Dance Is an Accessible Physical Activity for People with Parkinson’s Disease
Abstract
Objective. To evaluate the outcomes of face-to-face, digital, and virtual modes of dancing for people living with Parkinson’s disease (PD). Design. Systematic review informed by Cochrane and PRIMSA guidelines. Data Sources. Seven electronic databases were searched: AMED, Cochrane, PEDro, CINHAL, PsycINFO, EMBASE, and MEDLINE. Methods. Eligible studies were randomised controlled trials (RCT) and other trials with quantitative data. The PEDro scale evaluated risk of bias for RCTs. Joanna Briggs Institute instruments were used to critically appraise non-RCTs. The primary outcome was the feasibility of dance interventions, and the secondary outcomes included gait, balance, quality of life, and disability. Results. The search yielded 8,327 articles after duplicates were removed and 38 met the inclusion criteria. Seven were at high risk of bias, 20 had moderate risk of bias, and 11 had low risk of bias. There was moderately strong evidence that dance therapy was beneficial for balance, gait, quality of life, and disability. There was good adherence to digital delivery of dance interventions and, for people with PD, online dance was easy to access. Conclusion. Dancing is an accessible form of exercise that can benefit mobility and quality of life in people with PD. The COVID-19 pandemic and this review have drawn attention to the benefits of access to digital modes of physical activity for people living with chronic neurological conditions.
1. Introduction
Parkinson’s disease (PD) is a debilitating and progressive condition that currently has no cure. People living with PD can experience movement disorders and nonmotor symptoms that compromise their levels of physical activity [1] and quality of life [2–5]. Movement slowness [6], balance impairment [7], falls [8, 9], and gait disturbance often occur [10]. These movement disorders, coupled with anxiety, depression, or lethargy, can be major barriers to maintaining long-term engagement in physical activity [1].
Structured exercises and physical activities can assist people with chronic diseases to keep moving and to stay engaged in social activities and recreational sports [1]. One of the challenges for practitioners is keeping people with Parkinson’s motivated to adhere to regular physical activities over long periods of time [1]. People typically live with PD for 7–25 years [11, 12], and clinical guidelines recommend daily physical activities for at least 30–45 minutes per session [13]. For progressive conditions such as PD, it is recommended that a range of therapeutic exercises is available, to maintain long-term exercise adherence and compliance [1, 14]. There is evidence that people in the early to midstages of Parkinson’s can benefit from progressive resistance strength training [8, 15, 16], cueing [10,15], aqua therapy [17], physiotherapy [18, 19], aerobic exercises [20], Nordic walking [21], community walking [22], assisted cycling [23], boxing [24], and tai chi [25]. Therapeutic dancing is another option, given that it is engaging and can be done in groups or individually [26–28].
Dancing for people with PD aims to improve movement, wellbeing, and quality of life, as well as social engagement and exercise capacity [29–32]. Dance also allows for creative expression and can take the focus off the disease and onto movement to music and social connection [31,33,34]. A study by Dos Santos Delabary et al. [35] reported that dance sometimes has greater benefits for functional mobility and motor symptoms than usual care. Likewise, Shanahan et al. [36] noted that participation in dance can improve endurance, motor impairment, and balance for those with mild to moderate PD. Berti et al. [37] reported that adapted tango dance programs are an effective intervention for individuals with PD with a range of abilities and balance limitations.
Given the need for people with Parkinsonism and related disorders to have a range of evidence-based exercise choices, the primary aim was to evaluate the outcomes of face-to-face, online, and virtual modes of therapeutic dancing as an accessible physical activity for people living with PD. The outcomes of particular interest were balance, gait, disability, and quality of life.
2. Methods
We conducted a systematic review of the literature following a priori methods. Two independent reviewers (SE, HH) were involved in the selection of studies into the review and two independent reviewers (SE, DJ) completed the data extraction to ensure that all relevant studies were identified, and that data were extracted reliably and consistently [38]. The review was informed by Cochrane guidelines and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist [39].
The search was conducted using seven electronic databases: AMED, Cochrane, PEDro, CINHAL, PsycINFO, EMBASE, and MEDLINE. The search terms included: Parkinson disease or Parkinson’s disease or Parkinson∗, movement disorders and dance therapy or dancing or dance based or danc∗ or foxtrot or tango or waltz or “Irish set” or ballroom or dance movement therapy or contemporary salsa or cultural and telerehabilitation or telemedicine or telehealth or tele or remote or online or web-based or virtual or in-person or pre-recorded or live or synchronous or asynchronous or partnered or on-partnered and quality of life or balance or gait or disability. The MEDLINE strategy was adapted to the other databases and search strategies are available on request. An example of the Medline search strategy is in Table 1. The searches were conducted by a health sciences librarian up until June 2020, saved in each database, and downloaded into the bibliographic management software program Endnote [40, 41]. Search yields were combined into one Endnote library, and duplicates were deleted prior to application of the eligibility criteria to the titles.
| Search ID# | Search terms | Search notes | Results |
|---|---|---|---|
| 1 | Exp Parkinson disease, secondary/or exp Parkinson disease/ | 70995 | |
| 2 | Parkinson∗.mp. | 127920 | |
| 3 | Exp stroke/or exp stroke rehabilitation/ | 136433 | |
| 4 | (Stroke or strokes).mp. | 295325 | |
| 5 | Exp Multiple sclerosis/ | 58198 | |
| 6 | “Multiple sclerosis”.mp. | 82515 | |
| 7 | 1 or 2 or 3 or 4 or 5 or 6 | 519376 | |
| 8 | Exp dance therapy/ | 359 | |
| 9 | Exp dancing/ | 2848 | |
| 10 | (Dance∗ or dance-based or dancing).mp. | 7345 | |
| 11 | (Foxtrot or tango or Waltz or “Irish set” or ballroom or ballet).mp. | 2113 | |
| 12 | Or/8–11 | Dance related terms | 8348 |
| 13 | Exp exercise movement techniques/ | 8116 | |
| 14 | physiotherap∗.mp. | 26124 | |
| 15 | Exp exercise therapy/ | 50130 | |
| 16 | Exp exercise/ | 192926 | |
| 17 | exercis∗.ti,ab. | 290086 | |
| 18 | Or/13–17 | Exercise/physio related terms | 431332 |
| 19 | 12 or 18 | Included dance and physio/exercise terms | 438077 |
| 20 | Exp telemedicine/or exp telerehabilitation/ | 27950 | |
| 21 | telerehabilitation.mp. | 933 | |
| 22 | tele.mp. | 3173 | |
| 23 | (Remote adj3 rehabilitat∗).mp. | 87 | |
| 24 | telehea∗.mp. | 4922 | |
| 25 | app.mp. | 25736 | |
| 26 | ((Exercise or mode) adj2 delivery).mp. | 8376 | |
| 27 | virtual.mp. | 59008 | |
| 28 | video.mp. or exp video recording/or tape recording/or videotape recording/ | 148947 | |
| 29 | (Online or “online”).ti,ab. | 137403 | |
| 30 | telemedicine.mp. | 27556 | |
| 31 | Exp telemedicine/ | 27950 | |
| 32 | (Telemonitor∗ or tele-monitor∗).mp. | 1706 | |
| 33 | Internet.mp. | 102501 | |
| 34 | ((Tele∗ adj2 coach∗) or telecoach∗).mp. | 374 | |
| 35 | videoconferenc∗.mp. | 2843 | |
| 36 | ipad.mp. | 1300 | |
| 37 | computer.mp. | 693528 | |
| 38 | Exp internet/or exp internet-based intervention/ | 78406 | |
| 39 | Mobile applications/ | 5683 | |
| 40 | (Apps or “mobile applications”).mp. | 10631 | |
| 41 | zoom.mp. | 1600 | |
| 42 | webinar∗.mp. | 569 | |
| 43 | (Live adj2 stream∗).mp. | 148 | |
| 44 | Web-based.mp. | 30097 | |
| 45 | Pre-record∗.mp. | 363 | |
| 46 | (Dvd adj2 deliv∗).mp. | 31 | |
| 47 | Or/20–46 | 1110851 | |
| 48 | 7 and 19 and 47 | Final results | 1903 |
| 49 | recorded.mp. | 525831 | |
| 50 | synchronous.mp. | 35231 | |
| 51 | asynchronous.mp. | 9988 | |
| 52 | 49 or 50 or 51 | 566263 | |
| 53 | 7 and 19 and 52 | Testing results for synchronous/asynchronous. | |
| Or recorded | 1204 |
Inclusion and exclusion criteria were firstly applied to the titles to exclude studies that were clearly ineligible. We then applied the eligibility criteria to the titles and abstracts (SE, HH). Two reviewers (SE, HH) independently read in full the remaining articles to determine whether they met the eligibility criteria. A third reviewer (SS) was consulted to reach consensus if needed. Remaining discrepancies were resolved through consensus by two final reviewers (MM, MH) to determine the final included studies.
