Healthcare Professional’s Perception of Patient Safety Measured by the Hospital Survey on Patient Safety Culture: A Systematic Review and Meta-Analysis
Abstract
Objective. To assess the culture of patient safety in studies that employed the hospital survey on patient safety culture (HSOPS) in hospitals around the world. Method. We searched MEDLINE, EMBASE, SCOPUS, CINAHL, and SciELO. Two researchers selected studies and extracted the following data: year of publication, country, percentage of physicians and nurses, sample size, and results for the 12 HSOPS dimensions. For each dimension, a random effects meta-analysis with double-arcsine transformation was performed, as well as meta-regressions to investigate heterogeneity, and tests for publication bias. Results. 59 studies with 755,415 practitioners surveyed were included in the review. 29 studies were conducted in the Asian continent and 11 in the United States. On average studies scored 9 out of 10 methodological quality score. Of the 12 HSOPS dimensions, six scored under 50% of positivity, with “nonpunitive response to errors” the lowest one. In the meta-regression, three dimensions were shown to be influenced by the proportion of physicians and five by the continent where survey was held. Conclusions. The HSOPS is widely used in several countries to assess the culture of patient safety in hospital settings. The culture of culpability is the main weakness across studies. Encouraging event reporting and learning from errors should be priorities in hospitals worldwide.
1. Introduction
Health institutions, which are known to be complex organizations, have over the years devised improvement strategies and added quality to the health care service [1]. Patient′s safety culture reflects the perceptions of processes, norms, and attitudes relating to a culture of preventable errors shared by health professionals in the delivery of care [2]. In health environments, behaviors and attitudes shape the culture of each organization [3]. The sharing of beliefs, values, and attitudes related to the patient′s safety culture influences the outcome and organizational aspects [4].
Higher culture of patient safety has been shown to be associated with better patient outcomes [5]. Quality in hospital services means providing the patient with multidisciplinary care at minimal risk [6]. Therefore, implementing improvements in organizational and safety culture enhances quality [7].
Surveys are widely used to assess the culture of safety by identifying the perception of health practitioners [8]. Such inquiries allow for a general assessment of the work climate, the relationship between teams or in a given group, communications, professional relationships, and hierarchical relations. They can identify areas that need prioritization for interventions.
Among the validated tools [8], the Hospital Survey on Patient Safety Culture (HSOPS) and the Safety Attitudes Questionnaire (SAQ), both created in the United States of America (US), are widely cited in research that aims to assess the safety culture of patients in different countries [9]. The HSOPS was designed by the US Agency of Healthcare Research and Quality in 2004 and proposes the assessment of 12 dimensions pertaining to the climate of patient safety in hospital setting. Seven dimensions of the survey are related to the work area, three dimensions explore aspects of the safety culture in the hospital, and two are outcome variables [10]. The culture of safety is measured by the staff perspective. For each dimension, percentages above 75% are considered as strengths and below 50% are areas that need improvement [10].
Since its inception, HSOPS has been translated and validated in several languages and settings [11–17]. To date, no compilation of surveys that employed HSOPS in hospitals in different countries. This comparison would bring valuable sources of strengths and limitations of culture of patient safety.
The aim of present study is to summarize surveys that assessed the culture of patient safety by HSOPS in hospitals worldwide, by means of a systematic review and meta-analysis.
2. Methods
2.1. Protocol and Registration
The protocol for this review was prepared in advance and registered in the International Prospective Register of Systematic Reviews (PROSPERO) under registration number CRD42016047941.
2.2. Eligibility Criteria
Studies meeting the criteria were selected as follows: Portuguese, Spanish, or English language; publication date between 2008 and 2015; cross-sectional, hospital-based design; full or partial use of the HSOPS questionnaire; inclusion of staff with direct or indirect patient contact; and surveying one or more categories of health professionals.
Studies were excluded if they were performed outside of the hospital setting, if they were conducted in a single area or unit of the hospital, or if they were lacking in results for each dimension. Additionally, validation studies, duplicate studies, papers with no full-text available, or studies that used qualitative approaches were excluded.
