[Retracted] A Study on the Impact of Perioperative Pain Care Management on Pain, Comfort, and Defecation of Patients in Anorectal Surgery
Abstract
Purpose. The aim of the study is to explore the impact of perioperative pain care management on patients’ pain, comfort, and defecation in anorectal surgery. Methods. From January to December 2021, 126 patients who underwent anorectal surgery in our department were selected for the study and were randomly divided into a study group and a control group of 63 patients each after consent was obtained from the patients. The control group was given the usual care protocol and the study group was given the perioperative pain care management on top of the usual care. The two groups of patients were compared in terms of postoperative anal pain rating, comfort score, time to first bowel movement and time spent in bowel movement, the Pittsburgh sleep quality index (PSQI) scores at night, related complications, and satisfaction with care. Results. ① Postoperative anal pain was less severe in the study group than in the control group (P < 0.05). ② Postoperative comfort scores were higher in the study group than in the control group (P < 0.05). ③ The time to first bowel movement and its duration after surgery were shorter in the study group than in the control group (P < 0.05). ④ Patients in the study group had lower postoperative night-time PSQI scores than the control group (P < 0.05). ⑤ Patients in the study group had a lower rate of postoperative complications than the control group (P < 0.05). ⑥ Patients in the study group had higher postoperative care satisfaction scores than the control group (P < 0.05). Conclusion. The application of perioperative pain care management to patients undergoing anorectal surgery plays an important role in reducing anal pain, improving treatment comfort, and relieving difficult defecation symptoms, with significant improvement in postoperative sleep quality and reduction in complications. It is worthy of clinical reference and promotion.
1. Introduction
Department of Proctology is one of the most important departments in the hospital. The study of diseases that occur in the organs at the end of digestion, i.e., between 8 and 12 cm from the anal opening to the rectum, treats constipation, anal fistula, haemorrhoids, perianal abscesses, anal fissures, and rectal cancer, with a tendency to be located in the anus and rectum [1, 2]. With advances in medical care, many patients with anal diseases can be treated surgically with good results. However, it is inevitable that patients will experience a certain amount of pain, difficulty in defecation, and urinary retention during their postoperative recovery. In particular, the perianal skin is delicate and has a rich distribution of nerves and blood vessels, making the area more sensitive to pain, which can have a serious impact on wound recovery and even on the recovery of anal function if not treated properly [3, 4]. In response, some scholars [5, 6] have shifted the focus of their research towards the protocol of postoperative care in anal surgery, trying to find scientific and feasible nursing measures to improve patients’ symptoms of anal pain and defecation difficulties and to promote their prognosis in a comprehensive manner. It is thus clear that postoperative anal care measures are essential for a better recovery outcome. Pain care management is one of the widely used clinical models in recent years. With the goal of alleviating patients' pain, we provide services to patients in many aspects, with good results, which are recognized and praised by patients and their families.” [7, 8]. This paper discusses the specific measures and application value of perioperative pain care management in 126 patients treated with anorectal surgery in our anorectal surgery department from January to December 2021. The specific results are reported below.
2. Materials and Methods
2.1. General Data
A total of 126 patients who underwent anal surgery in our department from January to December 2021 were selected for the study. The inclusion criteria were as follows: ① those who met the diagnostic criteria for relevant anorectal diseases in anorectal pathology [9] and the indications for surgical procedures in practical anorectal surgery [10]; ② those who are 18–70 years old; ③ those with complete clinical information; and ④ those who voluntarily signed the informed consent form. The exclusion criteria were as follows: ① those with combined mental illness, impaired consciousness, speech impairment, or hearing impairment; ② those with organic pathology, cardiopulmonary, hepatic or renal insufficiency, coagulation disorders, or malignant tumours; ③ those who were transferred to another hospital midway, changed their surgical procedure, or lost contact during the follow-up period; and ④ those with inadequate treatment compliance. The patients were randomly divided into a study group and a control group of 63 cases each after consent was sought. The baseline data for both groups are shown in Table 1 and they were not significantly different and were comparable (P > 0.05).