2.1. Inclusion Criteria
2.1.1. Study Designs
The study designs included randomised controlled trials (RCT) and nonrandomised trials that contained data. We deliberately included both randomised and nonrandomised trials, to extend the findings of systematic reviews, which were confined to RCTs (e.g., 35–37). The full text had to be available and accessible in English. Systematic reviews, meta-analyses, protocol papers, letters to the editor, conference posters, opinion pieces, and abstracts were excluded.
2.1.2. Participants
Participants had to have a diagnosis of PD. Other chronic neurological, musculoskeletal, or respiratory conditions were excluded, as well as dementia and Alzheimer’s disease. Individuals were at any stage of PD classified by the modified Hoehn and Yahr Scale [42] and living in residential care or the community. Adults of all ages, genders, and many cultures were included.
2.1.3. Interventions
Studies were included if they used dance as an exercise intervention or form for physical activity or physiotherapy. All genres of dance were eligible, including Irish-set dancing, tango, waltz, tap, jazz, salsa, ballroom, ballet, mixed genre, and creative dancing. Classes could be delivered partnered or nonpartnered, group or one to one and with or without music. The mode of delivery was in-person, digitally (also known as online), or using virtual tools. Online delivery was via platforms such as Zoom® or Microsoft Teams®. Some of the dance interventions were delivered by dance teachers and others were delivered using “virtual” tools such as Wii (Nintendo Inc., Japan) or Sony Play Station® video game systems. The criteria for comparison or control interventions were any “usual care” or “usual physical activity” condition or any other therapeutic intervention.
2.1.4. Outcomes
Studies were selected if they included baseline and after intervention outcomes for any of the following variables: gait, balance, movement, mobility, movement disorders, nonmotor symptoms, disability, participation, quality of life, wellbeing, or social participation. Feasibility studies were also reviewed.
2.1.5. Risk of Bias
The PEDro scale was used to determine the risk of bias for RCTs [43]. PEDro was selected as it is a valid and reliable appraisal instrument for RCTs [44, 45]. Joanna Briggs Institute (JBI) instruments were used to critically appraise nonrandomised studies and to determine their risk of bias [46, 47]. Risk of bias assessments were completed independently by two reviewers (SE, SS), and consensus was reached by consultation with the research team (MM, MH).
2.1.6. Data Extraction
Reviewers (SE, DJ,) independently extracted data into a pretested spreadsheet under headings such as study, participant and intervention characteristics, and outcome data. The data were independently screened and confirmed (SS, MEM). Outcome data were extracted for short-, medium-, and long-term follow-up assessments when reported.
2.1.7. Data Analysis
For quantitative data, summary statistics were calculated. For the RCTs, the reported means and standard deviations were tabulated, and the Hedge’s g, bias-corrected effect size (ES) index was used to estimate the effects of dancing compared to another intervention or no therapy [48]. In some cases, the ES was already reported as a standardized mean difference (SMD) or Cohen’s d [49, 50] which we used. The Hedge’s g and Cohen’s d are similar; the Hedge’s g tends to perform better with sample sizes lower than 20. Whenever possible, a 95% confidence interval (95% CI) was calculated around the SMD for an estimate of the range of intervention effects [51]. Median scores and interquartile ranges (IQR), reported by the study authors, were also tabulated [52]. To facilitate comparisons across studies, median scores were entered into SMD calculations as best estimates of mean scores [53]. For non-RCTs, within-group mean differences and change scores were reported and effect sizes calculated whenever possible.
3. Results
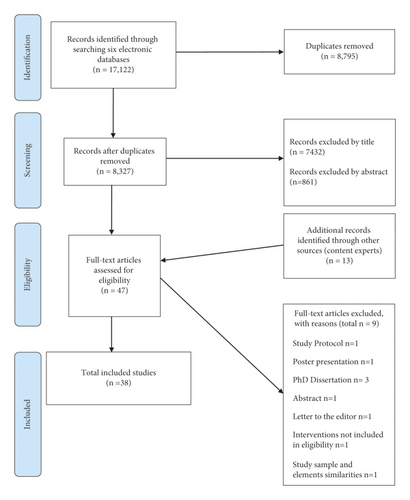
Of the initial yield of 17,122, there were 8,327 remaining after duplicates were removed. Screening of the articles was conducted by two independent reviewers (SE, HH) with 34 articles initially assessed for eligibility. A third reviewer (SS) was consulted to check the findings and reach consensus and 13 additional articles were added by members of the research team (MM, MH). From the articles read in full, 9 were excluded because they did not meet the eligibility criteria. Final consensus was reached in consultation with MM and MH, yielding a total of 38 articles. Figure 1 shows the PRISMA-compliant flowchart for selection of studies [39]. Of the included studies, 17 were RCTs [26, 27, 30, 54–67]. One of these was a sequential RCT [66], one was a quasi-RCT [67], and one was an RCT with a crossover design [63] (Table 2). Of the trials, 21 had nonrandomised designs [28, 68–87], and one of these was a quasiexperimental study [81]. One used mixed methods design [82] for which quantitative data were extracted and analysed. Also, one was an exploratory trial [87] and there was an additional single case study [88]. (Table 2).
