Atypical Osteomyelitis Caused by Mycobacterium chelonae—A Multimodal Imaging Approach
Abstract
We present an unusual case of a biopsy-proven Mycobacterium chelonae infection (MCI) of skin and soft tissue, which led to osteomyelitis in a 55-year-old Caucasian male. We provide clinical data and discussion about MCI and its diagnostic workup and demonstrate comprehensive imaging findings, including clinical pictures, radiographs, three-phase bone scintigraphy, and combined SPECT/CT findings of this entity, which have not yet been presented in the medical literature.
1. Introduction
Mycobacterium chelonae is an atypical mycobacterium which does not cause tuberculosis or leprosy in humans. They are known for infections of skin, lungs, eyes, and soft tissue. People with immunodeficiency are more likely to contract an infection although a minority of concerned patients were reported to be primary healthy. The identification of the agent is performed by bacterial cultures, polymerase chain reaction (PCR), and DNA sequencing [1].
Bone and joint infections are extremely rare in the context of atypical mycobacterium infections [2].
Osteomyelitis is mostly caused by staphylococcus aureus (75–80%), infrequently also by other bacteria, viruses, and funguses [2, 3].
In the medical literature we found only 2 cases of Mycobacterium chelonae osteomyelitis visualized by multiple diagnostic imaging modalities [2, 4]. To our best knowledge SPECT/CT findings have not yet been published at all.
2. Clinical Presentation
The patient is a 55-year-old Caucasian male with an unclear redness and swelling at the right medial malleolus without any noticed trauma. His medical record includes ulcerative colitis and sarcoidosis treated with prolonged cortisone therapy and liver transplant for treatment of primary sclerosing cholangitis (PSC) 14 years ago.
Tentative diagnosis was gout because of high uric acid in blood testing but common ambulant drug therapy with colchicine and indomethacin did not improve the condition. Spreading of the swelling and redness in combination with increasing inflammation parameters was interpreted as possible phlegmon and treated with penicillin. However no regression was observed and the patient developed additional nodular lesions spreading from the ankle to the anterior medial lower leg. Visible were 12–15 nodular lesions, the newest and proximal lesions were erythematous, and the older ones were darker and violaceous with some scaling (Figure 1).

In the following, punch biopsies were performed, which microscopically showed positive results on gram staining and acid resistance on Ziehl-Neelsen staining, matching with mycobacteria. Bacteria cultures revealed rapidly growing mycobacteria of Runyon group IV.
Additional PCR and sequencing of the amplified DNA detected Mycobacterium chelonae.
In the course of the events several diagnostic imaging modalities were conducted to find out about a possible osseous involvement, which is important for the appropriate selection of antibiotics.
Initially radiographs of the right ankle, tibia, and fibula were obtained, showing moderate circumferential soft tissue swelling around the metatarsophalangeal joint I (MTP I). The ankle mortise was intact with the underlying bony structures appearing normal, beside a healed fracture at the proximal first phalanx (Figure 2).


For further investigation MRI was scheduled but even with sedation refused by the patient due to claustrophobia.
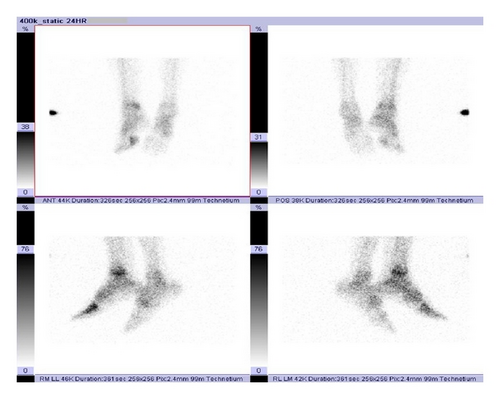
Instead a three-phase bone scan (33 mCi Tc-99 m MDP IV with 24-hour delay) was performed which showed local hyperemia at the right distal lower leg and the MTP I on perfusion phase, surrounding soft tissue tracer uptake on blood pool phase and increased bone remodeling on bone phase, also at the right distal lower leg and the MTP I (Figure 3, bone phase).
Subsequently, using the already given tracer, a combined SPECT/CT was conducted which provides the advantages of better localization and demonstration of morphological changes, compared with scintigraphy.
In the merged pictures we could localize the increased tracer uptake exactly at the distal tibia and the MTP I (Figure 4). The CT data showed evidence of soft tissue and periosteal reaction and osseous disruption at the MTP I (Figure 5).
