Prevalence of Cardiovascular Disease and Associated Risk Factors among Adult Population in the Gulf Region: A Systematic Review
Abstract
Background. CVD is a principal cause of mortality and disability globally. Objective. To analyse the epidemiological data on CHD, strokes, and the associated risk factors among adult population in the Gulf countries. Methods. A systematic review of published articles between 1990 and 2014 was conducted. Results. The analysis included 62 relevant studies. The prevalence of CHD was reported to be 5.5% in Saudi Arabia. The annual incidence of strokes ranged from 27.6 to 57 per 100 000 in the Gulf countries with ischaemic stroke being the most common subtype and hypertension and diabetes being the most common risk factors among stroke and ACS patients. The prevalence of overweight and obesity ranged from 31.2% to 43.3% and 22% to 34.1% in males and from 28% to 34.3% and 26.1% to 44% in females, respectively. In males, the prevalence of hypertension and diabetes ranged from 26.0% to 50.7% and 9.3% to 46.8%, respectively; in females these ranged from 20.9% to 57.2% and 6% to 53.2%, respectively. The prevalence of inactivity was from 24.3% to 93.9% and 56.7% to 98.1% in males and females, respectively. Relatively more males (13.4% to 37.4%) than females (0.5% to 20.7%) were current smokers. Available data indicate poor dietary habits with high consumption of snacks, fatty foods, sugar, and fast food. Conclusion. Effective preventative strategies and education programs are crucial in the Gulf region to reduce the risk of CVD mortality and morbidity in the coming years.
1. Introduction
Cardiovascular disease (CVD) is now recognized as the leading cause of death and disability worldwide [1]. The World Health Organization (WHO) estimated that in 2008, out of 17.3 million CVD deaths globally, heart attacks (myocardial infarction) and strokes were responsible for 7.3 and 6.2 million deaths, respectively [1]. According to the INTERHEART and INTERSTROKE studies, hypertension, diabetes, dyslipidaemia, obesity, smoking, physical activity, poor diet, and alcohol consumption are the most common risk factors for myocardial infarction (heart attack) and strokes worldwide [2, 3].
The Gulf Cooperation Council (GCC) is cooperation between Saudi Arabia, Bahrain, Oman, Qatar, the United Arab Emirates, and Kuwait. In 1981, the GCC was created to encourage investment and to adopt free trade between member states. This agreement also contributed to several fields including: education, culture, tourism, social opportunities, and health among the GCC members. The discovery of oil and other natural resources such as gas in the GCC countries including Saudi Arabia led to rapid development and economic growth [4]. Along with the rapid socioeconomic growth in the Gulf countries, there has been a change in lifestyle such as an increased consumption of poor quality foods and the adoption of a sedentary lifestyle [5], and as a consequence the rates of CVD and associated risk factors among the Gulf population have also increased; the rates sometimes exceed that of developed countries [5]. Furthermore, the number of deaths resulting from ischemic heart disease and hypertensive heart disease in the Middle East and North Africa region (including the GCC countries) was 294/100,000 and 115/100,000 respectively. Also, the number of disability-adjusted life years (DALYs) resulting from ischemic and hypertensive heart disease is 3702/100,000 and 1389/100,000, respectively, in the same region [6]. The WHO estimated the total number of noncommunicable diseases resulting in death in the GCC states in 2008. CVD was estimated to account almost half of the deaths in Oman and Kuwait, 49% and 46%, respectively. The rate of CVD deaths was also high in Saudi Arabia, the UAE, Bahrain, and Qatar 42%, 38%, 32%, and 23%, respectively [7]. Although some systematic reviews on the prevalence of CVD and/or CVD risk factors in the Middle East region have been published [8, 9], these reviews were limited to either CVD risk factors only [8], or specific gender [9]. To our knowledge, this is the first systematic review that provides a comprehensive analysis on the prevalence of CHD, strokes, and associated risk factors in the Arabic Gulf countries. The aim of this paper was to review the epidemiology of CHD, strokes, and the related risk factors among the adult population in the GCC.
2. Methods
2.1. Data Sources
An extensive literature search was conducted on the prevalence of CHD and incidence of strokes and the burden of associated risk factors to identify articles or reports published between 1990 and 2014 using Pro-Quest Public Health, MEDLINE, PubMed, Google Scholar, and World Health Organization (WHO) website. A manual search of reference lists of original studies was searched. In addition, checking the review articles, contacting authors, the official website of the Gulf Heart Association were also searched http://www.gulfheart.org/ and the section labelled “GHA studies” was specifically scanned. The search terms used were shown in Box 1.
-
Box 1: Selected search terms.
