Exercise and Motor Training in People with Parkinson′s Disease: A Systematic Review of Participant Characteristics, Intervention Delivery, Retention Rates, Adherence, and Adverse Events in Clinical Trials
Abstract
There is research evidence that exercise and motor training are beneficial for people with Parkinson′s disease (PD), and clinicians seek to implement optimal programs. This paper summarizes important factors about the nature and reporting of randomized controlled trials of exercise and/or motor training for people with PD which are likely to influence the translation of research into clinical practice. Searches identified 53 relevant trials with 90 interventions conducted for an average duration of 8.3 (SD 4.2) weeks. Most interventions were fully supervised (74%) and conducted at a facility (79%). Retention rates were high with 69% of interventions retaining ≥85% of their participants; however adherence was infrequently reported, and 72% of trials did not report adverse events. Overall, the labor-intensive nature of most interventions tested in these trials and the sparse reporting of adherence and adverse events are likely to pose difficulties for therapists attempting to balance benefits and costs when selecting protocols that translate to sustainable clinical practice for people with PD.
1. Introduction
In recent years there have been an increasing number of randomized controlled trials assessing the effects of exercise and/or motor training in people with Parkinson’s disease (PD). Overall, these trials support exercise and motor training as beneficial in improving walking, balance, muscle strength, and the performance of functional tasks in people with mild-to-moderate PD [1–11]. In order for findings from this research to be of general benefit to people with PD, therapists need to be able to translate the protocols used in the research into clinical practice [12].
Evidence-based practice aims to incorporate and apply high-quality clinical research findings in clinical policy and practice [13, 14]. However, this can be a challenging task as health practitioners may find it difficult to assess, interpret, and implement research evidence [13]. While evidence about beneficial outcomes is paramount in therapists’ decisions to implement a particular intervention, there are other factors that affect how the overall impact of the intervention is interpreted and its potential for widespread clinical application [13–17]. For example, therapists need to consider how the characteristics of participants included in a trial may affect their decision regarding the applicability of the trial intervention with their patients [14]. It is likely that the way in which the intervention was applied in terms of its duration, level of supervision, delivery (i.e., individual versus group), and location (e.g., facilities and equipment required) will influence therapists’ decisions to implement that intervention. A research protocol that has been shown to be effective may not be implemented by therapists if they cannot provide adequate supervision over the required time frame or they do not have access to necessary facilities or equipment. Finally, information regarding retention, adherence, and adverse events is required so that therapists and patients can weigh up the effectiveness of the intervention against its acceptability and any risks associated with implementation [14].
- (1)
disease severity and cognitive status of the included participants,
- (2)
duration, supervision, delivery, and location of the interventions,
- (3)
rates of retention, adherence, and adverse events.
2. Methods
2.1. Data Sources and Searches
Randomized controlled trials of exercise and/or motor training for people with PD were identified via database searches of MEDLINE, EMBASE, AMED, PsycINFO, the Cochrane Central Register of Controlled Trials, and CINAHL. The initial search was conducted in 2009, with a subsequent search conducted over 5 days from the 7th of April, 2011. The electronic search strategy used has been previously reported [2]. The Physiotherapy Evidence Database (PEDro; http://www.pedro.org.au/) was also searched, and the reference lists of previously published systematic reviews [4, 5, 8, 9, 18–30] were checked for any trials not identified with the database search.
2.2. Study Selection
Trials included were published randomized (or quasi randomized, i.e., not truly random but intended to produce similar groups, such as allocation by odd and even birth dates [31]) controlled trials of people with PD where at least one of the interventions was an ongoing program of exercise and/or motor training. All forms of exercise (e.g., aerobic, strength, and treadmill walking) and motor training (e.g., cueing and movement strategy training) were included. Whole-body vibration was not considered to be exercise or motor training. Trials were excluded if the intervention was multidisciplinary or was primarily occupational therapy.