| Data | Control group (n = 63) | Study group (n = 63) | t/χ2 | P |
|---|---|---|---|---|
| Age ( ± s, years old) | 46.98 ± 8.25 | 47.75 ± 10.12 | 0.480 | 0.632 |
| Disease duration ( ± s, years) | 3.37 ± 0.92 | 3.33 ± 1.08 | 0.224 | 0.823 |
| Male (n, %) | 34 (53.97) | 30 (47.62) | 0.508 | 0.476 |
| Disease classification (n, %) | 1.804 | 0.614 | ||
| Hemorrhoids | 24 (38.09) | 21 (33.33) | ||
| Anal fistula | 12 (19.05) | 15 (23.81) | ||
| Anal fissure | 15 (23.81) | 19 (30.16) | ||
| Anal stenosis | 12 (19.05) | 8 (12.70) |
2.2. Care Methods
Both the groups performed the relevant anal surgery with reference to the relevant protocols in practical anorectal surgery [10]. The control group used the conventional perioperative care protocol. Patients with a perianal disease had certain worries due to the specific location of the disease, so nursing staff were needed to treat the patients with enthusiasm and patience, explain relevant disease knowledge to them, help them to dispel their worries, and build up their confidence in treatment. The room was kept tidy, quiet, and comfortable with appropriate temperature and humidity. The patients were asked to wear loose cotton clothing and trousers and to change them daily. The patients were instructed to use soft toilet paper after defecation to avoid rubbing the wound and increasing the pain. The patients were instructed and provided help to prepare for the procedure, including skin preparation, a light diet, and oral polyethylene glycol electrolyte powder on the night before the procedure. Routine postoperative care measures such as timely administration of the medication, monitoring of signs, communication of medical advice, and discharge instructions were provided. The study group was given perioperative pain care management on top of the abovementioned care. The main contents are as follows specifically:
2.2.1. Formation of a Pain Care Management Team
The pain care management team was formed by the head of our anorectal department, consisting of experienced attending physicians and head nurses. The members were responsible for analysing the patient’s condition, formulating a pain prevention and management plan in conjunction with the clinical reality, updating and improving the plan to ensure its effective implementation and to improve the quality of pain management.
2.2.2. Organization of Training Activities for Members of the Pain Care Management Team
The training focused on the rational use of analgesic drugs, various modes of analgesic methods, and several measures to prevent wound infection. The training of nursing staff was regularly evaluated and the results were linked to their salaries, thus increasing their motivation to work.
2.2.3. Specific Implementation of Pain Care
① Dietary interventions: The patient’s diet was under strict control before and after the operation; the patients were strictly prohibited from consuming spicy, cold, greasy, and other foods to avoid stimulation of the gastrointestinal tract, especially for patients with haemorrhoids, before and after the operation, the diet should mainly contain liquid or semiliquid food, as far as possible to reduce the amount of bowel movements, in order to reduce the pain in the anus. During the later stages of hospitalisation, the diet was adjusted appropriately according to the patient’s recovery although no stimulating foods could be used, and vegetables and fruits of coarse fibre and that were easy to digest could be added appropriately. In addition, the nursing staff could communicate with the patients and adapt recipes to their daily dietary preferences to provide better quality care. ② Wound pain care: Postoperative caregivers needed to select a pain rating scale to assess the patient’s pain level on a continuous basis and make a dynamic scale of the specific data collected to reflect the various stages of the patient’s recovery. The nursing staff should give corresponding nursing care according to the specific pain degree of the patient. When the pain was mild, they could be instructed to choose the knee bending lateral position or deep breathing method to relieve the pain; when the pain was obvious, the attending doctor could be informed, and the patient could be given analgesic drugs in strict accordance with the doctor’s advice. At the same time, the patient should be warned not to stand for a long time during normal activities and should also avoid pulling the wound due to impulsive movement of the lower limbs. ③ Dressing change care: Regular postoperative wound dressing changes are required. Sitz bath fumigation was provided 30 minutes prior to dressing change to improve peri-incisional subcutaneous blood circulation and enhance the drug absorption. When changing the dressing, the exact location of the wound should be determined, the existing dressing should be removed with warm water and the skin should be wiped dry, and a new dressing should be applied, following aseptic standards to prevent postoperative infection. The movement in the process must be smooth and gentle, and the drainage gauze should be properly placed to avoid the pain caused by dressing and pressing. Attention should be paid to creating a private space for patients during the whole dressing change procedure. ④ Functional exercise: In the recovery stage, the nursing staff should guide the patients to carry out the corresponding rehabilitation training, including moderate simple exercises such as raising and shrinking the anus. During exercise, the nursing staff should help the patient to maintain a state of muscular and psychological relaxation, with a variety of options such as autonomous deep breathing, distraction methods and if necessary, music or television programmes. It was important to advise the patient to pay attention to the strength of the muscle contraction during the specific exercise and not to rush it, but to gradually increase the strength of the contraction to ensure that the wound could adapt to the intensity of the exercise. If pain was felt in the wound during training, it was necessary to stop immediately and continue only after the pain has disappeared; if the pain was not relieved for a long time, the wound was needed to be checked for secondary tears and treated promptly. ⑤ Defecation care: Creating a private space for patients to defecate, eliminating their nervousness, shyness, and embarrassment, etc., and promoting smooth bowel movements; patients were advised not to squat/sit for long periods of time when toileting and not to use excessive force to avoid retearing the wound and increasing perianal pain; it was important to clean thoroughly after defecation and to maintain anal and perianal hygiene and to take one to two sitz baths per day as directed by your doctor to reduce the risk of infection and relieve pain. ⑥ Psychological care: Some patients had severe postoperative pain that was also associated with factors such as psychological cues. For those with such tendencies, caregivers could eliminate the negative effects of tension, anxiety, fear, and other negative emotions on postoperative pain through music therapy and distraction methods to increase their comfort with treatment and improve their satisfaction with care. Nursing staff could also introduce patients to success stories on the ward to help build their confidence in recovery in a patient-directed way, as well as increase the communication between patients and alleviate negative psychology.
