister | 2 |
| Relationship status | |
| Married | 18 |
| Single | 1 |
| Dependents | |
| None | 13 |
| One | 3 |
| Two | 3 |
| Mean (range) | |
| Full-time education (years) | 14.9 (10–18) |
3.2. Overview of Findings
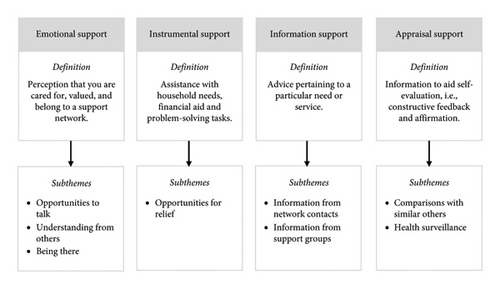
The themes (following House’s framework) [16] and associated subthemes are shown in Figure 1; supporting quotes are presented throughout and in Table 2. Throughout the results, ICs sought and received different supports from different contacts, expressing the value of strong/familiar (e.g., close friends) and weaker/unfamiliar ties (e.g., other ICs).
| Theme | Subtheme | Illustrative quotes |
|---|---|---|
| Emotional support | Opportunities to talk |
|
| Understanding from others |
|
|
| Being there |
|
|
| Instrumental support | Opportunities for relief |
|
| Information support | Information from network contacts |
|
| Information from support groups |
|
|
| Appraisal support | Comparisons with similar others |
|
| Health surveillance |
|
|
3.3. Emotional Support
Emotional support concerned the perception of being cared for, valued, and belonging to a support network. Subthemes were opportunities to talk, understanding from others, and being there.
3.3.1. Opportunities to Talk
All participants reported receiving emotional support through conversations with others. Most described feeling was able to openly talk to friends and family as an important source of reassurance and support. For some, speaking with close contacts was a welcome distraction. Some participants reported value in hearing others’ perspectives to consider different viewpoints, though others expressed frustration at receiving unsolicited advice.
“I’m sure it helped to have friends and neighbours to talk to and just go over things with…that allowed me to be calmer and more supportive.” – IC13 (aged 51, husband)
3.3.2. Understanding from Others
“We started going back out having a drink and it wasn’t the focus of the conversation. It was a known thing. It wasn’t an elephant in the room.” – IC12 (aged 66, wife)
3.3.3. Being There
“My work were texting me all the time, “How are things? Are you okay? Do you want somebody there with you?” just that caring.” – IC2 (aged 55, wife)
3.4. Instrumental Support
Most participants described instances of instrumental support, which concerned assistance with finances and daily tasks, such as transport, housework, and childcare. The only subtheme was opportunities for relief.
3.4.1. Opportunities for Relief
“They would take [child] and [child] overnight…his mum will take a load of ironing away and come back and have it all done. So, that’s lovely.” – IC15 (aged 44, wife)
3.5. Information Support
Most participants reported receiving information support related to managing the consequences of the tumour and its treatment. Subthemes were information from the network contacts and information from the support groups.
3.5.1. Information from Network Contacts
“My sister’s a [job role], and it’s her job to help people in [patient]’s situation…so if I needed knowledge I’d get it from her.” – IC10 (aged 59, wife)
3.5.2. Information from Support Groups
“We actually met at the Maggie’s centre. We were both doing the stress group on how to relieve your stress…there was about six of us in the group and we’ve all stayed in touch.” – IC19 (aged 54, wife)
3.6. Appraisal Support
Appraisal support concerned information that aided self-evaluation of the participant’s own, and the LGG patient’s, health. Subthemes were comparisons with similar others and health surveillance.
3.6.1. Comparisons with Similar Others
“To be able to see… that he has come off quite well… by comparison to other people.” – IC5 (aged 64, wife)
3.6.2. Health Surveillance
“My dad is often here helping to look after him, pretending he’s doing a bit of work in the house but he’s really keeping an eye on him for me if I’m at work.” – IC14 (aged 37, wife)
3.7. Inter-Relatedness of Support Dimensions
“Various friends have offered, “Look, if you ever need somebody to sit with [patient] and you go out for the afternoon, just pick up the phone,” which is lovely.” – IC24 (aged 67, husband)
4. Discussion
The tumour- and treatment-related limitations experienced by LGG patients mean those closest to them often adopt a caregiving role. However, not least due to the psychological burden from the incurable nature of the condition, ICs can experience a substantial impact on their wellbeing, for which informal networks (e.g., family, friends, and colleagues) are an essential source of support. This study, therefore, aimed to explore the nature and quality of support from informal networks for ICs of LGG patients.