The eligibility of trials was determined in a two-stage process. Firstly, all trial titles and abstracts were screened independently by two investigators (N. E. Allen and G. D. Suriyarachchi). Trials were excluded if it was clear that they did not meet the inclusion criteria. Secondly, the full article was obtained for the remaining trials and each trial was assessed independently by at least two investigators (N. E. Allen, C. G. Canning or J. Song), using a standardized form containing the details of the inclusion criteria. Care was taken to identify trials that had been reported in more than one journal article. Where this occurred, the multiple articles were counted as one trial and all articles were used to collect data for that trial.
2.3. Data Extraction
A data collection form was developed, tested on five randomly selected trials and then modified accordingly. All investigators were involved in data extraction, and all data was double-checked by an investigator not involved in its initial extraction (N. E. Allen or J. Song). Discrepancies were resolved by discussion.
Information extracted from each trial included a description of participants (including cognitive status), details of the exercise and motor training program and how it was administered, as well as details regarding retention rates, adherence to the intervention, and monitoring and reporting of adverse events. Retention was defined as the number of participants who completed the trial (i.e., undertook the first or only post-intervention assessment excluding further follow-up assessments) expressed as a percentage of the number of participants who began the trial. Adherence was defined as the number of intervention sessions attended by participants expressed as a percentage of the number of intervention sessions prescribed [15].
3. Results
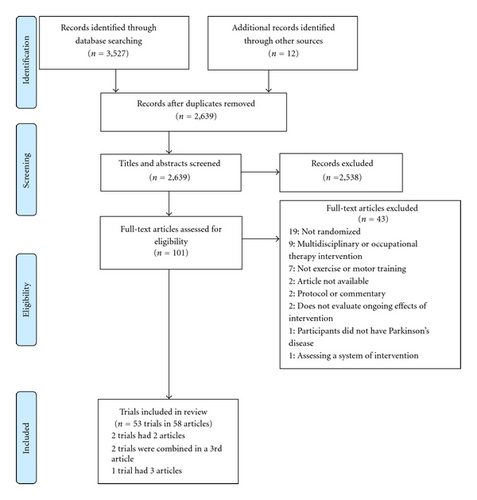
Searching identified 3,539 records, of which 53 trials involving 1,940 participants were found to be eligible for inclusion in the paper (Figure 1) [32]. There were no disagreements between reviewers regarding the inclusion of any articles. The characteristics of the included trials [1, 3, 6, 7, 10, 11, 33–85] are summarised in Table 1.
| First author, year and intervention type | Initial group sizes | Disease severity | Location and delivery of experimental intervention | Duration of intervention (weeks) | Hours of intervention (approx) | Supervision (%) | Retention (%) | Any dropouts related to intervention? | Adherence (%) | Adverse events occurred |
|---|---|---|---|---|---|---|---|---|---|---|
| Allen 2010, | Mild to | Facility, group | ||||||||
| exercise OR | 24 | moderate | + home individual | 26 | 65 | 10% | 87.5% | Y | 70% | N |
| control | 24 | 100% | ||||||||
| Ashburn 2007, | Moderate | Home, | ||||||||
| exercise and | 70 | individual | 6 | 33 | 18% | 96% | Y | U (99% of Supervised exercise) | N | |
| strategy OR | ||||||||||
| control | 72 | 92% | ||||||||
|
Mild | Facility, | NA | NR | NRM | |||||
| 4 | delivery | 16 | 32 | 100% | 100% | |||||
| unclear | ||||||||||
| control | 4 | 100% | ||||||||
| Blackinton 2002, | U | Mild to | Facility, | U | NR | NRM | ||||