-
Cardiovascular disease
-
(1) “Cardiovascular disease” OR “epidemiology of cardiovascular disease” OR
-
“coronary heart disease” OR “epidemiology of coronary heart disease”
-
Strokes
-
(2) “stroke” OR “epidemiology of stroke” OR “incidence of stroke”
-
Associated risk factors
-
(3) “Cardiovascular risk factors” OR “coronary heart disease risk factors” OR
-
“stroke risk factors” OR “diabetes mellitus” OR “epidemiology of diabetes
-
mellitus” OR “NIDDM” OR “dyslipidaemia” OR “epidemiology of
-
dyslipidaemia” OR “hypercholesterolemia” OR “high cholesterol” OR
-
“smoking” OR “tobacco use” OR “epidemiology of smoking” OR
-
“hypertension” OR “high blood pressure” OR “epidemiology of
-
hypertension” OR “obesity” OR “overweight” OR “BMI” OR “epidemiology
-
of obesity” OR “physical activity” OR “exercise” OR “epidemiology of
-
physical activity” OR “Food consumption patterns” OR “eating habits” OR
-
“dietary patterns” OR “food”
-
The Gulf region
-
(4) “Gulf region” OR “Arab countries” OR “GCC” OR “Saudi Arabia” OR
-
“Kuwait” OR “Oman” OR “Bahrain” OR “Qatar” OR “United Arab Emirates”
-
(5) #1 AND #4
-
(6) #2 AND #4
-
(7) #3 AND #4
-
(8) #1 AND #3 AND #4
-
(9) #2 AND #3 AND #4
2.2. Study Selection
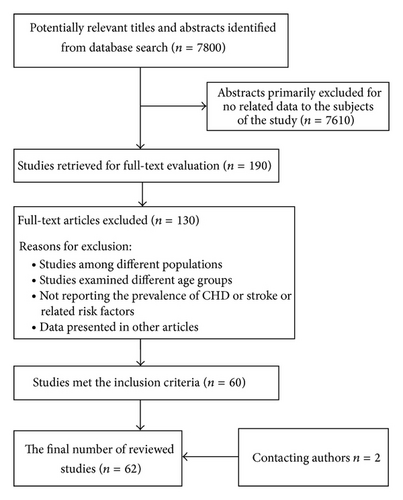
A total of 7800 articles were identified in initial search. The titles and abstracts of all articles of potential interest were reviewed for inclusion and exclusion of studies. The criteria for selected studies aimed to include studies that indicated the prevalence of CHD and/or stroke and/or at least one of the associated risk factors: diabetes, hypertension, obesity, dyslipidaemia, dietary habits, smoking, and physical activity. All the included studies were required to only include individuals over 18. The CHD and stroke studies were not restricted by sample size due to the limited numbers of these studies in the GCC countries. However, all the included studies that examined the burden of the risk factors were restricted with a sample size that exceeded 500 except for diet studies. All selected studies were required to relate to at least one of the GCC populations. Only studies published in English and where full manuscripts were included. Studies were published in abstract form and those on congenital heart disease or other CVDs were excluded. A total of 190 full-text papers were identified and further reviewed. Finally, 62 articles including two articles by contacting authors directly were included in this review. Figure 1 summarizes the selection process of the reviewed studies.
2.3. Data Abstraction and Quality Assessment
Data extracted for each study included first author and publication year, sample size, demographic characteristics, the country of study, place of study, study objectives, year(s) of survey, response rate, study methods, the definition of CHD and/or stroke and/or associated risk factors, and the prevalence of CHD and/or stroke and/or associated risk factors. The quality of selected studies was assessed according to the Centre for Reviews and Dissemination guidelines [10]. Since there are few papers that addressed the study questions, no studies were excluded for their qualities. The quality assessment checklist of the included studies in the systematic review is shown in the far-right column of Tables 1 and 2.
Reference country |
Year(s) of survey | Total sample | Age, range, and mean | Sampling methods | Study design | Response rate (%) | Diagnostic criteria | The main outcomes (CHD/stroke/associated risk factors/mortality rates) | Quality assessment checklist (*) |
|---|---|---|---|---|---|---|---|---|---|
| CHD studies | |||||||||
|
1995–2000 |
|
30–70 | Two-stage stratified cluster | National cross-sectional survey | NR | WHO MONICA (monitoring trends and determinant in cardiovascular disease) |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2005-2006 |
|
57.1 | No sampling (all ACS patients included with no excluded patients) | Prospective study | NR | The Joint Committee of the European Society of Cardiology/American College of Cardiology (ACC) | Risk factors of ACS: DM 56%, HTN 48%, smoking 39%, and hyperlipidaemia 31% | 1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
|
2007 |
|
56 | No sampling (all ACS patients included with no excluded patients) | Prospective multinational study | NR | The American College of Cardiology clinical data standards (ACC)/DM, hypertension, dyslipidaemia defined when patients known to have these risk factors and on treatment/regular smoking defined as 1 cigarette per day/nonsmoker after stopping 12 months ago |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
|
2007 |
|
|
No sampling (all ACS patients included with no excluded patients) | Prospective multinational study | NR | The American College of Cardiology clinical data standards (ACC)/DM, hypertension, dyslipidaemia defined when patients known to have these risk factors and on treatment/regular smoking defined as 1 cigarette per day/nonsmoker after stopped 12 months ago |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-N, 7-NA |
| Strokes studies | |||||||||
|
1982–1992 |
|
|
Nonrandom sampling (500 medical records of stroke patients) | Retrospective study | NR | NA |
|
1-Y, 2-Y, 3-Y, 4-Not well described, 5-N, 6-N, 7-NA |
|
1989, 1992 and 1993 | Not clear | 60.6 years | Nonrandom (all patients with first-ever stroke, patients with previous stroke were excluded) | Prospective study | NR | WHO definition for diagnosing stroke/HC defined as more than 5.78 mmol/L/smoking as any current use of cigarette/hypertension and DM were not clear |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2008 |
|
60.5 years | Nonrandom (all ischemic stroke patients, there was an inclusion criterion) | Retrospective study | NR | Stroke defined according to WHO/stroke subtypes was defined according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria |
|
1-Y, 2-Y, 3-Y, 4-N, 5-N, 6-Y, 7-NA |
|
1995–1999 |
|
64.1 years | No random (all ischemic stroke patients included) | Retrospective study | NR | Stroke defined according to WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-N, 7-NA |
|
2005–2008 |
|
53 years | Nonrandom (all patients diagnosed with PCS stroke, there was an inclusion criterion) | Prospective study | NR | Stroke defined according to Kidwell and Warach/DM as fasting blood glucose >140 mg/dL or in medication/hypertension as >140/90 mmHg or on medication/dyslipidaemia as TC >5 mmol/L/smokers as currently smokers or during the last 12 months/obesity as BMI ≥30 |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Partly, 7-NA |