Findings from interviews with 19 ICs were mapped to the four dimensions of social support, [16] namely, emotional (e.g., “opportunities to talk”), instrumental (e.g., “opportunities for relief”), information (e.g., “information from network contacts”), and appraisal (e.g., “Health surveillance”).
4.1. Support Dimensions
All participants described the importance of emotional support, valuing the care provided by friends and family. Participants particularly valued being listened to and having the opportunity to talk, which were consistent with several studies exploring caregiving in other cancers [7, 25, 26]. Since ICs might feel unable to fully express their emotions to the patient [19], such support from informal networks may be crucial [14].
Our findings support the cathartic function of opportunities to vent [27], a support mechanism scarcely evidenced in the cancer literature. Still, venting may only be beneficial if met with the appropriate response, as feeling listened to and understood has distress-buffering effects [28]. What our study adds is the value of passive listeners, as participants sought an outlet, not a solution. We might speculate that ICs place more expectation on a solution to be provided by their formal networks. Ultimately, finding, or facilitating, mechanisms for stress relief may be important to mitigate caregiver burden.
The feeling that informal networks understood the symptoms and severity of an LGG was highly regarded, though often absent. Reported misconceptions of disease severity evoked frustration [29], which was exacerbated by the perception that LGG is an “invisible” disease, due to “hidden” impairments (e.g., cognitive deficits and fatigue). [30] Consequent informal support is perceived as inadequate [11], artificially positive [19], or insensitive [29]. A perceived lack of understanding from others may, therefore, be a barrier in receiving emotional support, inciting the feelings of isolation. The “family unit” was particularly valued in our findings, approaching caregiving demands collectively. These high-quality family relationships could be associated with lower caregiver burden [31], as they feel able to share the caregiving demands. Still, colleagues, social group members, and neighbours were also cited as sources of informal support with no preferences given.
Most participants appreciated opportunities for relief from daily tasks (i.e., household chores and childcare), which afforded some the opportunity for self-care (e.g., socialising with friends). This is important, as caregiving demands typically detriment an IC’s social wellbeing [9, 19]. Indirect instrumental support (e.g., financial aid) was also valuable for mitigating caregiver burden, particularly if the condition has influenced changes in employment for the IC or patient [32, 33].
Some participants appreciated information, especially practical advice, offered from informal contacts, particularly those in healthcare positions. Such support is especially important if the IC feels ill-informed by formal healthcare channels [7]. Several participants indicated the value of appraisal support. Some described a feedback system, whereby informal contacts monitored the IC’s and LGG patient’s wellbeing, informing the IC of any changes. This was important for ICs whose focus on caregiving meant they had neglected their own wellbeing. To our knowledge, this is a novel finding, with future research required to consider the influence of “health surveillance” on protecting an IC’s wellbeing.
4.2. Support Groups
Across emotional, information, and appraisal support, we highlight the potential benefits and hindrances from support groups. Such groups for ICs may be a favourable avenue of emotional support, particularly where understanding from friends and family is lacking [14, 25]. They may also be a useful access point to wide-ranging information resources, as advice and experiences can be exchanged at any given time with those in similar circumstances. However, our findings support that ICs might avoid support groups to protect themselves from negative experiences, such as reminders of the tumour’s inevitable outcome [30], potentially exacerbated if a support group member died [13]. Furthermore, there is value and risk in interacting with similar others on an IC’s self-efficacy, depending how they perceive their situation in relation to other ICs [17, 34]. Consequently, guidance outlining the potential implications of interactions in support groups may be beneficial to inform an IC’s approach to this avenue of support. This should acknowledge that each LGG patient is individual in the potential prognosis, which is the extent of tumour- and treatment-related limitations experienced.
4.3. Benefits of Extended Informal Networks
While friends and family can provide emotional and instrumental support, valuable information and appraisal support may come from interactions with other ICs (e.g., via support groups). Our findings suggest, for the first time in brain tumours, that ICs may seek different supports from different contacts, in accordance with the expanded network theory [35]. Strong/familiar ties (e.g., close friends) may share similar perspectives and backgrounds, limiting the ability to obtain diverse information. Interactions with strong/familiar ties may also expose the IC to judgement, while weaker/unfamiliar ties (e.g., other ICs) might allow sensitive topics to be broached without repercussions [36]. The absence of intimacy from weaker/unfamiliar ties, however, means shared information is limited to the IC’s immediate needs [37]. Thus, to receive a full range of support mechanisms and diverse social resources, ICs may benefit from engagement with both strong/familiar and weaker/unfamiliar ties. The extended prognosis of LGGs means different supports are likely to be needed over time. Hence, where appropriate, ICs should be encouraged to engage with available support groups and other ICs, in addition to their strong/familiar ties. However, given the associated concerns with support groups, alternative ways to form and maintain weaker/unfamiliar ties require further consideration.