| exercise OR | 15 | moderate | group + home | 6 | 15 | 66% | 53% | Y | ||
| control | total | individual | total | |||||||
| Bloomer 2008, | Mild | Facility, | ||||||||
| resistance | 8 | delivery | 8 | 8 | 100% | 75% | N | U | N | |
| training OR | unclear | |||||||||
| control | 8 | 88% | ||||||||
| Braun 2011, | Mild to | Facility, | U | NRM | ||||||
| physiotherapy | moderately | individual or | 6 + home | |||||||
| + mental | 25 | severe | group + home, | 6 | mental | U (100%)‡ | 88% | Y | (87%)†‡ | |
| practice OR | individual | practice | ||||||||
| physiotherapy + relaxation | 22 | 6 | 6 + home relaxation | U (100%)‡ | 82% | (88%)†‡ | ||||
| Bridgewater | Mild to | Facility, group | NA | NRM | ||||||
| 1996 (also as [38]), | moderate | |||||||||
| aerobic and | 13 | 12 | 16 to 22 | 100% | 100% | 95% | ||||
|
||||||||||
| education | 13 | 12 | 4 | 100% | U | |||||
| Burini 2006*, | Mild to | Facility, group | NRM | |||||||
| aerobic | 13 | moderate | 7 | 17 | 100% | 85% | Y | 87% | ||
| exercise OR | ||||||||||
| Qigong | 13 | 7 | 17 | 100% | 85% | Y | 88% | |||
| Caglar 2005, | Mild to | Facility, group | NA | NRM | ||||||
| exercise OR | 15 | moderate | + home, | 9 | 63 | 4% | 100% | 100% | ||
| control | 15 | individual | ||||||||
| Cakit 2007, | Mild to | Facility, | NR | Partial— | ||||||
| treadmill | 27 | moderate | delivery | 8 | 8 | 100% | 78% | U | 2 minor | |
| walking OR | unclear | cardiac | ||||||||
| control | 27 | 37% | ||||||||
| Comella | U | Mild to | Facility, | U | NRM | |||||
| 1994*, | 18 | moderate | delivery | 89% total | ||||||
| physiotherapy | total | unclear | 4 | 12 | 100% | U | U | |||
| OR | ||||||||||
| control | ||||||||||
| de Bruin 2010, | Mild to | Home, | ||||||||
| walk with | 16 | moderate | individual | 13 | 19.5 | 0% | 69% | Y | 100%† | Y—1 |
| music OR | thigh | |||||||||
| control | 17 | 65% | cramping | |||||||
|
||||||||||
| Dereli 2010, | Mild to | NRM | ||||||||
| supervised | 16 | moderate | Facility, | 10 | 22.5 | 100% | 94% | Y | 100%† | |
|
individual; | |||||||||
| 16 | home, individual | 10 | 22.5 | 4% | 94% | NR | ||||
| Dias 2005, | Mild to | Facility, | NA | NRM | ||||||
| physiotherapy | 8 | moderate | delivery | 4 to 10 | 20 | 100% | 100% | 100% | ||
| + cues OR | unclear | |||||||||
| physiotherapy | 8 | 4 to 10 | 20 | 100% | 100% | 100% | ||||
| Ebersbach 2010, | Mild to moderate | NR | NRM | |||||||
| LSVT BIG | 20 | Facility, individual; | 4 | 16 + home X | U (100%)‡ | 100% | NA | |||
| OR Nordic walking | 20 | facility, group; | 8 | 16 + home X | U (100%)‡ | 95% | U | |||
| OR home exercise | 20 | home, individual | 4 | U | U | 95% | N | |||
| + all did home, individual | ||||||||||
| Ellis 2005* | Mild to | Facility, group | NRM | |||||||
| (also as [44]), | moderate | |||||||||
| physiotherapy | 35 | 6 | 18 | 100% | 91% | N | 93% | |||
| OR | ||||||||||
| control | 33 | 94% | N | |||||||
| Fisher 2008, | Mild | Facility, | NA | NR | N | |||||
| treadmill | 10 | delivery | 8 | 18 | 100% | 100% | ||||
| walking OR | unclear | |||||||||
| physiotherapy | 10 | 8 | 18 | 100% | 100% | |||||
| OR | ||||||||||
| control | 10 | 100% | ||||||||