|
1989-1990 and 1991–1993 |
|
All | Nonrandom (all Saudi patients with first stroke were included, and there was excluded patients) | Prospective register | NR | The WHO multicentre Stroke Register/hypertension defined as BP >160/90 mmHg/DM defined as fasting blood sugar above 6.6 mmol/L |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1997–2000 |
|
63 years | Nonrandom (all stroke patients included, no excluded patients) | Retrospective study | NR | NR |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-N, 7-NA |
|
1997 |
|
57 years | Nonrandom (all stroke patients records were reviewed, and only first-ever stroke cases were included) | Retrospective study | NR | Stroke defined according to the WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
|
1995 |
|
≥20 | Nonrandom (all stroke cases were reviewed) | Retrospective study | NR | Stroke defined according to the WHO criteria |
|
1-Y, 2-Y, 3- Y, 4-N, 5-N, 6-N, 7-NA |
|
2001 |
|
61.2 years | Nonrandom (the data of all stroke patients were reviewed, and there were inclusion criteria) | Retrospective study | NR |
|
Risk factors: HTN 69%/DM 51%/dyslipidaemia 57%/obesity 30%/smoking 26%/CAD 23% | 1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
|
2006-2007 |
|
58.9 years | No sampling (all ischemic stroke patients were included, and there were inclusion criteria) | Prospective registry | NR | HTN: BP >160/90 mmHg or on medication/DM: past history or elevated A1c or on medication/dyslipidaemia: TC >5.2 mmol/L or TG >1.7 mmol/L or HDL >1.0 mmol/L LDL <3.4 mmol/L/BMI ≥30 kg/m²/smokers: regular smoking within the last 5 years |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
1993 |
|
NR | No sampling (all Saudi living in the Thuqbah area were screened) | Community-based cross-sectional survey | NR | Stroke defined “sudden or rapid onset of focal or global brain dysfunction of vascular origin lasting for more than 24 h or leading to death especially if diagnosed by physicians” |
|
1-Y, 2-Y, 3-Y, 4-N, 5-Y, 6-N, 7-NA |
- M, male; F, female; U, urban; R, rural; DM, diabetes; IFG, impaired fasting glucose; HC, hypercholesterolemia; TG, triglyceride; TC, total cholesterol; HDL, high-density lipoprotein; LDL, low-density lipoprotein; HTN, hypertension; SBP, systolic blood pressure; DBP, diastolic blood pressure; NR, not reported; ACS, acute coronary syndrome; BMI, body mass index; Y, yes; N, no; and NA, not applicable. (*) the quality assessment checklist assessed according to the Centre for Reviews and Dissemination guidelines (CRD) for nonrandomized studies: 1- Was the aim of the study stated clearly? 2- Was the methodology stated? And was it appropriate? 3- Were appropriate methods used for data collection and analysis? 4- Was the data analysis sufficiently rigorous? 5- Were preventive steps taken to minimize bias? 6- Were limitations of the study discussed? 7- In systematic review, was search strategy adequate and appropriate?
Reference country |
Year(s) of survey | Total sample | Age, mean, and min to max | Sampling methods | Study design | Response rate (%) | Diagnostic criteria and/or dietary assessment methods | The main findings and prevalence data | Quality assessment checklist (*) |
|---|---|---|---|---|---|---|---|---|---|
|
1996-1997 |
|
≥40 | Random stratified sampling | Cross-sectional study | 76.6 | HC: TC >6.2 mmol/L/overweight BMI for men ≥27.2 women ≥26.9/HTN: SBP ≥140 mmHg or DBP ≥95 or on medication |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1990–1993 |
|
≥20 | Multistage stratified cluster sampling | National epidemiological cross-sectional survey | 69 | Overweight and obesity defined according the WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1995–2000 |
|
30–70 | Two-stage stratified cluster sampling | National epidemiological cross-sectional survey | 98.2 | DM was defined according to the WHO |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1996 |
|
18–26 | Random sampling | Cross-sectional study | 91 | Current smokers: currently smoking at least 1 cigarette per day |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1990–1993 |
|
30–64 | Multistage stratified cluster sampling | National Cross-sectional survey | 92 | DM: the random serum glucose according to the WHO criteria or self-reported/HC: mild (5.2–6.2 mmol/L) severe (>6.2 mmol/L)/HDL: <0.9 mmol/L/BMI: WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1995–2000 |
|
30–70 | Two-stage stratified cluster sampling | National epidemiological cross-sectional survey | NR | Overweight and obesity defined according to the WHO |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2001 |
|
35–85 | Cluster sampling | Cross-sectional study | NR | HTN: BP ≥140 mmHg systolic and 90 mmHg diastolic or self-reported with medication or both |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1996 |
|
≥19 | Random sampling | Cross-sectional study | 75 | Regular active: physically active for 30 or more minutes, 2 or more days a week | Physically inactive 53%, irregularly active 27.5%, and physically active on a regular basis 19% | 1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-N, 7-NA |
|
1995–2000 |
|
30–70 | Two-stage stratified cluster sampling | National epidemiological cross-sectional survey | NR | HTN: SBP ≥140 mmHg or DBP ≥90 mmHg |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1995–2000 |
|
30–70 | Two-stage stratified cluster sampling | National epidemiological cross-sectional survey | NR | Physically active: 30 minutes or more of at least moderate-intensity activity for three or more times per week/physical inactivity: participants who did not meet the physically active criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
1995–2000 |
|
30–70 | Two-stage stratified cluster sampling | National epidemiological cross-sectional survey | 97 | HC: TC ≥5.2 mmol/L/TG: ≥1.69 mmol/L |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
1999-2000 |
|
35.5 | Random sampling | Cross-sectional study | 70 | Current smokers: those who regularly or occasionally smoke on a daily, weekly, or monthly basis/nonsmokers: those who never smoked. |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
2004-2005 |
|
≥30 | Nonrandom (all Saudis aged 30 and above who lived in the eastern region in SA were invited to participate in the screening programme) | Cross-sectional survey | 99.1 | Overweight and obesity defined according to the WHO |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