2.3. Information Sources and Search Strategy
The following databases were searched: MEDLINE (via PubMed), EMBASE, SCOPUS, CINAHL, and SciELO.
The search terms used for PubMed that were adapted for the other databases were “HSOPSC OR (Hospital Survey on Patient Safety Culture)”.
2.4. Study Selection
The Covidence software platform (www.covidence.org) was used to organize the references and find duplicates. Two independent reviewers screened the titles and abstracts of the papers, with selected papers progressing to the second phase, which was a full-text review. The articles were evaluated according to pre-specified criteria and, in the event of disagreements in either of the two phases, a third reviewer determined the inclusion.
2.5. Data Collection Process
Two reviewers independently summarized the data using a data extraction sheet. The following information was collected from each paper: year, country, proportion of physicians and nurses, sample size, and results for the 12 HSOPS dimensions (Table 1).
| Dimensions of patient safety culture related to the work area or unit | |
| (1) Teamwork within units | Supervisors and managers consider employee suggestion about patient safety, teamwork and open communication about errors, work hours are adequate to provide the best patient care. Feedback from management, and continuous improvement to avoid errors. |
| (2) Supervisor/manager expectations and actions that promote patient safety | |
| (3) Organizational learning and continuous improvement | |
| (4) Communication openness | |
| (5) Feedback and communication about error | |
| (6) Staffing | |
| (7) Nonpunitive response to errors | |
| Dimensions explore aspects of the safety culture in hospital | |
| (8) Management support for patient safety | Hospital management support patient safety and patient care information are not lost during shift change and from one unit to another |
| (9) Teamwork across units | |
| (10) Handoffs and Transition | |
| Dimensions of outcome variables | |
| (11) Overall perceptions of patient safety | Existence of procedures to avoid the occurrence of errors, notifications of possible problems and corrections before they affect the patient |
| (12) Frequency of events reported | |
2.6. Risk of Bias
Two reviewers evaluated the studies independently using a validated 10-item tool, which assessed (i) representativeness of the sample, (ii) appropriateness of the recruitment, (iii) adequacy of the sample size, (iv) description of both the study subjects and the setting, (v) response rate, (vi) objective, standard criteria used for the measurement of the condition, (vii) reliability of the measurement of the condition, (viii) appropriateness of the statistical analysis, (ix) important confounding factors/subgroups/differences that were identified and accounted for, and (x) subpopulations that were identified using objective criteria [18]. Disagreements were resolved by consensus.
2.7. Summary Measures and Statistical Analysis
The outcome measure for this study was the proportion of positive responses in each dimension. STATA statistical software V.14.2 was used for all calculations.
For each HSOPS dimension, meta-analyses were performed by grouping the positive scores using the random effects model described by DerSimonian and Laird and the double-arcsine transformation for variance stabilization as proposed by Freeman-Tukey [19, 20]. The prediction confidence interval was also calculated [20, 21].
Heterogeneity was assessed by calculating the inverse variance in a fixed-effects model, which was expressed as a percentage of the I2 statistic [20, 22]. Among the study characteristics, possible causes of heterogeneity were investigated: year of publication, proportion of physicians, proportion of nurses, quality scores, and continent where the study was performed. A meta-regression was performed of the double-arcsine transformed results in the method-of-moments model with a restricted maximum likelihood and a modified coefficient variance as suggested by Knapp and Hartung [23, 24]. Thus, the β coefficient, the probability (p value), and the residual heterogeneity were calculated. Values of p < 0.05 were deemed significant.
Publication bias (small study effect) was investigated using three approaches for each dimension. The first consisted of a regression of the log odds of the positive results against their standard errors (Egger’s test). The second strategy was a regression of the odds against the reciprocal of the sample size (Peters’ test). For both tests, probability values below 0.10 were deemed significant [25]. The third approach included a visual assessment of asymmetry in two funnel plots: one that compared sample size against log odds and the other that compared the log odds against the standard errors [25, 26].
