[Retracted] Efficacy of Otomicroscopy Combined with Otoendoscopy Double-Lens Technology-Assisted Tympanic Membrane Repair on Elderly Patients with Chronic Suppurative Otitis Media
Abstract
Objective. To investigate the effect of otomicroscopy combined with otoendoscopy double-lens technology-assisted tympanic membrane repair on elderly patients chronic suppurative otitis media (CSOM). Methods. 120 elderly CSOM patients from January 2017 to July 2019 were selected and divided into the otomicroscopy group (n = 40), the otoendoscopy group (n = 40), and the double-lens group (n = 40) by the random number method. All patients were treated with tympanic membrane repair. The otomicroscopy group was assisted by otomicroscopy, the otoendoscopy group was assisted by otoendoscopy. and the double-lens group was assisted by otomicroscopy combined with otoendoscopy. The three groups of operations status, clinical efficacy, the incidence of adverse reactions, hearing improvement rate, and satisfaction rate with incision after 6 months were compared. Results. The operation time, intraoperative blood loss, hospitalization time, and VAS score of the otoendoscopy group and the double-lens group were all lower than those of the otoendoscopy group, and the operation time of the double-lens group was lower than that of the otoendoscopy group (P < 0.05). The clinical efficacy of the double-lens group was better than that of the otomicroscopy group and otoendoscopy group (P < 0.05). The adverse reaction rate of the otoendoscopy group and the double-lens group was lower than that of the otomicroscopy group, and the average postoperative air-bone conductance of the double-lens group was lower than that of the otomicroscopy group and the otoendoscopy group, and the hearing improvement rate was higher than that of the otomicroscopy and otoendoscopy groups (P < 0.05). The satisfaction rate with postoperative incision in the otoendoscopy group and double-lens group was higher than that in the otomicroscopy group (P < 0.05). Conclusion. The double-lens technology-assisted tympanic membrane repair has an obvious effect on elderly patients with CSOM. Compared with the single-use otomicroscopy, the operation time, intraoperative blood loss, hospitalization time, patient’s dry ear condition, degree of surgical pain, clinical efficacy, adverse reaction rate, hearing improvement rate, and patient’s incision satisfaction of the double-lens technology are better. Compared with the single-use otoendoscopy, the operation time, clinical efficacy, and hearing improvement rate of the double-lens technology are better.
1. Introduction
Chronic suppurative otitis media (CSOM) is a chronic suppurative inflammatory reaction of the middle ear mucosa and tympanic membrane, which often invades middle ear tissues such as tympanum, mastoid process, tympanic sinus, and eustachian tube. The main clinical manifestations of this disease are tympanic membrane perforation, hearing loss, and intermittent or continuous discharge of pus in the ear [1]. CSOM is one of the most common inflammatory lesions in otolaryngology. If it is not treated in time, severe cases can cause intracranial and extracranial complications [2]. The pathogenesis of CSOM is still unclear. At present, it is mostly believed that it is caused by acute otitis media with treatment failure or incomplete treatment and is related to age, environment, genetics, and eustachian tube function [3, 4]. The elderly have a high incidence of CSOM due to aging of their organs and decreased autoimmunity. The primary goal of clinical treatment of CSOM is to reduce the symptoms of patients and restore hearing to the greatest extent. Surgical treatment is one of its main methods. For CSOM patients with complete ossicular chain and only tympanic membrane perforation with normal mastoid, tympanic membrane repair is the most commonly used surgical treatment to improve their clinical symptoms, reconstruct the sound transmission structure, and improve hearing [5–7]. The traditional method of tympanic membrane repair is assisted by otomicroscopy. This method has been widely used clinically, and the technology is mature. However, it requires a wider surgical path, and the surgical wound is large, which easily triggers the patient’s resistance [8]. With the development of endoscopic technology and related devices, otoendoscopy-assisted tympanic membrane repair has gradually been applied in clinical practice. The otoendoscopy can directly observe the tympanic membrane, so that the surgeon can operate close to the lesion, and the image presented is clear and magnified, which is in line with the concept of minimally invasive. However, the easy contamination of the mirror surface, the small operation space, and the difficulty of the operation are also the unavoidable shortcomings of this technology at this stage [9]. Endoscopy combined with microscopy has been used in various groups of brain-related minimally invasive surgery, but its application in middle ear surgery is still relatively small [10]. This study uses otomicroscopy combined with otoendoscopy to treat elderly CSOM and summarizes our hospital’s clinical experience in operating double-lens technology-assisted tympanic membrane repair, in order to provide a certain reference for the surgical treatment of CSOM.