4.4. Implications
These findings provide important considerations for healthcare professionals, particularly nurses, given they are often a key point of liaison with the patient’s family. Our findings highlight the potential benefits of opportunities to talk; health professionals may consider ways to facilitate opportunities to talk to a passive listener, without judgement or unsolicited advice. Perceiving an understanding of the condition and its severity was highly regarded by ICs. It may be beneficial to provide ICs with guidance on “what to expect” with LGGs and support needs of ICs, which they could disseminate to their informal network, better equipping the network to provide support.
Overall, we highlighted the wide-ranging value of support from informal networks; this may outline potential unmet support needs in ICs whose informal support network is limited (e.g., poor family relationships), or unavailable (e.g., distant proximity). This has implications across all four support dimensions, most pertinently instrumental support, as there are challenges with remote provision of opportunities for relief. Consequently, the size and/or availability of an IC’s informal network should be acknowledged to understand possible disparities in ICs’ wellbeing. Following from this, where health systems allow, cancer nurses could have an important role in assessing whether ICs themselves may need care interventions or other support to manage the challenges of caregiving.
4.5. Strengths and limitations
The main strength of our study is the novel understanding of the informal support mechanisms for ICs of LGG patients, who to date have been under studied. While emotional support was particularly valued, our findings benefit from eliciting the importance of instrumental, information, and appraisal support; mechanisms were rarely explored in the cancer literature. With regards to this analysis, the last three interviews did not add anything new to the coding frame, so we are confident that reasonable data saturation was reached. Our sample benefitted from a representation of male ICs, as they are typically underrepresented in caregiving literature [38].
Informal support networks were a secondary focus of the interviews, which may have implications for whether support mechanisms were explored in sufficient depth. Still, the length of the interviews shows that the participants were comfortable and invested in sharing their experiences; there was no sense, even in the longest interviews, that participants became fatigued or that the interview quality was compromised. Our sample largely comprised spousal ICs, and the few nonspousal ICs were often “secondary” ICs; some care is needed in interpreting the findings as it regards other types of ICs (e.g., primary nonspousal). Due to Covid-19, partial recruitment through The Brain Tumour Charity’s networks means participants may have been self-selected, inadvertently recruiting those in a more “active” caregiving role, with more time and interest in taking part. Furthermore, all interviews had to be conducted remotely, though this may have eased participant discomfort and encouraged greater disclosure [39].
5. Conclusion
The challenges of being an IC for an LGG patient can be detrimental to the ICs wellbeing, for which their informal networks are an essential source of support. This study, for the first time, explored the nature and quality of support from informal networks for ICs of LGG patients. Informal networks can provide wide-ranging support to help protect ICs wellbeing, namely, emotional (e.g., “opportunities to talk”), instrumental (e.g., “opportunities for relief”), information (e.g., “information from support groups”), and appraisal (e.g., “health surveillance”). Different supports may be sought or provided from different network contacts. We highlighted the importance of extended networks, encouraging engagement with strong/familiar and weaker/unfamiliar ties.
Disclosure
The analysis was conducted as a part of the MSc in Public Health at Newcastle University.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors’ Contributions
LS, PG, RB, JL, SW, VAS, and TF conceived the Ways Ahead study and secured the funding; LS, BR, and LD designed the study; BR and LD collected the data; AM and BR performed data coding and analysis; AM and BR wrote the initial draft of the paper. All authors critically reviewed the paper and approved the final version for submission. Andrew James Murrell and Ben Rimmer contributed equally to this work.
Acknowledgments
This is an output for the Ways Ahead project (research.ncl.ac.uk/waysahead). The authors would like to thank our collaborating NHS sites, Newcastle upon Tyne Hospitals NHS Foundation Trust, NHS Lothian, The Christie NHS Foundation Trust, and South Tees Hospitals NHS Foundation Trust, as well as colleagues at the Brain Tumour Charity, for their assistance with recruitment to the project. This work was supported by funding from the Brain Tumour Charity (GN-000435).
Open Research
Data Availability
The data that support the findings of this study may be available from the Chief Investigator (Professor Linda Sharp; [email protected]) upon reasonable request.