| First author, year | Study design | Sample size | Interventions | Age (years) mean ± SD Sex (M, F) |
H&Y mean ± SD, range, or median (IQR) | Session length, frequency, intervention duration | Medications | Outcome measures | |
|---|---|---|---|---|---|---|---|---|---|
| Randomised studies | |||||||||
| Duncan and Earhart, 2012 [62] | RCT | 62 | Argentine Tango |
|
2.6 ± 0.1 | 1 hr class, 2/week, 12 months | Not reported but tested in the “off phase” | UPDRS-II, UPDRS-III, FOG, 6MWT, MiniBEST, gait velocity | |
| Control, no dance |
|
2.5 ± 0.1 | |||||||
| Duncan and Earhart, 2014 [54] | RCT | 10 | Argentine Tango |
|
2.4 | 1 hr, 2/week, 2 years | Levodopa | UPDRS-I, UPDRS-II, UPDRS-III, MiniBEST, gait velocity, TUG, dual-task TUG, 6MWT, FOGQ | |
| Control, no dance |
|
2.3 | |||||||
| Kunkel et al., 2017 [55] | RCT | 51 | Dance (mixed genre) |
|
1–3 | 1 hr, 2/week, 10 weeks | Not reported | BBS, SS180, TUG, 6MWT, Phone-FITT, EQ-5D, ABC | |
| Control, no dance |
|
1–3 | |||||||
| Hackney and Earhart, 2010 [60] | RCT | 39 | Partner dancing |
|
2-3 | 1 hr, 2/week, 10 weeks | Levodopa | UPDRS-III, BBS, tandem stance, one leg stance, TUG, 6MWT, gait measures | |
| Nonpartner dancing |
|
2-2.6 | |||||||
| Hackney and Earhart, 2009 [61] | RCT | 58 | Waltz/foxtrot |
|
2.0 ± 0.2 | 1 hr, 2/week, 13 weeks | Levodopa | UPDRS-III, BBS, TUG, 6MWT, gait measures, FOGQ | |
| Tango |
|
2.1 ± 0.1 | |||||||
| Control, no dance |
|
2.2 ± 0.2 | |||||||
| Hackney et al., 2007 [59] | RCT | 19 | Tango |
|
2.3 ± 0.7 | 1 hr, 2/week, 13 weeks | PD medications | UPDRS-III, BBS, gait velocity, TUG, FOGQ | |
| Group exercise class |
|
2.2 ± 0.6 | |||||||
| Hashimoto et al., 2015 [67] | Quasi-RCT | 46 | PD dance |
|
Score 2 (11) | 60 min class, 1/week, 12 weeks | Not reported | TUG, BBS, UPDRS, SDS, FAB, Mental Rotation Task, Apathy Scale | |
| PD exercise |
|
Score 3 (33) | 60 min class, 1/week, 12 weeks | ||||||
| Control, usual care |
|
Score 4 (2) | |||||||
| Lee et al., 2015 [57] | RCT | 20 | Virtual reality dance |
|
Not reported | 30 mins, 5/week, 6 weeks | Not reported | BBS, BDI, MBI | |
| Control |
|
||||||||
| Lee et al., 2018 [63] | RCT with cross-over design | 32 | Qigong dance |
|
1–3 | 60 min, 2/week, 8 weeks | Not reported | UPDRS, PDQL, BBS, BDI | |
| Control, wait list |
|
1–3 | |||||||
| McKee and Hackney, 2013 [66] | Sequential RCT | 33 | Tango |
|
2.3 (2.0-2.6) | 90 mins, 20 sessions, 12 weeks | PD medications | UPDRS-III, Four-Square Step Test, TUG, dual-task TUG, PDQ-39, FOGQ, SFHS-12 | |
| Lecture series |
|
2.0 (2.0- 2.0) | |||||||
| Michels et al., 2018 [30] | Pilot RCT | 13 | Dance therapy |
|
|
60 mins, 1/week, 10 weeks | Stable PD medication regimen | UPDRS, MOCA, TUG, BBS, BDI, FSS, Visual Analog Fatigue Scale, PDQ-39 | |
| Control, support group | |||||||||
| Poier et al., 2019 [64] | Pilot RCT | 29 | Argentine Tango |
|
Not reported | 60 min class, 1/week, 10 weeks | Not reported | PDQ-39, BMLSS, ICPH | |
| Control, Tai Chi |
|
||||||||
| Rocha et al., 2018 [27] | Pilot RCT | 21 | Argentine Tango |
|
1–4 |
|
PD medication | TUG, BBS, functional gait assessment, FOGQ, UPDRS-II and -III, PDQ-39 | |
| Mixed dance |
|
||||||||
| Rio Romenets et al., 2015 [58] | RCT | 33 | Argentine Tango |
|
2 ± 0.5 | 1 hr, 2/week, 12 weeks | Not reported | UPDRS-III, UPDRS, MiniBEST, TUG, dual-task TUG, BDI, Apathy Scale, KFSS, PDQ-39, CGI-C, FOGQ, Falls Questionnaire, MOCA | |
| Control |
|
1.7 ± 0.6 | |||||||
| Shanahan et al., 2017 [26] | RCT | 41 | Set dancing |
|
1.25 ± 1 | In-person: 1 hr, 1/week | Not reported | UPDRS-III, 6MWT, MiniBEST, PDQ-39 | |
| Control, usual care and ADL |
|
2 ± 1 | Home: 20 mins, 3/week, 10 weeks | ||||||
| Solla et al., 2019 [56] | RCT | 20 | Sardinian folk dance |
|
2.1 ± 0.6 | 90 mins, 2/week, 12 weeks | PD medications | UPDRS-III, 6MWT, BBS, TUG, Parkinson’s Disease Fatigue Scale, BDI, Starkstein Apathy Scale, MOCA | |
| Control, usual care |
|
2.3 ± 0.4 | |||||||
| Volpe et al., 2013 [65] | RCT: single blind, parallel group | 24 | Intervention: Irish set dancing |
|
2.2 ± 0.4 | 90 min classes, 1/week, 6 months |
|
UPDRS-III, BBS, FOG, PDQ-39 | |
| Control: physiotherapy (balance, cueing, gait training, strength) |
|
2.2 ± 0.4 | 90 mins, 1/week, 6 months, 1 hr weekly home video | ||||||
| Nonrandomised studies | |||||||||
| Albani et al., 2019 [68] | Single group, pre-post design, feasibility | 10 | Tango-based home exercises and group sessions |
|
2-3 |
|
Not reported | Gait measures (fully cued visual four-choice reaction-time tasks, simple reaction-time task, an uncued task, two partially cued tasks), UPDRS | |
| Batson, 2010 [77] | Single group, pre-post design | 11 | Modern dance |
|
1-2.5 | 85 min class 3/week, 3 weeks |
|
TUG, FAB | |
| Blandy et al., 2015 [70] | Single group, pre-post design | 6 | Argentine Tango |
|
2 (2-2) | 1 hr, 2/week, 4 weeks | “ON” phase of medication | EQ-5D, Visual Analogue Scale, BDI | |
| Dahmen-Zimmer and Jansen, 2017 [69] | Pre-post design, pilot trial | 37 | Karate (Shotokan) |
|
1–3 | 1 hr, 1/week, 30 weeks | Not reported | Multidimensional Mood State Questionnaire, Hospital Anxiety and Depression Scale, CEDS Depression Scale, SFHS-12, Short Scale Of General Self-Efficacy | |
| Dance (mixed genre) |
|
||||||||
| Control (waitlist) |
|
||||||||
| Delextrat et al., 2016 [71] | Single group, pre-post design, feasibility | 11 | Zumba |
|