2. Materials and Methods
2.1. Research Object
Total of 120 elderly CSOM patients admitted to our hospital from January 2017 to July 2019 were selected. Inclusion criteria: meet the CSOM diagnostic criteria [11], age 60–85 years; complete ossicular chain, good eustachian tube function, CT of the temporal bones showed no lesions in the mastoid and tympanum, dry ear time> 1 month, and good compliance. Exclusion criteria: combined with auricle deformity, ear canal erosion, and other factors that affect hearing recovery, combined with acute upper respiratory tract infection or other active infections, combined with middle ear cholesteatoma, and combined cognitive impairment. According to the random number method, 120 patients were divided into the otomicroscopy group, otoendoscopy group, and double-lens group, each with 40 cases. There was no statistically significant difference in the basic data of the three groups of patients (P > 0.05), as given in Table 1.
| Group | n | Male/female | Age (year) | Disease course (year) | Preoperative air-bone conduction difference (dBHL) | Cases of perforation diameter >5 mm (n) |
|---|---|---|---|---|---|---|
| Otomicroscopy group | 40 | 22/18 | 65.14 ± 2.39 | 5.32 ± 1.89 | 22.11 ± 5.89 | 12 |
| Otoendoscopy group | 40 | 19/21 | 66.03 ± 2.71 | 5.14 ± 2.13 | 21.69 ± 6.44 | 9 |
| Double-lens group | 40 | 25/15 | 65.55 ± 2.39 | 5.71 ± 2.24 | 22.71 ± 5.13 | 11 |
- There was no statistically significant difference in the basic data of the three groups of patients (P > 0.05).
2.2. Research Methods
The otomicroscopy group was treated with otomicroscopy-assisted tympanic membrane repair. After the patient is under general anesthesia, the surgeon routinely makes a “C”-shaped incision behind the ear, separates and exposes the temporalis muscle fascia, cuts it out of an appropriate size, and air-dried it for later use. Separate the external auditory canal skin from the temporal line to the anterior edge of the sigmoid sinus projection area, expose the anterior superior spine of the external auditory canal, thin the auditory canal skin, insert a retractor, and remove excess squamous bone. Expose the tympanic ring and ossicles under the otomicroscopy, create a fresh transplant bed, and implant the temporalis muscle fascia with the built-in method. Lift the fascia and fill the tympanic cavity and outside of the tympanic membrane with a proper amount of gelatin sponge. After reduction, gelatin sponge and chlortetracycline ointment gauze fill the entire operation cavity, suture the incision layer by layer, and then bandage it. Give conventional treatments such as antibiotics after the operation and clean up the residual gelatin sponge 2 weeks later.
The otoendoscopy group was treated with otoendoscopy-assisted tympanic membrane repair. After the patient is anesthetized, the appropriate cartilage-perichondrium is cut from the affected tragus, thinned and trimmed to a suitable size, and flattened for later use. Observe the tympanic membrane with an otoendoscopy and peel off the edge of the tympanic membrane to create a fresh wound. Approximately 8 mm away from the tympanic ring, make an arc-shaped incision on the front and rear lower walls of the external ear canal, peel off and turn the ear canal skin-tympanic flap forward, enter the tympanum, and expose the tympanic ring. Lift up the tympanic membrane, get the cartilage-periperitoneum to repair the tympanic membrane, and the rest of the operation is the same as that of the otomicroscopy group.
The double-lens group was treated with otomicroscopy combined with otoendoscopy-assisted tympanic membrane repair. After the patient is anesthetized, the appropriate cartilage-perichondrium is cut from the affected tragus, thinned and trimmed to a suitable size, and flattened for later use. Under otoendoscopy, remove calcification foci with microscopic instruments, scrape out the surrounding epithelium of the perforation, and make a fresh blood oozing wound to form a transplant bed. Under the microscope, peel off and turn over the tympanic membrane of the external auditory canal, enter the tympanic cavity, and implant the cartilage-periosteal membrane between the malleus stem or ossicles and the tympanic membrane. Flatten the fascia under the ear endoscope, and the rest is the same as the ear microscope group.