3. Results
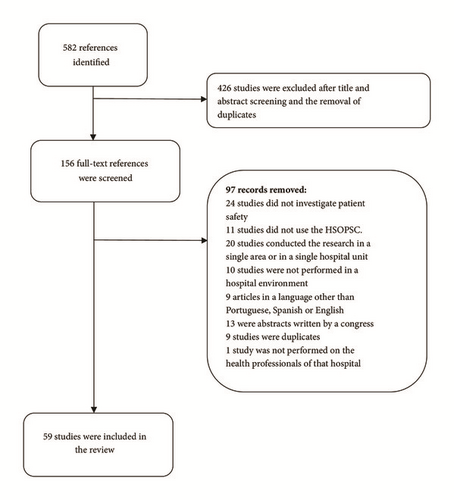
The search retrieved 582 studies, of which 59 were included [5, 27–83] (Figure 1).
Eleven studies were published prior to 2011; and 48, between 2011 and 2015 (Table 2). Twenty-nine were conducted in Asia (of note, eight in Iran), 18 occurred in Europe, and 14 occurred in American continent, of which 11 were in the US. Two studies were located in Eurasia (Turkey) and one was in Africa (Egypt).
| Continent | Countries | Author, year | Sample size | Proportion of physicians | Proportion of nurses | Quality score |
|---|---|---|---|---|---|---|
| Africa | Egypt | Aboul-Fotouh, 2012 | 510 | 50.0 | 32.4 | 10 |
| America | Brazil | Silva-Batalha, 2015 | 301 | - | 18.9 | 9 |
| Colombia | Gómez Ramírez, 2011 | 201 | - | 54.7 | 10 | |
| United States of America | Blegen, 2010 a | 368 | 40.0 | 33.0 | 9 | |
| 434 | 34.0 | 30.0 | ||||
| Bump, 2015 | 955 | 100.0 | - | 7 | ||
| Campbell, 2010 | 2,163 | 19.9 | 80.1 | 10 | ||
| Dupree, 2011 b | 163 | 25.0 | 37.0 | 10 | ||
| 234 | 21.0 | 48.0 | ||||
| 325 | - | - | ||||
| Halbesleben, 2008 | 148 | - | 100.0 | 10 | ||
| Jones, 2013 | 2,137 | 9.4 | 32.0 | 10 | ||
| Mardon, 2010 | 179 | - | - | 10 | ||
| Patterson, 2015 | 247,140 | 4.7 | 51.2 | 10 | ||
| Ulrich, 2014 | 979 | - | 100.0 | 10 | ||
| Wagner, 2013 c | 196,462 | 4.0 | 36.0 | 8 | ||
| Wu, 2013 d | 106,710 | - | 100.0 | 9 | ||
| Mexico | Castañeda-Hidalgo, 2013 | 195 | - | 90.3 | 10 | |
| Asia | Saudi Arabia | Aboshaiqah, 2010 | 445 | - | 100.0 | 10 |
| Aboshaiqah, 2013 | 498 | - | 100.0 | 10 | ||
| Alahmadi, 2010 | 1,224 | 8.3 | 60.0 | 9 | ||
| Al-Ahmadi, 2009 | 1,224 | 8.8 | 63.7 | 9 | ||
| Al-Awa, 2012 | 605 | - | 100.0 | 7 | ||
| El-Jardali, 2014 | 2,572 | 8.7 | 50.1 | 10 | ||
| China | Nie, 2013 | 1,160 | 25.9 | 62.2 | 8 | |
| Shu, 2015 | 2,230 | 31.0 | 69.0 | 10 | ||
| Wang, 2014 | 463 | - | 100.0 | 10 | ||
| Iran | Adibi, 2012 | 90 | 7.8 | 71.1 | 3 | |
| Al-Mandhari, 2014 | 398 | 20.9 | 59.5 | 10 | ||
| Ammouri, 2015 | 414 | - | 100.0 | 10 | ||
| Bahrami, 2013 e | 135 | - | 100.0 | 9 | ||
| 135 | - | 100.0 | ||||
| Bahrami, 2014 f | 113 | - | 100.0 | 10 | ||
| 189 | - | 100.0 | ||||
| Davoodi, 2013 | 922 | 10.0 | 77.0 | 10 | ||
| Moussavi, 2013 | 175 | 32.6 | 41.7 | 10 | ||
| Raeissi, 2015 | 461 | 15.2 | 51.0 | 10 | ||
| Japan | Fujita, 2013 h | 6,963 | 8.5 | 58.1 | 10 | |
| Fujita, 2014 | 8,700 | 9.3 | 46.4 | 9 | ||
| Wu, 2013 d | 4,047 | - | 100.0 | 9 | ||