<3 | 45 mins–1 hr, 1/week, 6 weeks | Not reported | Enjoyment, change in physical activity, exercise intensity (accelerometry), heart rate, rated perceived exertion | |
| Hackney and Earhart, 2009 [72] | Single group, pre-post design | 14 | Argentine Tango |
|
2.4 (25%:2.0; 75%:2.5) | 1.5 hrs, 5/week, 2 weeks | Not reported | UPDRS-III, BBS, TUG, 6MWT, gait measures | |
| Hackney and McKee, 2014 [28] | Single group, pre-post, pilot trial | 88 | Argentine Tango (PD) |
|
1–3 | 1.5 hrs, 2/week for 12 weeks | PD medication | UPDRS-III, BBS, TUG, gait speed assessment, 30 second chair stand, tandem stance | |
| Older adults (non-PD) |
|
||||||||
| Heiberger et al., 2011 [78] | Single group, pre-post design | 11 | Mixed genre dance |
|
Moderate to severe 2.5–4 | 1/week class, 8 months | L-Dopa or dopamine agonists | UPDRS-III, TUG, QOLS, Westheimer Questionnaire | |
| Kalyani et al., 2019 [81] | Quasiexperimental design | 33 | Dance (mixed genre) |
|
1.65 ± 0.79 | 1 hr, 2/week, 12 weeks | Not reported | UPDRS-I, UPDRS-II, PDQ39 | |
| Control |
|
1.56 ± 0.81 | |||||||
| Listewnik and Ossowski, 2018 [75] | Single group, pre-post design | 10 | Dance |
|
— | 70 mins, 2/week for 12 weeks | Not reported | Tinetti POMA Test, TUG, 6MWT | |
| McGill et al., 2018 [85] | Non-RCT | 32 | Ballet |
|
2.32 ± 0.48 | 1.25-1.5 hrs, 1/week for 1 year | Not reported | Step and stride variability, ABC | |
| Control |
|
2.15 ± 0.55 | |||||||
| McKay et al., 2016 [80] | Single group study | 22 | Adapted Tango |
|
1–4 | 90 mins, 15 lessons over 3 weeks | Not reported | UPDRS, dyskinesia, BBS, Dynamic Gait Index, FAB, musculoskeletal health, 6MWT, single and dual-task TUG, fast and preferred cadence, ABC, FOGQ | |
| McNeely et al., 2015 [74] | Pre-post design | 16 |
|
|
2.25 ± 0.27 | 1 hr group class, 2/week, 12 weeks | Levodopa | UPDRS-III, MiniBEST, TUG, dual-task TUG, 6MWT, gait velocity | |
|
2.13 ± 0.58 | ||||||||
| McRae et al., 2018 [87] | Exploratory study, surveys | 61 | Dancing for Parkinson’s Disease (mixed genre) |
|
1–4 | 1-2/week, 12 months (6months–2 years), session length unknown | Not reported | 36-Item Short Form Health Survey, Self-Efficacy Scale, functional mobility | |
| Marchant et al., 2010 [79] | Single group, pre-post design | 11 | Improvisation dance |
|
2.4 ± 0.4 | 10 1.5-hour classes, 2 weeks | PD medication | UPDRS-III, BBS, TUG, gait measures, Five Times Sit-to-Stand Test, 6MWT, FOGQ, ABC, PDQ-39 | |
| Rawson et al., 2019 [86] | Nonrandomised controlled | 96 | Tango vs treadmill vs control (stretching) |
|
1–4 | 1 hr class, 2/week, 12 weeks | Levodopa | UPDRS-III, PDQ-39, 6MWT, MiniBEST, gait measures | |
| Seidler et al., 2017 [84] | Non-RCT | 26 | Telerehab dance |
|
1–3 | 1 hr, 2/week, 12 weeks | Not reported | MiniBEST, UPDRS-III, gait velocity | |
| In-person dance |
|
||||||||
| Shanahan et al., 2015 [76] | Single group, pre-post pilot trial | 10 | In-person and home-based dance programs |
|
1.5 ± 0.5 |
|
Not reported | UPDRS, 6MWT, BBS | |
| Tillmann et al., 2020 [83] | Non-RCT | 47 | Brazilian samba |
|
1.8 ± 0.7 | 1 hr, 2/week, 12 weeks | 4 months stable medication | PDQ-39, PDSS, BDI, FSS, UPDRS-I | |
| Control |
|
||||||||
| Tunur et al., 2020 [73] | Pre-post -mixed methods | 7 | Google glass dance modules |
|
2–3 | 3+ modules/day, 3 weeks. Session length not reported | Not reported | MiniBEST, one leg stance, TUG, dual-task TUG, ABC, BDI, PDQL | |
| Zafar et al., 2017 [82] | Pre-post design | 88 | Adapted Tango (PD) |
|
1–3 | 90 min, 2/week, 12 weeks | PD medication | Fear of falling, quality of life, composite physical function, MOCA, BDI, UPDRS-III, gait velocity, Impact on Participation and Autonomy Questionnaire | |
| Adapted Tango (non-PD) |
|
||||||||
- Note: 6MWT, Six-Minute Walk Test; ABC, Activities-Specific Balance Confidence Scale; BBS, Berg Balance Scale; BDI, Beck Depression Inventory; EQ-5D, EuroQol-5 Dimension; FAB, Fullerton Advance Balance Scale; FOGQ, Freezing of Gait Questionnaire; FSS, Fatigue Severity Scale; HADS, Hospital Anxiety and Depression Scale; KFSS, Krupp Fatigue Severity Scale; MiniBEST, Mini-Balance Evaluation Systems Test; MBI, Modified Barthel Index; MOCA, Montreal Cognitive Assessment; PDQ-39, Parkinson’s Disease Questionnaire-39; PDSS, Parkinson′s Disease Sleep Scale; RCT, Randomised Controlled Trial; SDS, Self-Rating Depression Scale; SFHS-12, Short Form Health Survey-12; SS180, Standing-Start 180° Turn Test; Tinetti POMA Test, Tinetti Performance-Oriented Mobility Assessment Test; TUG, Timed Up and Go; UPDRS, Unified Parkinson’s Disease Rating Scale.
The included studies ranged in sample size from 6 to 96 participants (Table 2). Only 3 studies included either telehealth [84] or technology-based interventions that included virtual reality dancing [57] or dance Google glass modules [73]. Dance interventions included tango [27, 28, 54, 55, 58, 59, 60–62, 64, 66, 68, 70, 72, 80, 82, 86], Sardinian folk dancing [56], Irish set dancing [26, 65], waltz/foxtrot [55, 61], ballet [85], Brazilian Samba [83], Zumba [71], Qigong dance [63], improvisation dance [79], or mixed dance genres [27, 55, 62, 66, 67, 77, 78], with three studies including home-based dance programs [27, 68, 76]. The duration of interventions ranged from two weeks to two years with frequency per week varying from once a week to daily. The intervention session length was usually 1 hour, although it ranged from 30 minutes to two hours.