| Frazzitta 2009, | Moderate | Facility, | NA | NR | NRM | |||||
| Treadmill | 20 | individual | 4 | 9.5 | 100% | 100% | ||||
| walking with | ||||||||||
| cues OR | ||||||||||
| physiotherapy | 20 | 4 | 9.5 | 100% | 100% | |||||
| with cues | ||||||||||
| Guo 2009, | Mild to | Facility, group | NR | NR | NRM | |||||
| physiotherapy | 23 | moderate | education and individual | 8 | 12 of therapy | 100% | 91% | |||
| and education | therapy | |||||||||
| OR | ||||||||||
| control | 21 | 90% | ||||||||
| Hackney 2007, | Mild to | Facility, | NA | NRM | ||||||
| Tango OR | 9 | Moderate | group | 13 | 20 | 100% | 100% | 100% | ||
| exercise | 10 | 13 | 20 | 100% | 100% | 100% | ||||
| Hackney 2008 | Mild to | Facility, | NRM | |||||||
| (also as [54]), | moderate | group implied | ||||||||
| Tai Chi OR | 17 | 10 to 13 | 20 | 100% | 76% | Y | 100%† | |||
| control | 16 | 81% | ||||||||
| Hackney 2009 | Mild to | Facility, | Partial— | |||||||
| (also as [54]), | moderate | group | 1 knee | |||||||
| Waltz/foxtrot | 19 | 10 to 13 | 20 | 100% | 89% | Y | 100%† | pain | ||
| OR | ||||||||||
| tango OR | 19 | 10 to13 | 20 | 100% | 74% | Y | 100%† | |||
| control | 20 | 85% | ||||||||
| Hackney 2010, | Mild to | Facility, group | NRM | |||||||
| partnered | 19 | moderate | 10 | 20 | 100% | 79% | Y | 100%† | ||
| tango OR | ||||||||||
| nonpartnered | 20 | 10 | 20 | 100% | 80% | Y | 100%† | |||
| tango | ||||||||||
| Hass 2007, | Mild to | Facility, | NA | NR | Y—1 | |||||
| resistance | 10 | moderate | delivery | 12 | 12 | 100% | 100% | muscle | ||
| training + | unclear | soreness | ||||||||
| supplement | and 1 | |||||||||
| OR | Shoulder | |||||||||
| resistance | 10 | 12 | 12 | 100% | 100% | pain | ||||
| training + | ||||||||||
| placebo | ||||||||||
| Hirsch 2003, | Mild to | Facility, | ||||||||
| balance and | 9 | moderate | delivery | 10 | 22.5 | 100% | 67% | Y | 89%† | Y—1 |
| resistance | unclear | inguinal | ||||||||
| training OR | hernia | |||||||||
| balance | 9 | 10 | 15 | 100% | 100% | 92% | ||||
| training | ||||||||||
| Keus 2007, | Mild to | Facility, | NA | |||||||
| physiotherapy | 14 | moderately | individual | 10 | 11 to 15 | 100% | 100% | 63% | N | |
| OR control | 13 | severe | 92% | |||||||
| Kurtais 2008, | Mild to | Facility, | NR | NRM | ||||||
| treadmill | 13 | moderate | delivery | 6 | 12 + | U (100%)‡ | 92% | Y | ||
| walking OR | unclear + | home X | ||||||||
| home, | ||||||||||
| control | 14 | individual | 86% | |||||||
| Lehman 2005a, | Mild | Facility implied, | NA | NR | NRM | |||||
| walk with | 5 | delivery unclear | 2 | 5 | 100% | 100% | ||||
|
6 | 100% | ||||||||
| Mak 2008, | Mild to | Facility | NR | NRM | ||||||
| cued sit to | 21 | moderate | Implied, | 4 | 4 | 100% | 90% | U | ||
| stand OR | delivery | |||||||||
| OR exercise | 21 | unclear | 4 | 6 | 100% | 90% | U | |||
| control | 18 | 78% | ||||||||
| Marchese | U | Mild to | Facility, | U | NR | NR | NRM | |||
| 2000, | 20 | moderate | individual + | |||||||
| physiotherapy | total | home, | 6 | 18 + | U (100%)‡ | |||||
| OR | individual | home X | ||||||||
| physiotherapy | 6 | 18 + | U (100%)‡ | |||||||
| with cues | home X | |||||||||