2.2.4. Regular Induction of Management Effects
At regular intervals, patient feedback was used to assess the content of nursing care and to identify the oversights and shortcomings during the work and improve them. The nursing staff were rewarded for excellent performance with pay and goods to stimulate their motivation and enthusiasm for their work. Nursing staff who performed poorly were punished with verbal criticism or bonuses. In this way, the management was improved and quality care was provided to patients.
2.3. Assessment Indicators
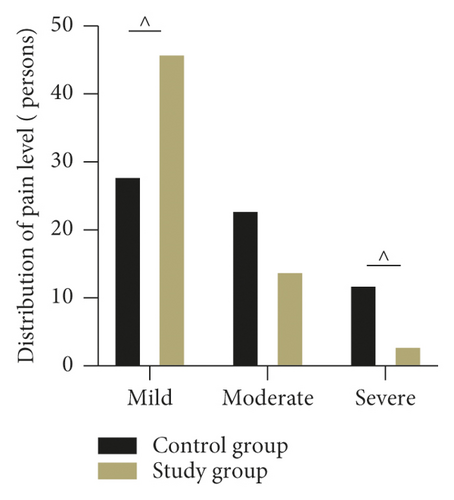
2.3.1. Pain Level
The verbal rating scale (VRS) [11] was used as the basis for postoperative anal pain grading in both groups. 0 level: no pain; mild: tolerable pain, not disturbed sleep; moderate: unbearable pain, disturbed sleep; and severe: severe pain, unbearable, severely disturbed sleep, may be accompanied by autonomic disturbance or passive body position.
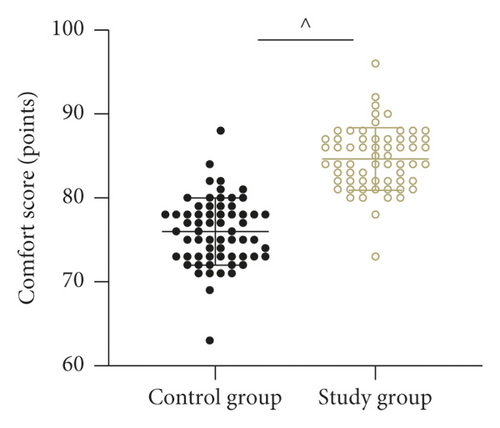
2.3.2. Comfort Score
Kolcaba’s general comfort questionnaire (GCQ) [12, 13] was used to evaluate the comfort level, which consisted of 30 questions on the following four dimensions: environmental, physical, psychological, and sociocultural comfort, using a 1–4 Likert scale, with a total score of 30–120. The higher the score, the higher the comfort level.
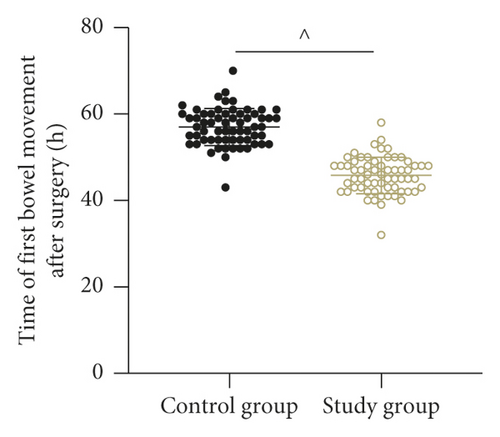
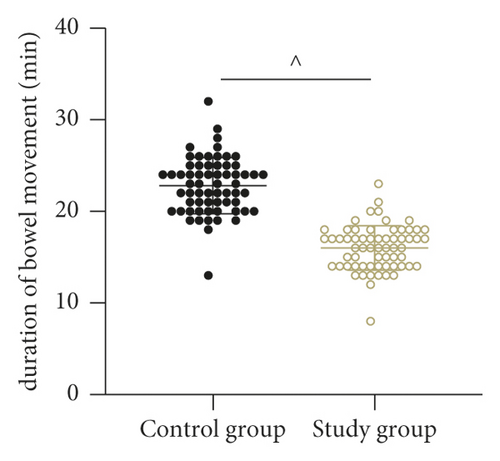
2.3.3. Defecation
The time to first bowel movement and duration of bowel movement after surgery were compared between the two groups.