| Jordan | Khater, 2015 | 658 | - | 100.0 | 10 | |
| Saleh, 2015 | 242 | - | 100.0 | 10 | ||
| Lebanon | El-Jardali, 2010 | 6,807 | 3.7 | 57.8 | 10 | |
| Palestine | Hamdan, 2013 | 1,408 | 20.0 | 49.2 | 10 | |
| Taiwan | Chen, 2012 | 788 | 29.2 | 60.7 | 10 | |
| Chen, 2010 | 788 | 29.2 | 60.7 | 10 | ||
| Fujita, 2013 h | 10,019 | 9.7 | 57.0 | 10 | ||
| Wagner, 2013 c | 10,146 | 10.0 | 58.0 | 8 | ||
| Wu, 2013 d | 5,714 | - | 100.0 | 9 | ||
| Eurasian | Turkey | Günes, 2015 | 554 | - | 100.0 | 8 |
| Ugurluoglu, 2012 | 108 | 27.8 | 42.6 | 9 | ||
| Europe | Belgium | Vlayen, 2012 | 55,225 | 8.8 | 49.8 | 10 |
| Hellings, 2010 g | 3,626 | 12.2 | 60.5 | 10 | ||
| 3,940 | 11.7 | 64.1 | ||||
| Vlayen, 2015 | 47,136 | 9.6 | 52.5 | 9 | ||
| Croatia | Brborovic, 2014 | 148 | - | 100.0 | 8 | |
| Sklebar, 2013 | 560 | - | - | 5 | ||
| Scotland | Agnew, 2013 | 1,866 | - | 53.0 | 5 | |
| Western Slovakia | Mikusová, 2012 | 1,787 | 13.6 | 50.5 | 9 | |
| Spain | Gama, 2013 | 1,113 | 24.7 | 45.0 | 10 | |
| Saturno, 2008 | 2,503 | - | - | 8 | ||
| Skodova, 2011 | 299 | - | 40.1 | 10 | ||
| Finland | Kuosmanen, 2013 | 283 | 6.4 | 82.2 | 6 | |
| Turunen, 2013 | 832 | - | 100.0 | 6 | ||
| Italy | Bagnasco, 2011 | 724 | 35.0 | 26.0 | 7 | |
| Norway | Ballangrud, 2012 | 220 | - | 100.0 | 10 | |
| Farup, 2015 | 185 | 14.1 | 61.6 | 10 | ||
| Netherlands | Smits, 2012 | 542 | 16.5 | 74.0 | 6 | |
| Wagner, 2013 c | 3,779 | 12.0 | 53.0 | 8 | ||
| United Kingdom | Lawton, 2015 | 648 | - | 100.0 | 8 |
- Note. a,b,g Different years: a2006 and 2007, b2005, 2008, and 2011, and g2005 and 2007; c,dsame study conducted on different continents; e,fsame study performed in different hospitals; hsame study conducted on different countries.
The studies included 755,415 professionals who answered the HSOPS, of which 55.4% were nurses and 5.2% were physicians. Sample sizes ranged from 90 to 247,140 participants (Table 2). The largest studies were conducted in the US [63, 64, 78] while the smallest studies were Iranian[41].
One study surveyed the same institution three times on different years [37]. Thirty-three studies included a variety of professionals, 22 surveyed nursing staff exclusively and one surveyed only physicians [73]. Four investigations were multi-center studies [31, 35, 51, 66] (surveys administered at different hospitals in the same country) and three were international multi-center surveys [54, 63, 64].