Method quality and risk of bias assessments were conducted for all studies. Table 3 shows that the risk of bias for five of the RCTs was high [54, 57, 59, 61, 66]. It was also high for two of the nonrandomised studies [72, 75]. In addition, 20 were at moderate risk of bias (eight RCTS, 12 nonrandomised studies) [26, 28, 30, 55, 56, 58, 65, 67, 69–71, 73, 74, 76–79, 84, 87, 88] and 11 were at low risk of bias (four RCTs, seven nonrandomised studies) [27, 62–64, 68, 81–83, 85, 86, 80]. For RCTs, blinding of the participants and therapists was generally not possible due to the nature of dance therapy. A large number of RCTs did not include intention to treat analysis [26, 30, 54–57, 59, 61, 65–67], concealed allocation [30, 54–61, 66], or reporting of outcomes for more than 85% of participants at each time point [26, 54, 57, 59–62, 65–67]. These omissions increased the risk of bias (Table 3). Non-RCT studies were identified as having increased risk of bias as there was no control group [28, 68, 70–74, 75–80, 84, 87], or they did not receive similar treatment or care [28, 68–75, 80, 81, 84, 87], or they did not conduct a follow-up [69–72, 74–76, 83–85, 87].
| Randomised controlled trials (PEDro Scale) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| First author, year | Random allocation | Concealed allocation | Baseline-similar | Blinded participant | Blinded therapist | Blinded assessor | Measures for >85% sample | ITT | Between group analysis | Outcome measure data | Score/10 |
| Duncan and Earhart, 2012 [62] | Y | Y | Y | N | N | Y | N | Y | Y | Y | 7 |
| Duncan and Earhart, 2014 [54] | Y | N | Y | N | N | Y | N | N | Y | Y | 5 |
| Hackney and Earhart, 2010 [88] | Y | N | Y | N | N | Y | N | Y | Y | Y | 6 |
| Hackney and Earhart, 2009 [61] | Y | N | Y | N | N | Y | N | N | Y | Y | 5 |
| Hackney et al., 2007 [59] | Y | N | Y | N | N | Y | N | N | Y | Y | 5 |
| Hashimoto et al., 2015 [67] | Y | Y | Y | N | N | Y | N | N | Y | Y | 6 |
| Kunkel et al., 2017 [55] | Y | N | Y | N | N | Y | Y | N | Y | Y | 6 |
| Lee et al., 2015 [57] | Y | N | Y | N | N | N | N | N | Y | Y | 4 |
| Lee et al., 2018 [63] | Y | Y | Y | N | N | Y | y | Y | Y | Y | 8 |
| McKee and Hackney, 2013 [66] | N | N | Y | N | N | Y | N | N | Y | Y | 4 |
| Michels et al., 2018 [30] | Y | N | Y | N | N | Y | Y | N | Y | Y | 6 |
| Poier et al., 2019 [64] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 7 |
| Rocha et al., 2018 [27] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Rios Romenets et al., 2015 [58] | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Shanahan et al., 2017 [26] | Y | Y | Y | N | N | Y | N | N | Y | Y | 6 |
| Solla et al., 2019 [56] | Y | N | Y | N | N | Y | Y | N | Y | Y | 6 |
| Volpe et al., 2013 [65] | Y | Y | Y | N | N | Y | N | N | Y | Y | 6 |
| Nonrandomised studies (JBI Appraisal Tool) | |||||||||||
| First author, year | Cause effect | Participants similar | Comparisons similar | Control group | Multiple measures | Follow-up | Consistent measurement | Reliable measurement | Statistical analysis | Score/9 | |
| Albani et al., 2019 [68] | Y | Y | N | N | Y | Y | Y | Y | Y | 7 | |
| Batson, 2010 [77] | Y | Y | Y | N | N | Y | Y | Y | N | 6 | |
| Blandy et al., 2015 [70] | N | Y | N | N | Y | N | Y | Y | Y | 5 | |
| Dahmen-Zimmer and Jansen, 2017 [69] | Y | N | N | Y | Y | N | Y | Y | Y | 6 | |
| Delextrat et al., 2016 [71] | Y | Y | N | N | Y | N | Y | Y | Y | 6 | |
| Hackney and Earhart, 2009 [72] | Y | N | N | N | Y | N | N | Y | Y | 4 | |
| Hackney and McKee, 2014 [28] | Y | N | N | N | Y | Y | N | Y | Y | 5 | |
| Heiberger et al., 2011 [78] | Y | N | Y | N | Y | Y | Y | Y | N | 6 | |
| Kalyani et al., 2019 [81] | Y | Y | N | Y | Y | Y | Y | Y | Y | 8 | |
| Listewnik and Ossowski, 2018 [75] | Y | N | N | N | N | N | Y | N | Y | 3 | |
| McGill et al., 2018 [85] | Y | Y | Y | Y | Y | N | Y | Y | Y | 8 | |
| McKay et al., 2016 [80] | Y | Y | N | N | Y | Y | Y | Y | Y | 7 | |
| McNeely et al., 2015 [74] | Y | Y | N | N | Y | N | Y | Y | Y | 6 | |
| McRae et al., 2018 [87] | Y | N | N | N | Y | N | Y | Y | Y | 5 | |
| Marchant et al., 2010 [79] | Y | N | Y | N | N | Y | Y | Y | Y | 6 | |
| Rawson et al., 2019 [86] | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 | |
| Seidler et al., 2017 [84] | Y | Y | N | N | Y | N | Y | Y | Y | 6 | |
| Shanahan et al., 2015 [76] | Y | N | Y | N | Y | N | Y | Y | Y | 6 | |
| Tillmann et al., 2020 [83] | Y | Y | Y | Y | N | N | Y | Y | Y | 7 | |
| Tunur et al., 2020 [73] | N | Y | N | N | Y | Y | Y | Y | Y | 6 | |
| Zafar et al., 2017 [82] | Y | N | Y | Y | Y | Y | Y | Y | Y | 8 | |
- Note: Y=yes; N=no.