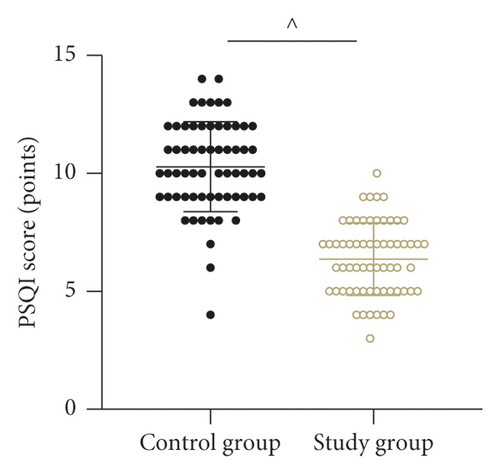
2.3.4. Sleep Quality Score
The Pittsburgh sleep quality index (PSQI) [14] was used to assess the quality of sleep at night after surgery, with a total score of 0–21, with higher scores indicating poorer sleep quality.
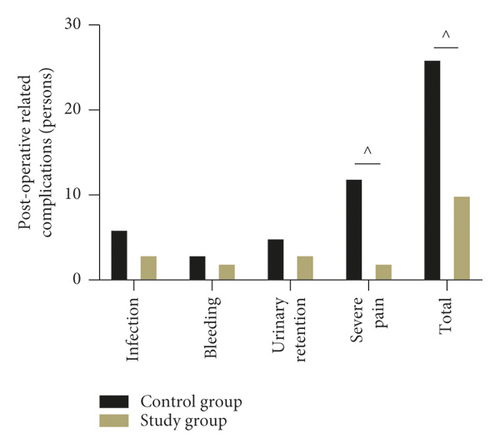
2.3.5. Complications
The occurrence of complications related to the care period was compared between the two groups.
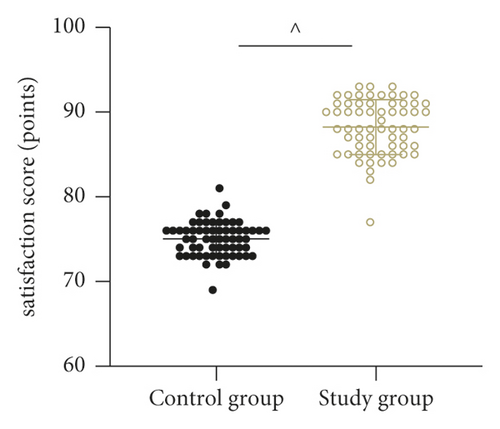
2.3.6. Satisfaction
The self-made nursing satisfaction scale in hospital was used as the basis for assessing satisfaction with nursing care, which consisted of 24 items; all assessed on a 5-point scale from 0 to 4, with a total score of 0–96, the higher the score, the better the satisfaction with nursing care.
2.4. Statistical Methods
The statistics and validation of this care outcome were completed by using the SPSS 20.0 statistical software. The measurement data were expressed as ( ± s) by the t test and the count data were described as (%) by the χ2 test, with P < 0.05 being a statistically significant difference.
3. Results
3.1. Comparison of the Postoperative Anal Pain Level within the Two Groups
Postoperative anal pain was less severe in the study group than in the control group (P < 0.05). See Figure 1.
3.2. Comparison of Postoperative Comfort Scores within the Two Groups
Postoperative comfort scores were higher in the study group than in the control group (P < 0.05). See Figure 2.
3.3. Comparison of Postoperative Bowel Movements within the Two Groups
The time to first bowel movement and its duration after surgery were shorter in the study group than in the control group (P < 0.05). See Figures 3 and 4.
3.4. Comparison of Postoperative Night-Time PSQI Scores within the Two Groups
Patients in the study group had lower postoperative night-time PSQI scores than the control group (P < 0.05). See Figure 5.
3.5. Comparison of Postoperative Complications within the Two Groups
Patients in the study group had a lower rate of postoperative complications than the control group (P < 0.05). See Figure 6.