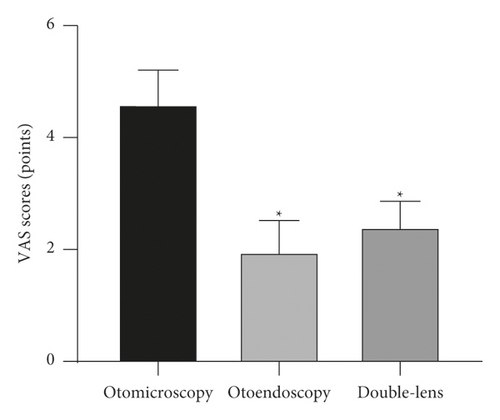
Comparing the operation status, including the patient’s operation time, intraoperative blood loss, hospitalization time, visual analogue scale (VAS) score, the higher the VAS score, the more severe the patient’s pain.
Comparing clinical efficacy, efficacy standards, markedly effective, otitis media, and related clinical symptoms disappeared, and hearing returned to normal; effective, otitis media, and related clinical symptoms are significantly improved, and hearing is significantly improved; ineffective, the above standards are not met. Total effective rate = (markedly effective + effective) number of cases/total number of cases × 100%.
Comparing the incidence of adverse reactions (reperforation, infection, tympanic membrane displacement, and dizziness) and hearing improvement rate, the average postoperative air-bone conduction difference ≤20dBHL is regarded as hearing improvement.
Comparing the satisfaction rate of three groups of patients with surgical incision at 6 months after operation, divided into satisfaction, basic satisfaction, and dissatisfaction, the total satisfaction rate = (basically satisfied + satisfied) number of cases/total number of cases × 100%.
2.3. Statistical Methods
The SPSS19.0 software was used for processing, measurement data were expressed as mean ± standard deviation (), multiple group comparisons were analyzed by the variance analysis, and pairwise comparisons were analyzed by the t-test. The enumeration data were expressed by (%), and the comparison between groups was analyzed by the χ2 test. The test level is α = 0.05, and P < 0.05 indicates that the difference is statistically significant.
3. Results
3.1. Comparison of the Operation Status of the Three Groups
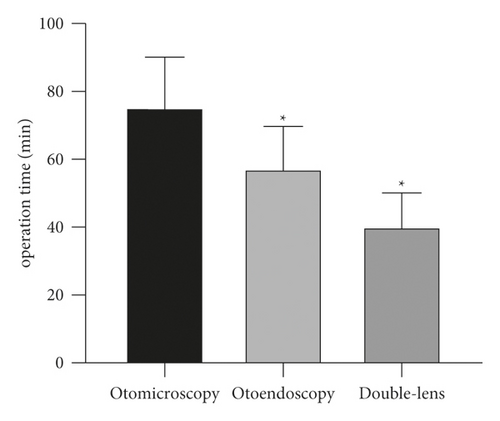
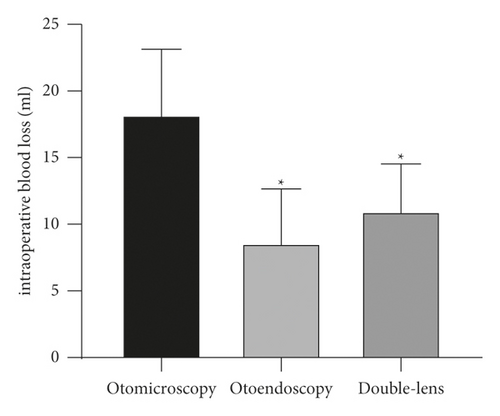
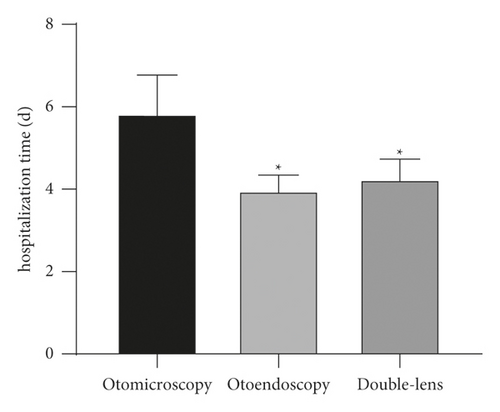
The operation time, intraoperative blood loss, hospitalization time, and VAS scores of the otoendoscopy group and the double-lens group were lower than those of the otomicroscopy group, and the operation time of the double-lens group was lower than that of the otoendoscopy group. The differences were statistically significant (P < 0.05), as given in Figures 1–4.