1993–1998 | F: 1764 | 30–70 years | Multistage stratified cluster sampling | CSS | NR | NR/Structured questionnaire |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
2008-2009 |
|
21.1 years | Random selection | CSS | NR | BMI according to the National Institute of Health. HTN according to the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure/Self-reported questionnaire (11 items) |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2009 |
|
30–70 years | Random selection | CSS | NR | NR/Questionnaire and 24 h recall | (i) The most popular food was kabsa (80% in M and 65% in F), fresh fruits (63% in M and 45% in F), vegetables (62% in M and 47% in F) and dates (45%) in both genders and soft drinks (21% in M and 25% in F). | 1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
|
2008–2010 |
|
18–75 | Nonrandom (all UAE nationals residing aged 18 to 75 who were living in Abu Dhabi city were enrolled in the CVD screening program) | Cross-sectional national survey | Measured data (98.7–99.9), self-reported data (86.1–99.8) | Obesity and overweight: according to WHO/DM: past history and on medication or HbA1c ≥6.5% or random glucose 11.1 mmol/L/HTN: self-reported and on medication or SBP ≥140 mmHg or DBP ≥90 mmHg/dyslipidaemia: self-reported on medication or LDL 4.1 mmol/L or HDL 1.0 mmol/L/current smokers: 1 cigarette per day during the last 12 months or 1 water pipe per month during the last 3 months |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
1997 |
|
18–75 | Stratified random sampling | Cross-sectional study | NR | HTN: SBP >140 mmHg and/or DBP >90 mmHg and/or self-reported with medication |
|
1-Y, 2-Y, 3-Y, 4-N, 5-Y, 6-N, 7-NA |
|
1999-2000 |
|
≥20 | Stratified multistage cluster sampling | National epidemiological cross-sectional study | 89 | DM: fasting blood glucose ≥7.0 mmol/L or taking insulin or oral hypoglycemic agents |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2000-2001 |
|
>19 | Stratified random sampling | Cross-sectional survey | 95 | Overweight and obesity were defined according to WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
2002-2003 |
|
18–69 | Multistage cluster random sample | Large cross-sectional survey | 94.9 | Physical inactivity: the person did not meet the following criteria: 3 or more days of various activities during the last week of at least 20 minutes per day or 5 or more days of moderate-intensity activity or walking during the last week of at least 30 minutes per day |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
2010 |
|
|
Convenience sampling | CCS | NR | MetS according to ATP III/24 h recall |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
2001-2002 | F: 400 | 18–25 years | Convenience sampling | CSS | NR | BMI according to WHO/self-administrated questionnaire |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-N, 7-NA |
|
1993 |
|
≥20 | Random selection | CSS | NR | NA/pretested structured questionnaire |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1995-1996 |
|
≥20 | Convenience sampling (all Kuwaiti +20 in the survey area invited to participate) | Cross-sectional study | NR | DM according to the WHO diagnostic criteria for abnormal glucose tolerance |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-N, 7-NA |
|
1996 |
|
33.2 | A three-stage stratified cluster sampling | Cross-sectional national study | 96.5 | Current smokers: if they were smoking at the time of the survey and had smoked more than 100 cigarette in their lifetime, former smokers: if they had smoked more than 100 cigarette in their life but no longer smoking, and never smokers: when they had never smoked or smoked less than 100 cigarettes in their life |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
1998–2009 |
|
20–69 | Convenience sampling (Kuwaitis in health examination for Gov. and Hajj health check-ups and PHCCs) | National cross-sectional survey | NR | HC: moderate (5.2–6.22 TC mmol/L) severe (>6.23 TC mmol/L) | HC prevalence increased from 1998 to 1999 (M 35%; F 31%) until 2006-2007 (M 56%; F 53.6%) and then declined in 2008-2009 (M 33.7%; F 30.6%) | 1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
|
2006 |
|
20–65 | Systematic random sampling | National cross-sectional survey | 77.6 | Overweight and obesity were defined according to the WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N,7-NA |
|
1998–2009 |
|
20–69 | convenience sampling (Kuwaitis in health examination for Gov. and Hajj health check-ups and PHCCs) | National cross-sectional survey | NR | Overweight and obesity defined according to the WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
|
2002–2009 |
|
20–69 | Convenience sampling (Kuwaitis in health examination for Gov. and Hajj health check-ups and PHCCs) | National cross-sectional survey | NR | Diabetes defined according to the WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
|
2006 |
|
|
Random sampling |
|
84.5 | Water-pipe smokers: a person who smoked sheesha and had smoked sheesha for at least one month, people who had not smoked sheesha were classified as sheesha nonsmokers |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-N, 7-NA |
|
2003 |
|
25–65 | A multistage stratified cluster sampling | Cross-sectional study | 80.5 | BP according to the WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2007-2008 |
|
>20 | A multistage stratified cluster sampling | Cross-sectional study | 77.9 | DM was defined according to the WHO expert group |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
1992 |
|
18–67 | Convenient sampling | Cross-sectional survey | NR | Obesity and overweight according to the WHO definition/self-reported of past history of DM and HTN |
|
1-Y, 2-partly, 3-not entirely appropriate, 4-Y, 5-N, 6-N, 7-NA |
|
2000 |
|
≥20 | A multistage stratified probability-sampling | Cross-sectional national survey | 83–91.5 | Current smokers: people who were smoking at the time of the survey and had smoked more than 100 cigarette in their life/former smokers: if they had smoked more than 100 cigarette in their life but no longer smoking/never smokers: if they had never smoked or had smoked less than 100 cigarette in their life |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2000 |
|
≥20 | A multistage stratified probability-sampling design | Cross-sectional national survey | 96 | The WHO criteria for glucose intolerance, HC, and HTN |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