| Miyai 2000*, | Mild to | Facility, | NA | NR | NRM | |||||
| treadmill | 5 | moderate | individual | 4 | 6 | 100% | 100% | |||
| walking OR | ||||||||||
| physiotherapy | 5 | 4 | 6 | 100% | 100% | |||||
| Miyai 2002, | Mild to | Facility, | NR | NRM | ||||||
| treadmill | 12 | moderate | individual | 4 | 6 | 100% | 92% | N | ||
| walking OR | ||||||||||
| physiotherapy | 12 | 4 | 6 | 100% | 75% | N | ||||
| Morris 2009, | Mild to | Facility, | NA | NRM | ||||||
| movement | 14 | moderate | individual | 2 | Up to 12 | 100% | 100% | 88% of | ||
| strategies OR | maximum | |||||||||
| sessions | ||||||||||
| exercises | 14 | 2 | Up to 12 | 100% | 100% | 81% of | ||||
| maximum | ||||||||||
| sessions | ||||||||||
| Müller 1997, | Mild to | Location and | NR | NR | NRM | |||||
| behavioural | 15 | moderate | delivery | 10 | 30 | 100% | U | |||
| therapy OR | unclear | |||||||||
| nonspecific | 14 | 10 | 30 | 100% | U | |||||
| exercises and information | ||||||||||
| Mild to moderate |
|
|
||||||||
| cueing | 76 | 3 | 4.5 | 100% | 99% | N | 100% | |||
| training OR | ||||||||||
| control | 77 | 100% | ||||||||
| Pacchetti | Mild to | Facility, group | U | NR | NR | NRM | ||||
| 2000, | moderate | |||||||||
| physiotherapy | 16 | 13 | 19.5 | 100% | ||||||
| OR | ||||||||||
| music therapy | 16 | 13 | 26 | 100% | ||||||
| Palmer 1986, | Mild to | Facility, group | NA | NR | NRM | |||||
| exercise OR | 7 | moderately | 12 | 36 | 100% | 100% | ||||
| seated karate | 7 | severe | 12 | 36 | 100% | 100% | ||||
| Pelosin 2010, | Mild to | Facility, | NA | NR | NRM | |||||
| physiotherapy | 9 | moderate | delivery | 4 | 12 | 100% | 100% | |||
| with FOG | unclear | |||||||||
| strategies OR | ||||||||||
| physiotherapy | 9 | 4 | 12 | 100% | 100% | |||||
| Protas 2005, | Mild to | Facility, | NA | NRM | ||||||
| treadmill | 9 | moderate | individual | 8 | 24 | 100% | 100% | 100% | ||
| walking | ||||||||||
| and step | ||||||||||
| training OR | ||||||||||
| control | 9 | 100% | ||||||||
| Qutubuddin | Mild to | Facility, | NRM | |||||||
| 2007, | moderate | delivery | ||||||||
| computerized | 12 | unclear + | 8 | 18 | 20% | 75% | U | U | ||
| dynamic | home, | |||||||||
| posturography | individual | |||||||||
| OR | ||||||||||
| physiotherapy | 10 | 8 | 18 | 20% | 60% | U | U | |||
| Ridgel 2009, | Mild to | Facility, | NA | NR | NRM | |||||
| forced cycling | 5 | moderate | delivery | 8 | 24 | 100% | 100% | |||
| OR | unclear | |||||||||
| self-paced | 5 | 8 | 24 | 100% | 100% | |||||
| cycling | ||||||||||
| Sage 2009, | Mild to | Facility, | NRM | |||||||
| aerobic | 17 | moderate | group | 10 to 12 | 18 | 100% | 76% | Y | 86.8%† | |
| exercise OR | ||||||||||
| SAFEx OR | 21 | 10 to 12 | 20 to 34 | 100% | 86% | Y | 92.9%† | |||
| control | 15 | 100% | ||||||||
| Sage 2010, | Mild to | Facility, | NA | NRM | ||||||
| SAFEx OR | 15 | moderate | group | 12 | 36 | 100% | 100% | 100% | ||
| non-SAFEx | 14 | 12 | 36 | 100% | 100% | 100% | ||||
| Schenkman | Mild to | Location | ||||||||
| 1998, | moderate | unclear, | ||||||||
| exercise OR | 27 | individual | 10 to 13 | 22.5 to 30 | 100% | 85% | U | 100%† | N | |
| control | 24 | 96% | ||||||||