The mean score for methodological quality of the evaluated articles, on a scale of 0 to 10, was 9.0 points, with 34 studies that achieved the maximum score (Table 2). Considering the appraisal criteria, 19 studies showed errors in the participant recruitment process, 12 neglected the calculation of sample size, and nine failed to report response rates.
The results of the meta-analyses of the 12 HSOPS dimensions are presented in Table 3. Five had less than 50% of positivity in the dimensions of “communication openness”, “frequency of events reported”, “staffing”, “handoffs and transitions”, and “nonpunitive response to errors”. Only the dimension of “teamwork within units” produced positive responses in 75% of those surveyed, which was the highest percentage.
| Dimensions | Positive responses, % (95% CI) | I2 (%) |
|---|---|---|
| Teamwork within units | 75 (73-76) | 97.9 |
| Supervisor/Manager expectations and actions that promote patient safety | 61 (59-64) | 99.0 |
| Organizational learning and continuous improvement | 70 (67-73) | 99.3 |
| Management support for patient safety | 53 (48-57) | 99.6 |
| Overall perceptions of patient safety | 54 (51-56) | 98.9 |
| Feedback and communication about error | 54 (51-57) | 99.1 |
| Communication openness | 47 (44-51) | 99.4 |
| Frequency of events reported | 48 (45-52) | 99.5 |
| Teamwork across units | 50 (47-53) | 98.9 |
| Staffing | 36 (33-40) | 99.5 |
| Handoffs and transitions | 45 (44-47) | 97.7 |
| Nonpunitive response to errors | 33 (30-37) | 99.4 |
- Note. Positive responses in percentage. 95% CI, 95% predictive confidence interval.
A survey that was conducted in Norway in 2012 produced positive responses in 78.8% of the “nonpunitive response to errors” dimension,[42] and an analysis performed in Spain, reported 3.7% positivity for the dimension of “management support for patient safety”[39], while seven others had positive scores of less than 30% [28, 36, 40–42, 55, 72].
The meta-analyses detected high heterogeneity values across the HSOPS dimensions, with all that were above 97%. The meta-regression showed that three dimensions were influenced by the proportion of doctors in the dimensions of “overall perceptions of patient safety”, “feedback and communication about error”, and the “frequency of events reported” (Table 4). The continent where the survey was held significantly affected the dimensions of “supervisor/manager expectations and actions promoting patient safety” (America 72-76% versus others 42-67%), “overall perceptions of patient safety” (America 58-67% versus others 30-55%), “communication openness” (America 59-63% versus others 31-63%), “staffing” (America 47-64% versus others 31-63%), and “nonpunitive response to errors” Asia and Eurasian 23-32% versus Europa and America 36-58%). Only the dimensions of “organizational learning-continuous improvement”, “teamwork within units”, and “handoffs and transitions” were not positive for small study effects. Funnel plot inspections showed asymmetry in all dimensions (data not shown).