|
|
≥20 | Convenient sampling | Cross-sectional surveys | 92 | Overweight and obesity were defined according to the WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-N, 7-NA |
| 2000 |
|
A multistage stratified probability-sampling design | 91 | 1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA | |||||
|
2001 |
|
≥20 | A probabilistic random sampling | Community based cross-sectional study | 75.5 | DM: FPG ≥5.6 mmol/L or 2hG ≥11.1 mmol/L or on medication/HTN: SBP ≥130 mmHg and/or DBP ≥85 mmHg or on medication/TC: ≥5.2 mmol/L/TG: ≥1.69 mmol/L/HDL: <1.03 mmol/L or on medication for dyslipidaemia/current smokers: people who smoking at the time of the survey/physical activity at leisure time and/or at work |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
2008 |
|
≥18 | A multistage stratified cluster sampling design | Community-based national cross-sectional survey | 93.5 | The WHO criteria for diagnosis HTN, HC, BMI, and DM were used |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-Y, 7-NA |
|
1995-1996 |
|
40–69 | Stratified sampling design | Cross-sectional national survey | 70 |
|
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2002 |
|
30–79 | Probability cluster sampling design | Cross-sectional community-based survey | NR | DM was defined by self-reported past history of diabetes |
|
1-Y, 2-Y, 3-not entirely appropriate, 4-Y, 5-N, 6-Y, 7-NA |
|
2001 |
|
30–79 | Probability cluster sampling design | Cross-sectional community-based survey | NR | Overweight and obesity were defined according to the WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1995-1996 |
|
40–69 | Stratified sampling design | Cross-sectional national survey | 62 | HTN: SBP ≥160 mmHg, DBP ≥95 mmHg or on antihypertensive |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1995-1996 |
|
40–69 | Stratified sampling design | Cross-sectional national epidemiological | 59–70 | DM was defined according to WHO criteria |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
2000 |
|
30–79 | Random cluster-sampling design | Cross-sectional study | NR | Current smokers: a person smoking at least 1 cigarette per day regularly/ex-smokers: person who gave up smoking at least 6 months previously/nonsmoker: person who had never smoked regularly |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-Y, 6-N, 7-NA |
|
1996 |
|
≥20 | Random selection from health care centres attendances | Cross-sectional study | 86.9 | DM was defined according to WHO criteria OR if the person had a previous history of DM |
|
1-Y, 2-Y, 3-Y, 4-Y, 5-N, 6-Y, 7-NA |
- M, male; F, female; U, urban; R, rural; DM, diabetes; IFG, impaired fasting glucose; HC, hypercholesterolemia; TG, triglyceride; TC, total cholesterol; HDL, high-density lipoprotein; LDL, low-density lipoprotein; HTN, hypertension; SBP, systolic blood pressure; DBP, diastolic blood pressure; NR, not reported; ACS, acute coronary syndrome; BMI, body mass index; Y, yes; N, no; and NA, not applicable.
- (*) the quality assessment checklist assessed according to the Centre for Reviews and Dissemination guidelines (CRD) for nonrandomized studies: 1- Was the aim of the study stated clearly? 2- Was the methodology stated? And was it appropriate? 3- Were appropriate methods used for data collection and analysis? 4- Was the data analysis sufficiently rigorous? 5- Were preventive steps taken to minimize bias? 6- Were limitations of the study discussed? 7- In systematic review, was search strategy adequate and appropriate?
2.4. Data Synthesis
A narrative synthesis was performed to identify the study questions. It included describing all the included papers, summarising the findings of the data extracted from each study, and exploring the relationships between the results of the different studies.
3. Results
Of the 62 articles that are reviewed in the present study, 13 were published in the 1990s, another 40 in the 2000s, and 9 in the last four years. Of the included studies, 4 reported data on CHD, 12 on stroke, and 46 on the prevalence of the associated risk factors. Further, of these 62 selected studies, 22 were carried out among Saudi, 8 in Bahraini, 10 in Kuwaiti, 5 in Omani, 6 in Qatari, and 8 in the UAE populations, and 3 were carried out in multiple GCC countries. Regarding the study design; 48 studies were cross-sectional, 7 were retrospective, and 7 were prospective observational studies. Seven studies looked at employees, 4 at university and college students, 8 at primary health care attendants, 14 at CHD and stroke patients, and 29 at the general population. The sample size in CHD and stroke studies ranged from 62 to 23,227 and in the burden of risk factors studies it ranged from 227 to 195,874. Response rates ranged from 59% to 99.8%. The summary of the included articles on CHD and strokes is shown in Table 1, whereas the summary of included articles on the burden of associated risk factors is shown in Table 2.
3.1. CHD and Strokes in the GCC Region
Overall, there is a lack of information on CHD and strokes in Arabic Gulf countries. The only nationally representative study conducted in Saudi Arabia reported the crude prevalence of CHD of 5.5% among the Saudi population [11]. This survey reported a higher prevalence of CHD in males (6.6%) compared to females (4.4%) and in urban Saudis (6.2%) than rural Saudis (4.0%). Further, the prevalence of CHD increased with age from 3.9% in 30–39-year olds to 9.3% in the 60–70-year olds [11].
The Gulf Registry of Acute Coronary Events (Gulf RACE), a project of Gulf Heart Association aimed to describe the characteristics, in-hospital outcomes, and associated risk factors of the acute coronary syndrome patients (ACS) and recruited patients from 64 hospitals in Bahrain, Oman, Qatar, Kuwait, the UAE, and Yemen [12, 13]. The Gulf RACE study reported ACS was more prevalent in male (74%) than female (24%) patients [12]. It also reported a high prevalence of diabetes (40%), hypertension (49%), dyslipidaemia (32%), smoking (38%), and obesity (27%) among ACS patients in the five Gulf countries [13]. The highest rates of the risk factors were in Bahrain and Kuwait, except for smoking, which has the highest rates in the UAE and Kuwait [13]. The prevalence of CVD risk factors was higher in females than males, including diabetes (55% versus 36%), hypertension (70% versus 43%), and dyslipidaemia (44% versus 28%), respectively [12]. Significantly more males (47%) than females (5%) were current smokers [13].