| Schmitz- | Mild to | Facility group | NR | NRM | ||||||
| Hübsch 2006, | moderately | + home | ||||||||
| Qigong OR | 32 | severe | individual | 24 | 16 + home X | 66% | 91% | Y | ||
| control | 24 | 87.5% | ||||||||
| Smania 2010, | Moderate | Facility, | NR | NRM | ||||||
| balance | 33 | to | individual | 7 | 17.5 | 100% | 85% | Y | ||
| training OR | moderately | |||||||||
| general | 31 | severe | 7 | 17.5 | 100% | 87% | Y | |||
| exercises | ||||||||||
| Stallibrass | Mild to | Facility, | NRM | |||||||
| 2002, | moderate | individual | ||||||||
| Alexander | 32 | 12 | 16 | 100% | 91% | Y | 99%† | |||
| technique | ||||||||||
| OR | ||||||||||
| massage OR | 31 | 12 | 16 | 93% | 97%† | |||||
| control | 30 | 100% | ||||||||
| Tamir 2007, | Mild to | Facility, | NR | Partial— | ||||||
| exercise + imagery | 12 | moderate | delivery | 12 | 24 + | U (100%)‡ | 92% | U | 2 cardiac | |
| OR | unclear + | home X | problems | |||||||
| exercise | 11 | home, individual | 12 | 24 + home X | U (100%)‡ | 91% | U | |||
| Thaut 1996, | Mild to | Home, | NA | |||||||
| walk with | 15 | moderate | individual | 3 | 10.5 | 14% | 100% | 100% | Y—1 fall | |
| auditory cues | ||||||||||
| OR | ||||||||||
| walk without | 11 | 3 | 10.5 | 14% | 100% | 100% | ||||
| cues OR | ||||||||||
| control | 11 | 100% | ||||||||
| Toole 2000, | Mild to | Facility, | NR | NRM | ||||||
| exercise OR | 6 | moderately | delivery | 10 | 30 | 100% | 67% | N | ||
| control | 5 | severe | unclear | 60% | ||||||
| Toole 2005, | U | Mild to | Facility, | NR | NR | 99% | NRM | |||
| treadmill | 23 | moderately | delivery | 6 | 6 | 100% | overall | |||
| walking with | total | severe | unclear | |||||||
| body weight | ||||||||||
| support OR | ||||||||||
| treadmill | 6 | 6 | 100% | |||||||
| walking with | ||||||||||
| weights OR | ||||||||||
| treadmill | 6 | 6 | 100% | |||||||
| walking | ||||||||||
| Yang 2010, | Mild to | Facility, | ||||||||
| downhill | 16 | moderate | delivery | 4 | 6 | 100% | 94% | Y | 100%† | N |
| treadmill | unclear | |||||||||
| walking OR | ||||||||||
| conventional | 17 | 4 | 6 | 100% | 88% | Y | 100%† | N | ||
| therapy | ||||||||||
| Yousefi 2009, | Mild to | Facility, | NA | NR | NRM | |||||
| exercise OR | 12 | moderate | group | 10 | 40 | 100% | 100% | |||
| education | 12 | 10 | 40 | 100% | ||||||
- Supervision: the number of intervention sessions supervised expressed as a percentage of the number of sessions prescribed; retention: the number of participants who completed the trial (i.e., undertook a post-intervention assessment but excluding follow-up) expressed as a percentage of the number of participants who began the trial; adherence: the number of intervention sessions participants attended expressed as a percentage of the number of intervention sessions prescribed; Y: yes; N: no; NA: not applicable; U: unclear—insufficient information to categorize; NR: not reported; NRM: not reported to be monitored; X: exercise; FOG: freezing of gait; SAFEx: sensory attention focused exercise; *cross-over trial; †data only for participants who completed the trial; ‡data only for the facility component of the intervention;apart 2 of trial only.