Data analysis is presented in Tables 4 and 5. Overall, the results showed moderate to large benefits from therapeutic dance for people with mild to moderate PD (Table 4). RCTs demonstrated significant short-term benefits for balance with the Berg Balance scale (BBS) [30, 56, 57, 59–61, 67], significant reduction in disability measured by the Unified Parkinson’s Disease Rating Scale (UPDRS) [26, 30, 56, 59, 61, 62, 65, 67], significantly improved mobility measured by Timed Up and Go (TUG) [56, 58, 59, 61], significantly improved endurance measured by the 6 Minute Walk Test [56, 61], significantly reduced gait freezing measured by the Freezing of Gait scale [59, 61, 65], and significantly reduced depression measured by the Beck Depression Inventory [57]. Meta-analysis was not conducted due to intervention and outcome measure heterogeneity.
| Author (lead), year | Dependent variable | Outcome measure | Effect size | 95% Confidence interval (CI) | Dose of intervention |
|---|---|---|---|---|---|
| Duncan and Earhart (2012) [62]: tango vs. usual care | Disability-motor | UPDRS-motor 3 | −2.71 | −3.40 to −2.02 | 1 hr class, 2/week, 12 months |
| Hackney and Earhart (2010) [60]: partnered tango vs. nonpartnered dance | Balance | Berg balance scale | −0.33 | −0.96 to 0.30 | 1 hr, 2/week, 10 weeks |
| Mobility | Timed up and go | 0.52 | −0.12 to 1.16 | ||
| Hackney and Earhart (2009) [61]: waltz/foxtrot vs. control argentine tango vs. control | Disability | UPDRS | WF: −2.61 | −3.53 to −1.70 | 1 hr, 2/week, 13 weeks |
| T: −2.44 | −3.37 to −1.51 | ||||
| Balance | Berg balance scale | WF: 2.54 | 1.64 to 3.44 | ||
| T: 2.52 | 1.57 to 3.46 | ||||
| Mobility | Timed up and go | WF: -1.74 | −2.25 to −0.95 | ||
| T: −2.14 | −3.02 to −1.25 | ||||
| Endurance | 6 minute walk test | WF: 1.86 | 1.05 to 2.66 | ||
| T: 2.39 | 1.47 to 3.31 | ||||
| Freezing of gait | Freezing of gait | WF: 0.85 | 0.14 to 1.55 | ||
| T: 0.76 | 0.03 to 1.49 | ||||
| Tango vs. waltz/foxtrot | Disability | UPDRS | 0.55 | −0.17 to 1.27 | |
| Balance | BBS | −0.09 | −0.80 to 0.61 | ||
| Mobility | TUG | −0.75 | −1.48 to −0.02 | ||
| Endurance | 6MWT | 1.75 | 0.92 to 2.58 | ||
| Freezing of gait | FOG | −0.08 | −0.79 to 0.63 | ||
| Hackney et al. (2007) [59]: partnered argentine tango vs. group exercise class | Disability (motor) | UPDRS–Motor 3 | 1.53 | 0.51 to 2.55 | 1 hr, 2/week, 13 weeks |
| Balance | Berg balance scale | 3.52 | 2.09 to 4.96 | ||
| Mobility | Timed up and go | −4.78 | −6.54 to −3.01 | ||
| Freezing of gait | Freezing of gait | 1.56 | 0.54 to 2.59 | ||
| Gait velocity | Gait velocity m/s | −1.01 | −1.97 to −0.05 | ||
| Dual tasking | Velocity of dual walking task m/s | −1.11 | −2.08 to −0.05 | ||
| Hashimoto et al. (2015) [67]: PD dance vs. PD ex | Mobility | Time up and go | 0.29 | −0.40 to 0.99 | Dance: 60 min class (dance), 1/week, 12 weeks Exercise: 60 min class (stretching, strengthening), 1/week, 12 weeks |
| Balance | Berg balance scale | 1.49 | 0.71 to 2.28 | ||
| Disability | UPDRS | −0.89 | −1.62 to −0.16 | ||
| Depression | Self-rating depression scale | −0.18 | −0.88 to 0.51 | ||
| PD dance vs. control (usual care) | Mobility | Time up and go | −0.22 | −0.95 to 0.51 | Dance: 60 min class, 1/week, 12 weeks |
| Balance | Berg balance scale | 1.05 | 0.27 to 1.83 | ||
| Disability | UPDRS | −1.19 | −1.98 to −0.40 | ||
| Depression | Self-rating depression scale | −0.71 | −1.46 to 0.04 | ||
| Kunkel et al. (2017) [55]: dance vs. control | Balance | Berg balance scale | −0.01 | −0.62 to 0.59 | 1 hr, 2/week, 10 weeks |
| Mobility | Timed up and go | 0.37 | −0.24 to 0.97 | ||
| Endurance | 6 minute walk test | −0.26 | −0.87 to 0.34 | ||
| Quality of life | PDQ-39 | 0.13 | −0.47 to 0.73 | ||
| Lee et al. (2015) [57]: virtual reality vs. control | Balance | Berg balance scale | 1.09 | 0.15 to 2.03 | 30 mins, 5/week, 6 weeks |
| Activities of daily living | Modified Barthel index | 1.12 | 0.18 to 2.07 | ||
| Depression | Beck depression inventory | −1.30 | −2.26 to −0.34 | ||
| Lee et al. (2018) [63]: Qigong dancing vs. wait list | Disability | UPDRS | −0.36 | −1.00 to 0.27 | 60 min, 2/week, 8 weeks |
| Quality of life | PD quality of life | 0.55 | −0.09 to 1.19 | ||
| Balance | Berg balance sale | 0.38 | −0.25 to 1.01 | ||
| Depression | Beck depression inventory | 0.33 | −1.22 to 0.06 | ||
| McKee and Hackney (2013) [66]: tango vs. education | Disability (motor) | UPDRS–Motor 3 | −0.66 | −1.45 to 0.12 | 90 mins, 20 sessions, 12 weeks |
| Balance | Advanced balance scale | 0.32 | −0.45 to 1.09 | ||
| Mobility | Timed up and go | −0.07 | −0.83 to 0.70 | ||
| Quality of life | PDQ-39 | 0.16 | −0.61 to 0.93 | ||
| Freezing of gait | Freezing of gait | −0.27 | −1.00 to 0.53 | ||
| Michels et al. (2018) [30]: dance therapy vs. control | Disability (motor) | UPDRS–Motor 3 | −1.32 | -2.60 to −0.03 | 60 mins, 1/week, 10 weeks |
| Disability | UPDRS–Total | −0.61 | −1.81 to 0.59 | ||
| Balance | Berg balance scale | 1.32 | 0.03 to 2.60 | ||
| Mobility | Timed up and go | −1.07 | −2.32 to 0.18 | ||
| Depression | Beck depression inventory | 1.03 | −0.21 to 2.27 | ||
| Poier et al. (2019) [64]: argentine tango vs. tai chi | Quality of life | PDQ-39 | −0.14 | −0.87 to 0.59 | 60 min class, 1/week, 10 weeks |
| Satisfaction | BMLSS-life satisfaction | 0.18 | −0.55 to 0.91 | ||
| Rocha et al. (2018) [27]: argentine tango vs. mixed genre dance | Mobility | Timed up and go | −0.61 | −1.49 to 0.27 | In-person: 1 hour, 1/week Home: 40 mins, 1/week, 8 weeks |
| Freezing of gait | Freezing of gait | 0.26 | −0.60 to 1.12 | ||
| Balance | Berg balance scale | 0.43 | −0.44 to 1.30 | ||
| Quality of life | PDQ-39 | −0.75 | −1.64 to 0.14 | ||
| Disability (motor) | UPDRS 3 (R) | −0.01 | −0.87 to 0.85 | ||
| Disability (motor) | UPDRS 3 (L) | 0.14 | −0.72 to 0.99 | ||
| Rio Romenets et al. (2015) [58]: partnered tango vs. self-directed exercise | Disability | UPDRS-total | −0.50 | −1.19 to 0.20 | 1 hr, 2/week, 12 weeks |
| Disability (motor) | UPDRS 3 | −0.60 | −1.30 to 0.11 | ||
| Quality of life | PDQ-39 | 0.11 | −0.57 to 0.80 | ||
| Mobility | Timed up and go | −1.00 | −1.73 to −0.28 | ||
| Mobility | Dual timed up and go | 0.28 | −0.41 to 0.97 | ||
| Freezing of gait | Freezing of gait | −0.34 | −1.03 to 0.35 | ||
| Shanahan et al. (2017) [26]: Irish set dancing vs. usual care | Disability (motor) | UPDRS 3 | −1.13 | −1.79 to −0.47 | In-person: 1 hr, 1/week Home: 20 mins, 3/week, 10 weeks |
| Endurance | 6 minute walk test | 0.13 | −0.48 to 0.74 | ||
| Quality of life | PDQ-39 | 0.00 | −0.61 to 0.61 | ||
| Solla et al. (2019) [56]: Sardinian folk dance vs. usual care | Disability (motor) | UPDRS–Motor 3 | −1.16 | −2.11 to −0.21 | 90 mins, 2/week, 12 weeks |
| Endurance | 6 minute walk test | 2.57 | 1.38 to 3.75 | ||
| Balance | Berg balance scale | 1.99 | 0.92 to 3.07 | ||
| Mobility | Timed up and go | −1.81 | −2.85 to −0.77 | ||
| Volpe et al. (2013) [65]: Irish set dancing vs. physiotherapy | Disability (motor) | UPDRS-motor | −0.99 | −1.84 to −0.14 | Dance: 90 min classes, 1/week, 6 months PT: 90 mins, 1/week, 6 months, 1 hr weekly home video |
| Balance | Berg balance scale | 0.81 | −0.02 to 1.64 | ||
| Freezing of gait | Freezing of gait | −1.45 | −2.43 to −0.55 | ||
| Quality of life | PDQ-39 | −0.58 | −1.43 to 0.23 | ||
- PDQ-39: Parkinson’s Disease Questionnaire-39; PT: physiotherapy; UPDRS: Unified Parkinson′s Disease Rating Scale. Analyses were for baseline and after intervention data within groups, unless otherwise specified.