Similarly, the Saudi Project for Assessment of Coronary Events (SPACE) registry reported the characteristics and prevalence of risk factors among ACS patients in Saudi Arabia [14]. The SPACE registry reported that ACS was more frequent in males (77%) than females (23%) [14]. Ischemic heart disease was present in 32% of the study population. The study also reported diabetes to be the most common risk factor for CHD (56%) followed by hypertension (48%), being a current smoker (39%), and hyperlipidaemia (31%) [14].
The available data on strokes and the associated risk factors in the GCC were derived mostly from retrospective hospital-based studies but no population-based studies. The data on strokes and associated risk factors was reported in 12 studies: 4 in Saudi Arabia [15–18], 1 in Bahrain [19], 3 in Kuwait [20–22], 3 in Qatar [23–25], and 1 from multiple GCC countries [26].
Five studies reported the incidence of stroke in Saudi Arabia, Kuwait, Qatar and Bahrain [15, 17, 19, 20, 25]. The incidence of stroke ranged from 27.6 per 100 000 in Kuwait to 57 per 100 000 in Bahrain [15, 17, 19, 20, 25]. Further, the most common type of stroke in the region was ischemic ranging from 69 to 90.1% [15, 17, 22, 25]. There was no data available on the incidence of strokes in Oman and the UAE. Only one study in Saudi Arabia reported on the number of stroke survivors as 186/100,000 [16]. Further, in the majority of stroke studies, the incidence of strokes was higher in males than females across all age groups and it increased with age [15, 17–20, 25], although there was still relatively high stroke incidence in younger age groups (≤45 years) in the GCC region [15, 17, 19, 23]. Across all stroke studies, hypertension (38.1–72.5%) was the most common risk factor, followed by diabetes (20–69.4%) for stroke patients [15, 17–26]. Dyslipidemia was reported in 4–61% of stroke patients [18–24, 26]. Smoking was reported in 1.6–40% of stroke patients in the GCC [15, 17–24, 26].
3.2. The Burden of the CHD and Stroke Risk Factors in the GCC Region
The risk factors for CHD and stroke can be categorized into two groups: metabolic risk factors (obesity, hypertension, diabetes, and dyslipidaemia) and behavioural risk factors (diet, smoking, and physical activity). In this section, the burden of various risk factors among healthy population in the GCC states is described.
3.2.1. Overweight and Obesity
Prevalence of overweight and obesity has been reported in 13 studies: 4 in Saudi Arabia [28, 31, 32, 39], 2 in Bahrain [66, 68], 2 in Kuwait [54, 55], 2 in Oman [63, 65], 1 in Qatar [60], and 2 in the UAE [43, 46].
Based on the available national representative studies, the prevalence of overweight in males and females in the GCC region ranged from 28.8% to 42.4% and from 27.3% to 32.7%, respectively, while the prevalence of obesity in males ranged from 10.5% to 39.2% and in females ranged from 18.2% to 53%. The prevalence of overweight and obesity increased with age with the highest level in the middle age groups (30–39 and 40–49 years) [28, 31, 32, 39, 43, 46, 54, 55, 60, 63, 65, 66, 68]. The obesity rates in urban areas were higher than in rural areas [28, 31, 32, 63]. In general, the prevalence of overweight and obesity is remarkably high in the GCC states and Oman reported the lowest rates of obesity within the region.
3.2.2. Hypertension
The prevalence of hypertension was reported in 10 studies: 3 in Saudi Arabia [27, 33, 35], 1 in Bahrain [69], 2 in Oman [62, 65], 2 in Qatar [58, 60], and 2 in the UAE [43, 44].
The rate of hypertension in the GCC states ranged from 26% to 50.7% in males and from 20.9% to 31.7% in females [33, 35, 43, 44, 58, 62, 65, 69]. Across all studies, the prevalence of hypertension considerably increased with age with the highest rates in the 45–65 age groups. The prevalence of hypertension in Saudi Arabia was lower than Oman, Bahrain, and Qatar but close to the UAE. The lower rate of hypertension in Saudi Arabia may not be true reflection of the situation as the reported study was relatively old [35].
3.2.3. Diabetes Mellitus
The rates of diabetes mellitus in the GCC countries were addressed in 13 studies: 2 in Saudi Arabia [29, 31], 3 in Bahrain [67, 70, 72], 2 in Kuwait [51, 56], 2 in Oman [62, 65], 2 in Qatar [59, 60], and 2 in the UAE [43, 45].
The overall prevalence of diabetes ranged from 6% to 23.7% in the GCC. Three studies showed higher diabetes rates among females [31, 59, 67], while three studies indicated the opposite [29, 45, 56]. Four studies showed almost no difference in the prevalence of diabetes between genders [43, 51, 62, 65]. The prevalence of diabetes rose proportionally with age and reached the highest rates in both sexes among those aged 55–64 years and over [29, 31, 43, 45, 51, 56, 59, 62, 65, 67]. It was also considerably higher among the urban population [29, 62]. Overall, the available data on the prevalence of diabetes in this region indicated that Saudi Arabia, Bahrain, and the UAE have the highest rates of diabetes compared to the other Gulf countries especially Kuwait, where the rates of diabetes were relatively lower; however this might be due to the underestimation of the actual prevalence in one Kuwaiti study as it excluded diabetic subjects on medication [56].
3.2.4. Dyslipidaemia
The prevalence of dyslipidaemia was reported in 7 studies: 3 in Saudi Arabia [27, 31, 37], 1 in Kuwait [53], 2 in Oman [62, 65], and 1 in the UAE [43]. There was no consistent definition of dyslipidaemia within the region. The majority of the dyslipidaemia studies reported the prevalence rate based on total cholesterol and triglycerides levels.