3.1. Participant Characteristics
Forty (75%) of the reviewed trials included participants with mild-to-moderate PD (i.e., equivalent to Hoehn and Yahr stage I to III [86]). Seven trials (13%) included participants with mild-to-moderately severe PD (i.e., Hoehn and Yahr stage I to IV), while four trials (8%) included only participants with mild PD and two trials (4%) included only participants with moderate PD (Table 1). Most trials stipulated the cognitive status of included participants. Twenty-nine trials (55%) used the Mini-Mental State Examination [87] to screen potential participants’ cognitive abilities, with the minimum score for inclusion varying between 20 and 28 out of the maximum of 30 [1, 3, 6, 7, 10, 11, 34, 36, 39, 41–43, 45, 47–50, 56, 58, 60, 63–65, 69, 71, 76–78, 80, 85]. One trial (2%) [70] specified that participants required at least moderate scores on the Neurobehavioural Cognitive Status Examination [88]. Thirteen trials (25%) made a statement to the effect that included participants had no dementia and/or reasonable cognition [35, 46, 51, 52, 57, 59, 62, 66, 67, 79, 81, 83, 84]. Ten trials (19%) did not give a clear indication of the participants’ cognitive abilities [33, 37, 40, 53, 55, 68, 72, 74, 75, 82].
3.2. Exercise and/or Motor Training Program Characteristics
In the 53 trials, there were 90 intervention groups that involved exercise and/or motor training (including two intervention groups for the cross-over trials where one intervention was a control [11, 42, 47]) (Table 1). Average intervention duration was 8.3 weeks (SD = 4.2, range = 2 to 26 weeks), with 37 trials (70%) conducting an intervention of 10 weeks or less. The total number of hours of intervention was not clearly reported in all studies (see Table 1); however, from the available data, an average of approximately 20 hours (SD approximately 11, range = 4 to 65 hours) appears broadly representative of the included trials. Sixty-seven of the 90 intervention groups (74%) involved full supervision of exercise and/or motor training. Participants in 18 (27%) of the fully supervised intervention groups received one-on-one supervision and 20 (30%) received supervision in small groups but the intervention delivery (one-on-one or small group supervision) was unclear in the remaining 29 (43%) intervention groups. Participants in most intervention groups (71; 79%) were required to attend a facility for all or the majority of the intervention sessions.
3.3. Retention, Adherence, and Adverse Events
Retention was generally well reported and was high, with 62 (69%) of the 90 intervention groups retaining at least 85% of participants (Table 1). Seventeen (32%) of the 53 included trials reported that at least one participant dropped out for a reason related to the intervention (Table 2). Difficulties with transport and disinterest/poor adherence were the most common intervention-related reasons for dropouts.
| First author and year | Dropout reason | Number of participants |
|---|---|---|
| Allen 2010 | Did not want to do the intervention | 1 |
| Ashburn 2007 | Falls (but not during intervention) | 1 |
| Blackinton 2002 | Safety concerns | 1 |
| Braun 2011 | Imagery too confronting | 1 |
| Burini 2006 | Poor adherence to exercise; | 2 |
| back pain | 1 | |
| de Bruin 2010 | No access to necessary equipment | 1 |
| Dereli 2010 | Did not want to do the intervention | 1 |
| Hackney 2008 (also as [54]) | Exercise not intense enough; | 1 |
| transport problems | 2 | |
| Hackney 2009 (also as [54]) | Knee pain; | 1 |
| transport problems | 2 | |
| Hackney 2010 | Travel distance; | 2 |
| classes too fatiguing; | 1 | |
| lack of interest | 1 | |
| Hirsch 2003 | Inguinal hernia | 1 |
| Kurtais 2008 | Poor adherence to exercise | 1 |
| Sage 2009 | Time commitment | 4 |
| Schmitz-Hubsch 2006 | Uncomfortable in the group; | 1 |
| uncomfortable with Qigong | 1 | |
| Smania 2010 | Uncooperative | 4 |
| Stallibrass 2002 | Could not travel | 1 |
| Yang 2010 | Low motivation; | 1 |
| transport problems | 1 |
Overall, adherence and adverse events were infrequently reported in the included trials (Table 1). Adherence was reported in some form in 26 (49%) of the included trials. However, 11 (42%) of these trials only reported adherence for those participants who completed the intervention. Most trials (38; 72%) did not report monitoring for adverse events. Across the remaining 15 trials, 11 adverse events occurred (Table 1). Four participants from two separate trials [41, 80] experienced cardiac problems. Two of these participants, one from each group in a trial comparing physical therapy with and without mental practice [80], withdrew from the study. The two participants from the other trial [41] were able to continue safely with treadmill training. Other adverse events reported included a fall [81] and muscle cramps and tiredness [43] in trials involving cued overground walking, knee pain during a dancing program [52], muscle soreness and shoulder pain [56] following resistance training, and a hernia [57] subsequent to muscle strength assessment.