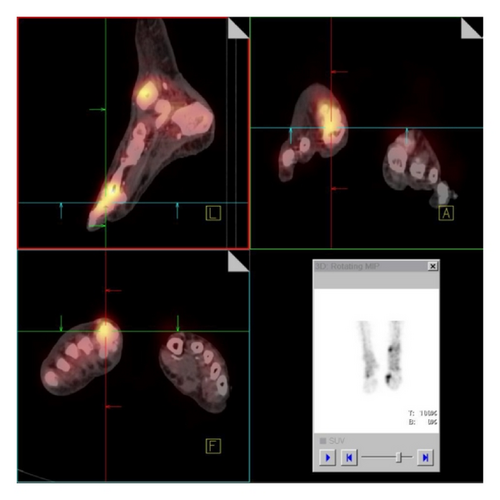
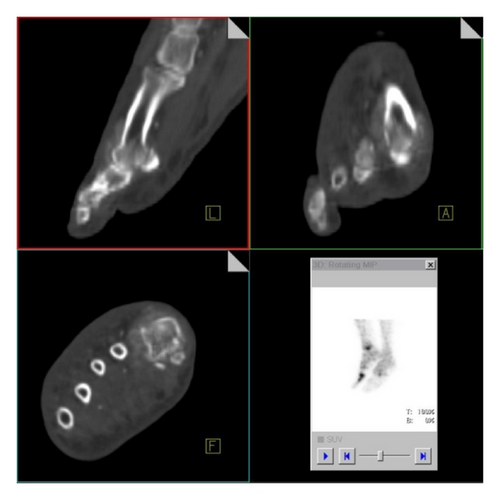
The combination of findings was indicative for a soft tissue infection with additional multifocal osteomyelitis, at the MTP I already with initial osseous destructions.
Antibiotic therapy was adjusted, following antibiogram, to a combination of azithromycin, moxifloxacin, and meropenem under which the patient improved. He could be discharged from our hospital in a good condition 2 weeks later.
3. Discussion
Mycobacteria are a heterogeneous group of aerobic bacteria. There are significant differences in the appropriate treatment so that it is important to distinguish between the agents.
The group can be detected by being gram positive and acid-fast on gram and Ziehl-Neelsen staining. The Runyon classification divides into 4 groups, based on growth rates in bacterial cultures. PCR and DNA sequencing are helpful to detect the agent.
The most familiar mycobacteria are Mycobacterium tuberculosis and Mycobacterium leprae, both listed in Runyon Group III.
Mycobacterium chelonae is a rapidly growing species (Runyon group IV) of mycobacteria other than tuberculosis (MOTT). Those do not respond to first-line antituberculosis drugs.
It is found in natural and processed water sources and known to be responsible for a distinct number of primary infections of the skin, lung, eyes, and soft tissue [2, 5–7].
As an opportunistic pathogen it should be considered when unclear skin and soft tissue infections occur on immunosuppressed patients like patients on corticosteroid therapy, after organ transplantation and with immunodeficiency or autoimmune disorders.
Infections of the bone and joints by nontuberculous mycobacteria, such as Mycobacterium chelonae, are extremely rare and often overlooked with less than a dozen reported cases in the medical literature [2, 8]. However for the selection of antibiotic therapy and for avoidance of chronification, it is of high priority to be aware of possible bone affection.
The disease is often a disseminated cutaneous infection [9, 10], like in our case. If osteomyelitis takes place in this regard, it is usually localized [9, 11] with only one reported case of multifocal osseous involvement [2]. Our findings are indicative for bifocal affection of the distal tibia and the MTP I.
Osteomyelitis by Mycobacterium chelonae has occurred occasionally in the sternum after cardiac operations [12, 13] or in immunocompromised patients [8, 10, 14, 15]; however recent publications reported also occurrence in previously healthy patients [4, 6]. Sternal osteomyelitis is associated with a poor clinical prognosis, perhaps related to late diagnosis and consecutive late onset of specific treatment [12].
To our best knowledge only 2 manuscripts have been published, describing Mycobacterium chelonae osteomyelitis on imaging [2, 4]. So far no literature has been published, describing SPECT/CT imaging findings of osteomyelitis caused by atypical mycobacteria, especially by Mycobacterium chelonae.
All previous reports demonstrated advanced bone changes on imaging, already visible on X-ray. In our case, the initial radiograph was unremarkable for osteomyelitis but we were able to detect the infection with MDP bone scan and get information about localization and morphological changes with a combined SPECT/CT, facilitating appropriate antibiotic therapy.
Conflict of Interests
The authors declare that they have no conflict of interests.