Overall, dyslipidaemia levels were higher in males than females and increased with age gradually up to the age group of 50–59 when it became stable in some studies and slightly declined in others. The prevalence of hypercholesterolemia (HC) ranged from 17% to 54.9% in males and from 9% to 53.2% in females [27, 31, 37, 53, 62, 65]. There was no difference in HC between urban and rural residents [37, 62]. However, one study in Saudi Arabia showed higher rates of hypertriglyceridemia in the urban population (43.2%) than rural population (34.1%) [37]. Based on the available data on dyslipidaemia within the region, HC (≥5.2 mmol/L) was more prevalent in Saudi Arabia. The variation in definitions used in dyslipidaemia studies and the limited data in the GCC make it difficult to accurately compare between countries; however the levels of blood lipids appeared to be high in the Gulf region.
3.2.5. Diet
Six studies carried out in Saudi Arabia [40–42] and UAE [48–50] have determined the eating habits among adult population in these countries.
The dietary patterns presented in these studies are mainly characterized by a high consumption of snacks, fatty food, salty food, and sugar. A study in Saudi Arabia reported that more than half of the study population was consuming a high amount of snacks and fatty and salty foods in daily basis [41]. Similarly, a high consumption of sugar and fast food was reported in the UAE [48, 49]. Further, a low consumption of fruits, vegetable, and cereals was reported in several studies [41, 49, 50]. One study showed a high intake of fruits, vegetables, and dates [42]. The findings from these surveys also demonstrated a high intake of total energy, fats, and protein [41, 48]. A Saudi survey showed a high proportion of total energy derived from fat and carbohydrates (38% versus 39%) and (46.1% versus 46.8%) in both males and females, respectively [41]. Some of the popular unhealthy food habits reported were not having breakfast, consuming less than two meals per day, and a high consumption of fast food meals [41, 49]. A number of studies have examined the association between some food items and CVD risk factors [40, 41, 49]. One study showed an inverse association between consumption of black tea and serum lipids [40], while another study reported a significant association of high intake of energy derived from fatty foods with BMI and hypertension in both genders [41]. Further, low consumption of cereals and fruits was found to be associated with obesity [49].
3.2.6. Smoking
The prevalence of smoking in the Gulf region was addressed in 9 studies: 3 in Saudi Arabia [27, 30, 38], 1 in Bahrain [71], 2 in Kuwait [52, 57], 1 in Oman [61], 1 in Qatar [60], and 1 in the UAE [43].
The rates of cigarette smoking in the GCC ranged from 13.4% to 37.4% in males and from 0.5% to 20.7% in females. Furthermore, the prevalence of smoking fluctuated from age group to age group. It was more common in males at younger ages (18–25 years); however some studies reported a high prevalence in the older age group (40–59 years). In females, the highest rates of smoking were in the older age group (40–49 years) [30, 43, 52, 57, 61, 71]. One study in Saudi Arabia reported higher rates of cigarette smoking in urban than rural subjects [38]. Overall, the prevalence of smoking was higher in Saudi Arabia, Kuwait, the UAE, and Bahrain in comparison to Oman.
3.2.7. Physical Activity
The prevalence of physical activity in the GCC countries was presented in 7 studies: 2 in Saudi Arabia [34, 36], 1 in Bahrain [66], 1 in Kuwait [56], 1 in Oman [64], 1 in Qatar [60], and 1 in the UAE [47].
The prevalence of inactivity was found to be significantly higher among the younger population in the region, and across all age groups physical inactivity was higher in females than males. The rates of inactivity ranged from 24.3% to 93.9% in males and from 50% to 98.1% in females in the GCC [36, 47, 60, 64, 66]. In general, the rates of physical inactivity were considerably high in the GCC region especially Saudi Arabia.
4. Discussion
This review revealed that, in the GCC region, there is a lack of information on the prevalence of CHD with only exception in Saudi Arabia where one national survey reported 5.5% prevalence of CHD [11], which is lower than the prevalence rate reported in Egypt 8.3% [73], while it is higher than in India (3%), China (2%), and Europe (5%) [74, 75]. However, it is important to note that the Saudi report is relatively old and may not reflect the current situation. The rates of ACS and associated risk factors appeared to be very similar in Saudi Arabia (SPACE report) and other Gulf states (Gulf RACE report) except for diabetes, which is more prevalent in Saudi Arabia. However, the SPACE registry results came from phase 1 (pilot study) and thus based on smaller sample size compared to that of Gulf RACE [13, 14].
In contrast to other ACS registries around the world, the prevalence rates of diabetes and current smoking are higher in the Gulf region, while a higher prevalence of hypertension and dyslipidaemia is observed in the Euro heart of the acute coronary syndrome survey and Canadian ACS registry [13, 14, 76, 77]. The rates of diabetes are ranged from 23.3% to 25.1% in the Euro heart survey, Canadian ACS registry, and the Global Registry of Acute Cardiac Events (GRACE) [76, 77], while the prevalence of diabetes is much higher among the ACS patients in the Gulf States especially in Saudi Arabia (56%) [13, 14]. One possible explanation for this high rate of diabetes could be due the high prevalence of obesity and physical inactivity in the GCC region, especially in Saudi Arabia. Furthermore, the mean age of presentation in the SPACE and Gulf RACE cohort is about ten years younger than that reported in the Euro heart survey and the GRACE cohort [13, 14, 78, 79]. This might be due to the high rates of uncontrolled risk factors in the Gulf region as well as the high percentage of younger populations in these countries.
The crude annual incidence of stroke in the Gulf countries was generally lower than the reported incidence in some Arabic countries, for example, Libya (63/100,000) [80] and Northern Palestine (51.4/100,000) [81]. The incidence is even much lower than that which is observed in some of the developed countries such as Scotland (280/100,000) [82] and the East Coast of Australia (206/100,000) [83]. The low rates of strokes in the GCC countries could be explained by the relatively younger age of patients in these countries. Further, the majority of stroke studies in the region had no record on the number of patients who died before reaching hospital, thus underestimating the actual incidence rate.