| Dimensions | Double arcsine coefficient (β), p value, residual heterogeneity (I2, %) of meta-regression | Publication bias | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Doctors | Nurses | Quality score | Continent | p value | ||||||||||||
| β | p value | I2 | β | p value | I2 | β | p value | I2 | β | p value | I2 | β | p value | I2 | Egger’s test | Peters’ test | |
| Teamwork within units | 0.013 | 0.424 | 97.9 | -0.006 | 0.166 | 98.5 | <0.001 | 0.808 | 98.0 | 0.008 | 0.416 | 97.8 | -0.029 | 0.458 | 97.8 | 0.071 | 0.005 |
| Supervisor/Manager expectations and actions that promote patient safety | -0.031 | 0.125 | 99.0 | -0.005 | 0.154 | 98.9 | -0.005 | 0.100 | 98.1 | 0.001 | 0.926 | 98.2 | -0.139 | <0.001 | 95.8 | 0.001 | <0.001 |
| Organizational learning and continuous improvement | 0.018 | 0.374 | 99.3 | <0.001 | 0.936 | 99.5 | <0.001 | 0.224 | 99.3 | 0.001 | 0.953 | 99.2 | 0.068 | 0.146 | 99.3 | 0.980 | 0.490 |
| Management support for patient safety | <0.001 | 0.987 | 99.6 | -0.012 | 0.064 | 99.6 | -0.012 | 0.307 | 99.6 | 0.002 | 0.903 | 99.6 | -0.019 | 0.776 | 99.5 | 0.022 | 0.016 |
| Overall perceptions of patient safety | -0.012 | 0.481 | 98.9 | -0.007 | 0.039 | 98.7 | -0.007 | 0.840 | 98.4 | 0.004 | 0.687 | 98.7 | -0.078 | 0.018 | 97.9 | 0.021 | 0.016 |
| Feedback and communication about error | 0.008 | 0.694 | 99.2 | -0.007 | 0.043 | 99.2 | -0.007 | 0.504 | 98.9 | 0.011 | 0.329 | 99.1 | -0.026 | 0.544 | 98.6 | 0.090 | 0.077 |
| Communication openness | -0.019 | 0.390 | 99.4 | -0.005 | 0.177 | 99.5 | -0.005 | 0.739 | 99.1 | -0.001 | 0.913 | 99.3 | -0.131 | 0.002 | 98.0 | 0.017 | 0.023 |
| Frequency of events reported | 0.003 | 0.892 | 99.5 | -0.009 | 0.049 | 99.7 | -0.009 | 0.606 | 99.5 | 0.022 | 0.072 | 99.5 | -0.070 | 0.145 | 99.4 | 0.074 | 0.089 |
| Teamwork across units | 0.013 | 0.526 | 98.9 | -0.004 | 0.385 | 99.2 | -0.004 | 0.467 | 98.9 | 0.012 | 0.270 | 98.7 | -0.027 | 0.539 | 97.7 | 0.114 | 0.115 |
| Staffing | -0.016 | 0.544 | 99.5 | -0.003 | 0.570 | 99.5 | -0.003 | 0.460 | 99.2 | 0.001 | 0.923 | 99.3 | -0.132 | 0.012 | 98.3 | 0.005 | 0.008 |
| Handoffs and transitions | 0.010 | 0.562 | 97.5 | -0.006 | 0.053 | 98.0 | -0.006 | 0.273 | 97.7 | 0.003 | 0.755 | 97.7 | -0.031 | 0.422 | 97.6 | 0.503 | 0.372 |
| Nonpunitive response to errors | -0.041 | 0.159 | 99.4 | -0.002 | 0.671 | 99.6 | -0.002 | 0.771 | 99.3 | 0.009 | 0.577 | 99.4 | -0.198 | <0.001 | 99.0 | 0.044 | 0.111 |
4. Discussion
The present review made it possible to identify studies that used HSOPS and to evaluate the safety culture of patient in hospital setting worldwide. There are still aspects in the safety culture of patient that deserve attention to improve patient care in these environments. HSOPS was used both in a specific class of professionals as well as to all hospital staff.
The dimension “nonpunitive response to errors” was the one with the lowest score and “teamwork among the units” the highest score regarding the patient safety items addressed in the survey. Similar results were found in a systematic review and meta-analysis of the HSOPS conducted to assess the patient′s safety culture in hospitals in Iran [84]. This review included Iranian surveys conducted between 2000 and 2014 and used a writing tool as an instrument of critical evaluation, with calculation of meta-analysis using simple means of the domains.
The weakest dimensions were those that were related to communication problems and staffing, with the “nonpunitive response to error” the worst rated dimension. This may reflect the culpability culture of the hospitals but also a comprehensiveness problem. This domain has only negative questions, which induces misunderstanding and less reliability in questionnaires [85]. Dimensions with lower scores may reflect the wording and not the limitation in safety culture. External analyses of HSOPS [86] showed possible weaknesses in its psychometric properties.