| Author (lead), year | Dependent variable | Outcome measure | Mean difference (within group: baseline to after intervention) | 95% confidence interval (CI) | Dose of intervention |
|---|---|---|---|---|---|
| Albani et al. (2019) [68] : home exercise + tango | Disability | UPDRS | −3.33 | N/A |
|
| Quality of life | PDQ-39 | −3.57 | N/A | ||
| Batson (2010) [77] : modern dance | Mobility | Timed up and go | 0.70 | N/A | 85 min class, 3/week, 3 weeks |
| Balance | Fullerton Advanced Balance Scale | 3.1 | N/A | ||
| Blandy et al. (2015) [70] : tango class | Quality of life | EurQol-5D | 0.06 (median) | N/A | 1 hr, 2/week, 4 weeks |
| Depression | Beck Depression Inventory | 4.50 (median) | N/A | ||
| Dahmen-Zimmer and Jansen (2017) [69] : dance training versus karate | Depression | Hospital Anxiety Depression Scale | ES (between group) 0.61 | −0.22 to 1.45 | 1 hr, 1/week, 30 weeks |
| Wellbeing | SF-12 | ES (between group) −1.02 | −1.88 to −0.15 | ||
| Delextrant et al. (2016) [71] | Aerobic capacity | Mean heart rate | No significant effect of dance style on heart rate (p = 0.689). | N/A | Up to 1 hr, weekly, 6 sessions |
| Hackney and Earhart (2009) [72]: Argentine tango | Balance | Berg Balance Scale | 2.80 | N/A | 1.5 hrs, 5/week, 2 weeks |
| Disability (motor) | UPDRS-motor 3 | −4.6 | N/A | ||
| Mobility | Timed up and go | −2.0 (seconds) | N/A | ||
| Endurance | 6-minute walk test | 35.90 (metres) | N/A | ||
| Hackney and McKee (2014) [28] : adapted tango | Balance | Berg Balance Scale | 0.30 | N/A | 1.5 hrs, 2/week, for 12 weeks |
| Mobility | Timed up and go | −0.19 | N/A | ||
| Heiberger et al. (2011) [78]: mixed dance for PD | Disability | UPDRS | 8.2 | N/A | 1/week class, 1.5 hrs, 8 months |
| Mobility | Timed up and go | 0.7 | N/A | ||
| Kalyani et al. (2019) [81]: dance class versus control | Quality of life | PDQ39 | ES (between group) 0.23 | −0.46 to 0.91 | 1 hr, 2/week, 12 weeks |
| Disability (ADL) | UPDRS-2 | ES (between group) −0.13 | −0.81 to 0.55 | ||
| Depression | Hospital Anxiety Depression Scale | ES (between group) −0.71 | −1.41 to 0.00 | ||
| Listewnik and Ossowski (2018) [75]: tango dance classes | Mobility | Tinetti Performance Oriented Mobility Assessment | 2.15 | N/A | 70 mins, 2/week, for 12 weeks |
| Mobility | Timed up and go | −1.72 | N/A | ||
| Endurance | 6-minute walk test | 85.20 | N/A | ||
| McGill et al. (2018) [85]: ballet classes versus no dance | Gait | Step variability | ES (between group) 0.70 | −0.03 to 1.42 | 1.25–1.5 hrs, 1/week, for 1 year |
| Gait | Stride variability | ES (between group) 0.62 | −0.10 to 1.34 | ||
| Balance | Activities-Specific BalanceConfidence Scale | ES (between group) 0.24 | −0.47 to 0.95 | ||
| McKay et al. (2016) [80]: adapted tango | Disability (motor) | UPDRS-motor 3 | −2.90 | N/A | 90 mins, 15 lessons over 3 weeks |
| Balance | Berg Balance Scale | 3.80 | N/A | ||
| Endurance | 6-minute walk test | 40.80 | N/A | ||
| Mobility | Timed up and go | −1.10 | N/A | ||
| Freezing of gait | Freezing of gait | 0.10 | N/A | ||
| McNeely et al. (2015) [89]:tango vs. mixed dance | Disability (motor) | UPDRS-motor 3 | ES (between group) −0.42 | −1.41 to 0.57 | 1 hr group class, 2/week, 12 weeks |
| Quality of life | PDQ-39 | ES (between group) −0.25 | −1.23 to 0.74 | ||
| Mobility | Timed up and go | ES (between group) 0.2 | −0.78 to 1.19 | ||
| Mobility | Dual task timed up and go | ES (between group) 0.42 | −0.57 to 1.41 | ||
| Endurance | 6-minute walk test | ES (between group) −0.39 | −1.38 to 0.60 | ||
| McRae et al. (2018) [87]: dance classes | Quality of life | Short-Form Health Survey | 3.84 | N/A | 1-2/week, 12 months (6 months–2yrs), session length unknown |
| Marchant et al. (2010) [79]: improvisation dance | Disability (motor) | UPDRS-motor 3 | 5.4 | N/A | 10 1.5 hour classes, 2 weeks |
| Endurance | 6-minute walk test | −3.8 | N/A | ||
| Mobility | Timed up and go | −0.5 | N/A | ||
| Balance | Berg Balance Scale | 3.0 | N/A | ||
| Rawson et al. (2019) [86] tango vs. treadmill | Disability (motor) | UPDRS-motor 3 | ES (between group) 1.35 | 0.83 to 1.87 | 1 hr class, 2/week, 12 weeks |
| Endurance | 6-minute walk test | ES (between group) 0.29 | −0.19 to 0.76 | ||
| Quality of life | PDQ-39 | ES (between group) 0.44 | −0.04 to 0.92 | ||
| Tango vs control (stretching) | Disability (motor) | UPDRS-motor 3 | ES (between group) 1.07 | 0.56 to 1.57 | |
| Endurance | 6-minute walk test | ES (between group) −0.80 | −1.29 to −0.31 | ||
| Quality of life | PDQ-39 | ES (between group) 1.14 | 0.63 to 1.65 | ||
| Seidler et al. (2017) [84]: tele-rehabilitation group (tango versus in-person group) | Disability (motor) | UPDRS-motor 3 | ES (between group) 0.22 | −0.66 to 1.10 | 1 hr, 2/week, 12 weeks |
| Shanahan et al. (2017) [76] : Irish set dancing | Disability (motor) | UPDRS-motor 3 | −2.0 (median) | N/A | In person: 1.5 hrs, 1/week Home: 20 mins, 2/week, 8 weeks |
| Quality of life | PDQ-39 | −4.03 (median) | N/A | ||
| Endurance | 6-minute walk test | 0.0 | N/A | ||
| Balance | Berg Balance Scale | 1.0 | N/A | ||
| Tillmann et al. (2020) [83] : Brazilian samba versus control | Beck Depression Inventory | ES (between group) 1.17 | 0.55 to 1.79 | 1 hr, 2/week, 12 weeks | |
| Tunur et al. (2020) [73] : Google glass dancing | Mobility | Timed up and go | 0.5 | N/A |
|
| Mobility | Dual task timed up and go | −0.5 | N/A | ||
| Zafar et al. (2017) [82] : adapted tango for PD versus AT for older adult | Participation | Participation and Autonomy Scale | ES (between group) 0.32 | −0.20 to 0.83 | 90 min, 2/week, 12 weeks |
- Note: ES, effect size; PDQ-39, Parkinson’s Disease Questionnaire-39; UPDRS: Unified Parkinson’s Disease Rating Scale Analyses were for baseline and postintervention data within groups, unless otherwise specified.