Several studies in the Gulf States have reported a high incidence of stroke at a younger age. Of the stroke patients, 9.8% to 25% were less than 45 years old [17, 23, 25]. The higher proportion of undiagnosed hypertension and diabetes might be a reason for younger stroke patients. One study in Saudi Arabia showed that only half of the hypertensive stroke patients were actually on medication [17]. Further, lack of awareness about stroke in the Gulf countries might have led to an increase in the incidence of strokes as well as the rates of associated risk factors [84].
When looking at the burden of risk factors among healthy subjects in the GCC region, the prevalence of obesity in adult females is one of the highest amongst females worldwide. This review found that almost half of the females in Kuwait and Bahrain and around 35% of females in Saudi Arabia, the UAE, and Qatar were obese. The overall prevalence of overweight and obesity in the GCC is higher than that which was reported in other Middle Eastern countries such as Lebanon and Turkey [85, 86]. The prevalence was even higher than in many developed countries such as the USA and in developing countries such as India [87, 88]. The food customs in the Gulf region, such as weddings and religious events, might be an important contributory factor for such a high rate of obesity as they serve food that is rich in fat, usually “Kabsa,” which includes meat (from sheep or small camel) with rice. Even socialising with friends and family is usually around eating meals and snacks.
Likewise, more than half of the GCC population are physically inactive, with only a small proportion of people being active on a regular basis. Furthermore, the rate of inactivity appeared to be remarkably higher in Saudi Arabia than in other Gulf countries. The reviewed studies also indicated that males are more likely to be physically active than females, a finding similar to that was reported in Turkey and Pakistan [47]. The unique social, cultural, and environmental factors of the GCC states, such as hot climate, lack of outdoor facilities, the limited number of health clubs, high cost of attending such clubs especially for females, high level of employment of domestic helpers, and the high dependency on automobiles are blamed on the increased levels of physical inactivity in both genders but more noticeably in females. Also, females have more social barriers that make it difficult for them to exercise outside the home without a family member [5, 89].
In the Gulf region, males start smoking cigarettes at an early age (before 18 years), while females generally start after 30s. Cigarette smoking by younger and unmarried females is viewed as culturally unacceptable and can potentially destroy their reputation. However, the case is different when smoking sheesha (water-pipe) as Arabic societies in general accept sheesha smoking by females irrespective of their age and/or social status.
Hypertension and diabetes are the two major risk factors associated with CHD and stroke patients in all studies in the Gulf region; this might be related to the high rates of undiagnosed hypertensive and diabetic patients within the region. In Saudi Arabia, about 70% of the hypertensive people were unaware of their disease [35]. A similar situation was reported in Oman, the UAE, and Bahrain [44, 65, 69]. Likewise, a large number of diabetic subjects in Saudi Arabia (28%) and the UAE (41%) were unaware of their disease [29, 45]. The high rates of uncontrolled diseases such as hypertension and diabetes could be a reason for the relatively young age of CHD and stroke patients in the Gulf region.
The prevalence of dyslipidaemia in general is high in the GCC countries. The available national surveys indicated that half the Saudi population have high level of total cholesterol and almost half of the males and one-third of Saudi females have high level of hypertriglyceridemia [37]. The rates of HC in Saudi Arabia are similar to that reported in USA (53.2%) [90]. Dyslipidaemia is a major risk factor for CHD and plays a central role in the development of atherosclerosis. The high rates of dyslipidaemia in the GCC countries may be due to the high prevalence of physical inactivity, obesity, and diabetes among the Gulf populations. Also, as mentioned before, food customs and the consumption of high fatty foods might be contributing factors.
This review has a number of limitations. First, there was a lack of recent nationally representative reports in the GCC countries, and thus it is difficult to compare the data between GCC countries. Second, there was significant heterogeneity between studies with respect to definitions of the risk factors, design, and population characteristics. Third, only a few studies reported stroke incidence and the majority of them were hospital-based studies with an absence of data on Oman and the UAE. Fourth, there were only a few studies focusing on hypertension, dyslipidaemia, and physical activity. Moreover, the number of included studies relating to the prevalence of risk factors in Qatar and Bahrain were also relatively low. However, the strength of this review was that the literature search was conducted on multiple databases including personal contact of the authors to capture all relevant documents.
5. Conclusion
The present review revealed lower incidence of strokes in the GCC countries than in developed countries and that those affected were younger than in some developing and developed countries. Although there was lack of nationally representative data on the prevalence of CHD in the region, high prevalence of key risk factors was observed. Further, the patterns of risk factors were very similar between the Gulf countries; this may be due to the similarity in culture, religion, cuisine, lifestyle, and environmental factors between these countries. With the rapid urbanization in the Gulf region and the relatively young population, the prevalence of CHD and strokes is expected to increase in the next few decades, which in turn will raise the rate of CVD mortality and morbidity in the region. Well-designed population-based nationally representative surveys focusing on CVD and its associated risk factors are crucial in the Gulf States. Furthermore, there is a need to increase the awareness of the high prevalence of CVD and associated risk factors among the public along with education programs on nutrition and healthier lifestyles including increase in physical activity levels in both men and women. In addition, there is also a need for preventative strategies, especially for type 2 diabetes, to be used in the region and the cooperation in management strategies, especially in obesity and diabetes is also crucial across the region. Moreover, addressing some of the cultural and social barriers that were mentioned previously is also important for reducing the risk of CVD and related risk factors among the GCC population.
Conflict of Interests
The authors declare that they have no competing interests.
Authors’ Contribution
Najlaa Aljefree designed the concept of study and prepared the paper draft. Faruk Ahmed has provided guidance on the study design and critically reviewed the paper. All authors read and approved the final paper.
Acknowledgments
Mrs. Najlaa Aljefree is supported by a scholarship from King Abdul Aziz University for Nutrition and Dietetics. The King Abdul Aziz University had no role in the design, analysis, or writing of this paper.