3.6. Comparison of Care Satisfaction Scores within the Two Groups
Patients in the study group had higher postoperative care satisfaction scores than the control group (P < 0.05). See Figure 7.
4. Discussion
Pain is an unpleasant sensory and emotional experience that occurs when the body is injured and is accompanied by existing or latent tissue damage [15, 16] . Although anorectal disease is less likely to endanger patients’ lives, the special anatomical site of the anal canal, with its high distribution of blood vessels and nerves, the release of postoperative inflammatory mediators, perianal tissue oedema, bowel irritation, psychological factors, and medication changes by health care workers can all irritate the patient’s wounds and lead to severe postoperative pain [17, 18]. Also, due to the high level of bacteria in the anorectal area, frequent dressing changes are required to prevent infection of the wound, which aggravates the patient’s postoperative pain. Postoperative pain can also lead to poor defecation, affecting the body’s neuroendocrine system and prompting a series of stress reactions, with patients suffering from constipation and difficult defecation in mild cases, or impaired digestion, cardiac arrhythmia, and even cardiac arrest in severe cases [19, 20]. The abovementioned scenarios will not only affect the patient’s normal life but also cause physical and mental disorders, which are detrimental to the patient’s prognosis level and quality of life.
In the conventional model of care, the healthcare provider only pays attention to the changes associated with the patient’s incision after surgery. Pain management, on the other hand, means caring for the patient’s postoperative incision recovery status while also being mindful of the patient’s physical and mental health, resulting in a significant reduction in pain and a further increase in patient comfort. In recent years, our department has advocated the implementation of pain care management for surgical patients, focusing on six aspects of dietary intervention, wound pain care, dressing change care, functional exercise, bowel care, and psychological care. It is also a continuous process of improvement and refinement of care measures, with the main aim of reducing anal pain triggers and adverse factors affecting the wound recovery, in order to provide a more detailed, quality and comfortable healthcare experience for patients.
The results of this study showed that patients in the study group who were managed with timely pain care after surgical treatment had significantly better pain relief, postoperative comfort, bowel movement, and sleep quality than the control group who were treated with routine perioperative care during the same period and that the study group had fewer postoperative complications and higher patient satisfaction, making it more valuable. Possible reasons for the analysis of the above results are the following: ① enhanced postoperative dietary interventions not only avoid painful irritation from irritating foods but also reduce the risk of haemorrhoids and are beneficial in enhancing the prognosis of patients; ② anal function training can be done by lifting and retracting the anal sphincter to promote postoperative smooth bowel movements and to reduce the anal stimulation caused by the prolonged toilet time and the retearing of the anal opening caused by difficult defecation, so as to reduce the pain symptoms; ③ trauma pain care through the development of a dynamic pain score scale, which allows healthcare professionals to understand the patient’s specific situation at each stage of recovery in real time and to provide appropriate care and pain relief instructions; ④ during dressing change care, attention is paid to maintaining appropriate strength and protecting the wound, as well as to the psychological needs of the patient, focusing on the protection of the patient’s privacy, so that the patient is more receptive psychologically, reducing the sense of rejection and facilitating the postoperative rehabilitation treatment; ⑤ the study also improved the quality of patients’ prognosis through defecation instructions, which consisted of three components: creating a private space, controlling the intensity of defecation, and cleaning after defecation to shorten the defecation time improve the incidence of complications such as infection and pain, and to improve the quality of care from both a physical and psychological perspective; and ⑥ given that 60% of the patients’ postoperative pain levels were related to their poor psychological cues, the nursing staff in this study alleviated the patients’ adverse emotions by means of positive psychological suggestion, distraction, and playing soothing music to improve the adverse effects of adverse emotions on pain, thereby reducing postoperative pain symptoms and improving the prognosis. Finally, by waiting for the regular summarisation and assessment of nursing work content, this study records the various problems that arise in clinical work, considers the subsequent improvement plans, and links the assessment results and management effects with the performance of nursing staff, which helps the continuous self-reflection and self-improvement of medical and nursing staff, and ultimately improves the level of nursing management and the quality of nursing services.
5. Conclusion
The application of perioperative pain care management to patients undergoing anorectal surgery has an important role in reducing anal pain, improving treatment comfort, and relieving difficult defecation symptoms, with significant improvement in postoperative sleep quality and reduction in complications. It is worthy of clinical reference and promotion.
Disclosure
Yimei Liao and Jing Jiang are co-first authors.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Open Research
Data Availability
The primary data used to support the results of this study are available on reasonable request to the corresponding author.