3.2. Comparison of Clinical Efficacy of the Three Groups
The total effective rate of the double-lens group was higher than that of the otomicroscopy group and the otoendoscopy group. The differences were statistically significant (P < 0.05), as given in Table 2.
| Group | n | Markedly effective | Effective | Ineffective | Total effective rate |
|---|---|---|---|---|---|
| Otomicroscopy group | 40 | 18 | 14 | 8 | 32 (80.00) |
| Otoendoscopy group | 40 | 23 | 10 | 7 | 33 (82.50) |
| Double-lens group | 40 | 26 | 11 | 3 | 37 (92.50) ∗# |
- Note. Compared with the otomicroscopy group, ∗P < 0.05. Compared with the otoendoscopy group, #P < 0.05.
3.3. Comparison of Incidence of Adverse Reactions and Hearing Improvement Rate of the Three Groups
The adverse reaction rate of the otoendoscopy group and the double-lens group was lower than that of the otomicroscopy group. The average postoperative air-bone conduction difference of the double-lens group was lower than that of the otomicroscopy group and the otoendoscopy group, and the hearing improvement rate of the double-lens group was higher than that of the otomicroscopy group and the otoendoscopy group. The differences were statistically significant (P < 0.05), as given in Table 3.
| Group | n | Adverse reactions | Incidence of adverse reactions | Average air-bone conduction difference | Hearing improvement rate | ||||
|---|---|---|---|---|---|---|---|---|---|
| Reperforation | Infection | Tympanic membrane displacement | Dizziness | Preoperation | Postoperation | ||||
| Otomicroscopy group | 40 | 6 | 3 | 1 | 2 | 12 (30.00) | 22.11 ± 5.89 | 14.72 ± 4.97 | 31 (77.50) |
| Otoendoscopy group | 40 | 2 | 1 | 1 | 1 | 5 (12.50) ∗ | 21.69 ± 6.44 | 15.42 ± 4.16 | 32 (80.00) |