Evaluating perceptions of the culture of safety implies the consideration of a number of factors and characteristics pertaining to the hospital setting [87]. Management that is committed to safety culture, effective leadership support, effective communication, sufficient staffing, incentives to capacity-building, and interdisciplinary teamwork are just some of those factors [72]. Unities with different profiles in terms of their constitution and organization (specialized intensive care units, emergency departments, surgical suites, and wards) are found in hospitals [88]. In those unities, perceptions of patient safety vary between practitioners [32, 42]. In this review, the influence of the medical staff was noted for some dimensions. Thus, to assess the perception of patient safety through surveys, the influence of the context of each unit and different professionals should also be considered.
Studies that evaluated the culture of safety have shown contrasting perceptions regarding patient safety in different professionals, and in one study, physicians showed a less positive perception compared to nurses [89] and more positive perceptions compared to the nursing staff in another [90, 91].
The continent where the study was conducted was a source of variability of results across studies. In international multi-center studies [54, 63], a greater proportion of positive scores was found in the US than elsewhere. In addition to the cultural differences [63], the HSOPS was developed in the US; hence its use is more disseminated in that country, a fact that becomes evident in the sample sizes. Another factor detected in those multi-center studies is the larger number of nurses in US hospitals compared to other countries [54], a fact that is attributable to the way hospitals adapt the numbers of nurses to their demand and hire temporary staff.
In a Norwegian study [42], a salient strength was found in the “nonpunitive response to error” dimension. Another study conducted in the same country [92] found a similar value for this dimension. In most studies that were conducted in a variety of countries, this dimension yielded low scores, which indicated the need for improvement. Other investigations were pursued [28, 32, 55, 58, 60, 63, 70] with higher positive percentages in this dimension and seven were found with positive scores above 50%. It was noted that, in the settings where these surveys were administered, a climate of encouragement existed in the management staff who promoted reporting and learning from errors.
Included studies showed good methodological quality, which showed no effect on the heterogeneity, partly attributable to the proportion of physicians and the location where the surveys were administered. The statistical tests indicated that small study effect was present and publication bias may have influenced the results. Studies published in scientific conferences and in other gray literature were not included and the restriction of only publications in Portuguese, English, and Spanish may have stressed out this effect. With the purpose of extending the usability and determining the applicability of the HSOPS, all sample sizes and professional categories were included, which influenced the high heterogeneity.
As a psychometric tool, HSOPS adaptation versions [93] are subject to inconsistences due to language and cultural particularities. A previous validation of the tool was not an eligibility criterion in our review. This may have overestimated or underestimated our findings and probably contributed to the high heterogeneity. HSOPS showed good psychometric properties of safety culture [10] when assessed by its development group. Like other questionnaires, the link between the society culture and patient safety may be an issue and could be better explored by qualitative assessment.
The methods of this review were based on internationally recommended standards [94]. Thus, paired reviewers worked on the inclusion, evaluation, and data extraction steps. Data analysis relied on statistical calculations grouped according to relevant variables. The use of the HSOPS is still emerging in some countries. In accordance with the worldwide trend towards patient safety in the health services, this systematic review could foster the use and dissemination of the HSOPS.
5. Conclusions
The culture of culpability is pervasive in most of the hospitals that measured the culture of safety using the HSOPS. This behavior reduces error reporting and the likelihood that corrective measures would be implemented. Effective communication, feedback following reporting, engaged leadership, and environments focused on learning from errors are factors that can lead to improvement.
Disclosure
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors’ Contributions
Julia Hiromi Hori Okuyama selected the studies, extracted the data, assessed the methodological quality of included studies, and drafted the manuscript. Tais Freire Galvao selected studies, extracted the data, and revised the manuscript for important intellectual content. Marcus Tolentino Silva designed the study, analyzed the data, mentored the drafting of the manuscript, and revised it for important intellectual content. All authors agree to be responsible for all aspects of the study and approved the final version of the manuscript.
Acknowledgments
The authors are grateful to graduate students in pharmacy, Henderson Hirata, for his participation in data extraction and Tathiany Torres, for her participation in critical appraisal of included studies.
Open Research
Data Availability
The data used to support the findings of this study are available upon request from the corresponding author.