The effects of dancing for PD reported in non-RCTs demonstrated end of intervention benefits for people with mild to moderately severe disease (Table 5). There were improvements in balance (BBS) [28, 72, 77, 80], disability (UPDRS) [68, 72, 78, 80, 86], mobility (TUG) [28, 72, 73, 75, 80] and Tinetti Mobility Scale [75], depression [70, 83], and quality of life [26, 68–70, 86, 87]. Key studies on digital delivery modes for dancing with PD (e.g., [57, 73, 84]) showed that virtual technologies can be an accessible and beneficial method of physical activity for some people living with this chronic and progressive disease.
4. Discussion
This systematic review of the global literature showed that dancing for individuals with mild to moderately severe PD could be a beneficial and accessible form of physical activity for some people, whether delivered face-to-face or using an online telemedicine platform or “virtual dance” video-gaming tools. The findings support mounting evidence that therapeutic dance can, in the short term, significantly improve balance, mobility, gait, disability, and quality of life in PD [26, 68, 70, 86, 87, 89]. Although the recruitment levels in the reviewed studies did not always meet clinical trial targets, attendance and adherence to dance classes were generally high. The duration of the dancing classes and session lengths varied, and improvements were seen in interventions running for two weeks [72] up to 2 years [54]. There were significant improvements when session lengths ranged from 30 to 90 minutes per day. Although previous systematic reviews of dance for Parkinson’s disease were conducted by Shanahan et al. (2017) [36], Carapellotti et al. [31], Berti et al. [37], and Rocha et al. [90], all of those were confined to randomised controlled clinical trials. By conducting a more recent search and extending our analysis to RCTs and non-RCT quantitative studies, our review captured more of the therapies currently being implemented in clinical practice.
Our review suggests good attendance for the telehealth mode of delivery in chronic diseases, possibly because digital delivery reduces geographical, environmental, economic, and commute barriers [91]. Some technological difficulties can be encountered with digital delivery [84] such as Internet and usability problems and the need for training and guidance in how to operate the technology. Nevertheless, the reviewed articles did not directly analyse the risk of falls with online delivery or when using video modes. For people with moderate to advanced disease, postural instability and falls can be problematic. Precautions need to be taken to ensure that people at home have strategies to prevent and manage falls, should they occur.
There are several clinical implications of this systematic review. Dancing was shown to be clinically feasible, with high levels of adherence by participants and considerable interest in future classes. Many of the publications that we reviewed supported the need to increase access to community dance classes to improve exercise capacity and wellbeing, as well as to increase the opportunity for people living with Parkinsonism to socialise. For face-to-face dance classes, there is a need to determine how to reduce barriers to participation, including transportation, access, and cost, (please see [1, 92]). For digital modes of dancing, clinical protocols are needed to support safe and sustainable implementation and guidance in the use of technology. In addition, it could be argued that a need exists for credentialing programs for dance teachers and practitioners, to ensure evidence-based and effective delivery of this form of structured exercise [93] as well as protocols for clinicians and dance teachers to ensure safe and effective delivery. In the current global context of the COVID-19 pandemic, there is arguably a need to further explore digitally delivered dance and other forms of physical activity for people living with chronic neurological conditions [91, 94].
Despite the systematic review being informed by the Cochrane guidelines, there were several limitations. Most studies included people with mild-moderate disease. The findings might not generalise to people with end-stage disease or very old people, or those who cannot access face-to face classes or digital technologies. Many trials did not control for the effects of levodopa or other Parkinson’s medications. Intervention duration and frequency were reported; however, none of the studies documented the intensity of dance therapy. Although some large, significant effects were demonstrated, these need to be considered in light of the moderate to high risk of bias in many studies, especially those that were not randomised trials. Although dance and music were shown to have benefit for people living with PD, the most effective dance genre or music type require further exploration [95]. Quality of life can be adversely affected by Parkinsonism [3, 5], and the mechanisms by which arts-health therapies such as dance and music can improve health-related quality of life warrant further exploration [95]. Also, the reviewed articles were in the English-language, limiting generalisability to non-English speaking cultures and their associated dance genres.
To conclude, dance is safe and feasible for some people in the early to midstages of PD, provided that safety precautions and training are incorporated into design and delivery. There are positive associations between therapeutic dancing and improvements in gait, balance, movement disorders, and disability. For some individuals, there can be improvements in quality of life. There was preliminary evidence that delivery of dancing for PD online is beneficial for some people, although there is a need to verify the efficacy and safety of this modality, especially for people who are frequent fallers.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Acknowledgments
This review was funded and copartnered by La Trobe University and Parkinson’s Victoria. The authors thank the La Trobe University librarians who ably assisted with the database searches and Parkinson’s Victoria for supporting this project.
Open Research
Data Availability
Data are available on request to the corresponding author.