| Double-lens group | 40 | 1 | 0 | 1 | 1 | 3 (7.50) ∗ | 22.71 ± 5.13 | 12.31 ± 4.21 ∗# | 39 (97.50) ∗# |
- Note. Compared with the otomicroscopy group, ∗P < 0.05. Compared with the otoendoscopy group, #P < 0.05.
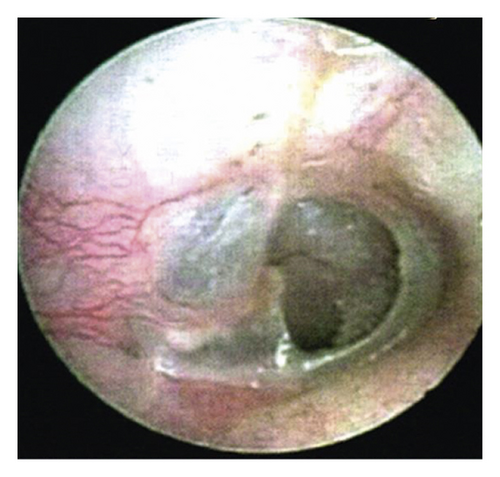
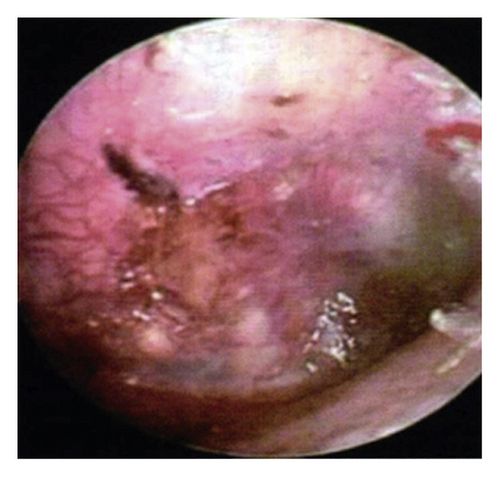
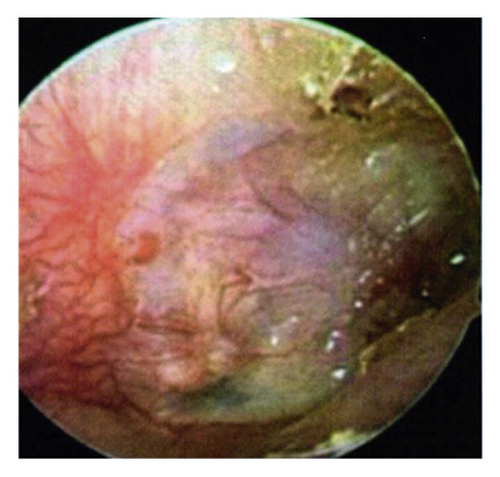
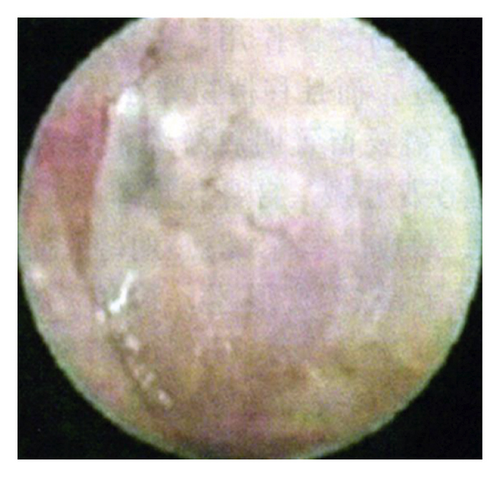
Typical cases of the double-lens group: Mr. Wu, 63 years old, with chief complain “Repeated discharge of the left ear with hearing loss for 3 years,” preoperative air-bone conduction difference 21 dBHL, perforation diameter < 5 mm, and the postoperative air-bone conduction difference 9 dBHL. There was no adverse reaction after the operation. One month after the operation, the transplant has a good growth status and rich blood supply; 3 months after the operation, the surface of the tympanic membrane is repaired and there is no obvious transplantation boundary; 6 months after the operation, there is no tympanic membrane atrophy, external migration, and adhesion. The operation was successful, as given in Figures 5–8.
3.4. Comparison of Postoperative Incision Satisfaction Rate of the Three Groups
The satisfaction rate in the otoendoscopy and double-lens group is higher than that in the otomicroscopy group. The differences were statistically significant (P < 0.05), as given in Table 4.
| Group | n | Satisfaction | Basic satisfaction | Dissatisfaction | Total satisfaction rate |
|---|---|---|---|---|---|
| Otomicroscopy group | 40 | 8 | 14 | 18 | 22 (55.00) |
| Otoendoscopy group | 40 | 17 | 16 | 7 | 33 (82.50) ∗ |
| Double-lens group | 40 | 11 | 19 | 10 | 30 (75.00) ∗ |
- Note. Compared with the otomicroscopy group, ∗P < 0.05.
4. Discussion
CSOM is a common disease of clinical otology in the elderly. Due to the special anatomical structure of the middle ear and mastoid, when the tympanic membrane perforates, it can easily spread to the surrounding tissues and organs and cause intracranial and extracranial complications, such as meningitis and labyrinth. Inflammation in severe cases can be life-threatening, and this is also the most common cause of clinical conductive deafness [12]. Tympanic membrane repair is a surgical method to repair the tympanic membrane by transplanting other tissues. It can not only completely remove the middle ear lesions, avoid exogenous bacterial infections, and reduce the incidence of repeated middle ear infections and complications but also reconstruct the sound transmission structure of the middle ear to improve the hearing of the patient [13]. Therefore, effective tympanic membrane repair for elderly CSOM patients with indications is a good means to ensure the quality of life and health of patients. There are two main assisted instruments for tympanic membrane repair: otomicroscopy and otoendoscopy. Otoendoscopy-assisted tympanic membrane repair is superior to otomicroscopy-assisted in terms of intraoperative blood loss and operation time [14]. However, the otoendoscopy has the disadvantages of requiring one-handed operation, difficult operation, small space, easy to contaminate the lens, and low imaging quality. Compared with otomicroscopy, there is no significant difference in the postoperative efficacy of otoendoscopy [15]. Which method can be used to better improve surgical efficacy and patient satisfaction has always been the research focus of clinical otology. Our hospital has rich clinical experience in the surgical treatment of CSOM. Through continuous discussion and summary after the operation, it is often found that the combination of the two can often achieve better results, and at the same time, reduce the operating requirements for the surgeon. After a certain period of training, the double-lens technology can be more proficiently mastered.
The results showed that the operation time, intraoperative blood loss, hospitalization time, and VAS scores of the otoendoscopy group and the double-lens group were lower than those of the otomicroscopy group; the operation time of the double-lens group was lower than that of the otoendoscopy group. The reason may be that the double-lens group can not only operate under video images but also can directly look at the angle of view. During the operation, there is no need to rotate the patient’s position to obtain a satisfactory angle of view and to minimize the impact of lens contamination. Compared with the otoscope group, the operation is simple, and the otoscope group has a flexible viewing angle, so the operation time is shorter [16, 17]. Compared with the otoendoscopy group, the operation is simpler, and compared with the otomicroscopy group, surgical perspective is more flexible, so the operation time of the double-lens group is shorter [18]. In addition, both the double-lens group and the otoendoscopy group can directly expose the tympanic membrane through the external auditory canal, eliminating the need to make a large incision in the auricle and temporal area, which makes the surgical wound smaller, so the operation time, intraoperative bleeding, hospitalization time, and pain are all lower than those in the otomicroscopy group.
In this study, the clinical efficacy, postoperative average air-bone conduction difference, and hearing improvement rate in the double-lens group were better than those in the otomicroscopy group and the otoendoscopy group; the adverse reaction rates in the otoendoscopy group and double-lens group were lower than those in the otomicroscopy group. In addition, the satisfaction rate with postoperative incisions in the double-lens group and the otoendoscopy group was higher than that of the otomicroscopy group. The reason may be that due to the limited exposure of the posterior wall of the mastoid through the ear incision and the blind area of the visual field under “direct vision” under the otomicroscopy, the contouring of the mastoid and the lateral wall of the tympanic sinus and the treatment of diseased tissue under otoendoscopy will have obvious advantages. Besides, the otoendoscopy can cross the narrow ear canal and observe deep cavities from multiple angles and in-depth and can clearly enlarge the observation field and comprehensively observe the lesion field, avoiding surgical errors, reducing unnecessary damage, and then improving the efficacy of surgery and minimizing the occurrence of adverse reactions [19]. However, the otoendoscopy is a 2D imaging, has a small angle of view, and must be operated with one hand; besides, its lens is susceptible to contamination by blood and tissue fragments and loses the field of vision; therefore, it is more difficult to use otoendoscopy surgery alone [20]. In contrast, the double-lens group is operated under a microscopy when the external auditory canal tympanic flap is lifted and cartilage is inserted, which avoids the shortcomings of otoscope as much as possible, thereby ensuring the smooth operation of the operation and obtaining better surgical results.
5. Conclusion
Otomicroscopy and otoendoscopy double-lens technology-assisted tympanic membrane repair has an obvious effect on elderly patients with CSOM. Compared with the single-use otomicroscopy, the operation time, intraoperative blood loss, hospitalization time, patient’s dry ear condition, degree of surgical pain, clinical efficacy, adverse reaction rate, hearing improvement rate, and patient’s incision satisfaction of the double-lens technology are better. Compared with the single-use otoendoscopy, the operation time, clinical efficacy, and hearing improvement rate of the double-lens technology are better.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors’ Contributions
Xin Cheng and Shaohua Wu are the co-first authors.
Open Research
Data Availability
The data used and/or analyzed during the current study are available from the corresponding author upon request.