4. Discussion
A substantial number of randomized controlled trials of exercise and/or motor training for people with PD have been published. However, the nature and reporting of these trials are likely to provide challenges for therapists aiming to implement the interventions into clinical practice [17]. Most trials involved only cognitively intact participants with mild-to-moderate PD. Trials tended to be of short duration, highly supervised, and conducted at a facility. Furthermore, the reports for many trials were lacking important details, with adherence and adverse events particularly being inadequately reported.
On the whole, trials included in this paper included only participants with mild-to-moderate PD who were without significant cognitive impairment. Including only these types of participants not only makes it easier to conduct trials of exercise and motor training interventions but also aids interpretation of the results. However, cognitive impairment is now recognised as a common problem in PD, with over 80% of people with PD ultimately developing dementia [89]. Further work is needed to determine the effectiveness of exercise and motor training in people with more severe cognitive impairment and/or more advanced disease.
Most of the reviewed trials were of short duration, highly supervised, and facility based (Table 1). Interventions lasted an average of around two months. Seventy-four percent of the intervention groups were fully supervised, with no reported expectation for participants to undertake unsupervised exercise. Furthermore, 79% of intervention groups were mainly conducted at a facility such as a hospital or university. Such brief, highly supervised interventions conducted in controlled environments are likely to improve the adherence of participants to exercise and motor training programs and to ensure that interventions are being performed optimally. In this regard, these trials are useful and important for determining the short-term efficacy of an intervention. However, given that PD is a long-term, neurodegenerative condition, the capacity of therapists and patients to sustain the intervention over the long term needs to be considered. Furthermore, such brief and highly supervised interventions are costly and less likely to give information about the effectiveness of the intervention when implemented into usual practice [13, 17]. For example, the requirement for participants to travel to a facility was a common reason for withdrawal from the included trials (Table 2). Moreover, the neurodegenerative nature of PD and the limited resources available to healthcare systems mean that such labor-intensive programs are unlikely to be sustained or afforded by most health-care providers. Additionally, as PD is a progressive disease it is important that people with PD are empowered to self-manage their disease to some extent [90, 91]. To this end, trials of more pragmatic and sustainable exercise and motor training interventions, with the potential for direct translation into clinical practice and including cost-effectiveness analysis, are needed.
The likely adherence to an exercise and motor training program is an important factor to consider when prescribing such a program for an individual with PD. Adherence to the intervention was reported in less than half of the included trials, and some reports of adherence are artificially elevated by including only those participants who completed the trial (Table 1). Some trials were able to effectively maximise adherence by providing a flexible timeframe for participants to complete the intervention [46, 51, 52, 74, 76] and so allow participants more options in fitting their exercise and/or motor training program around their daily lives. This pragmatic approach is likely to more closely reflect therapy attendance patterns and is therefore likely to be helpful for therapists considering translating the research into their clinical practice.
Given the importance of adherence to exercise and motor training programs, strategies to promote adherence in people with PD need to be considered. Providing a high level of supervision seems likely to promote adherence in the short term, as it may enhance participants’ commitment to the program. However, a Cochrane review comparing home and centre-based exercise programs for older adults found that, in the long term, participants were more likely to adhere to home-based programs [92]. Furthermore, the reviewers noted a trend toward more sustained improvements in the home-based than in the centre-based programs and suggested that this was attributable to the higher adherence in home-based programs. In the present paper, three of the included trials report high levels of adherence with minimally supervised home-based programs [40, 43, 81]. Common to all three of these trials was a requirement for participants to keep a daily record of what exercise/motor training they had performed. It seems likely that this simple strategy assisted in promoting adherence in these trials. Other strategies with the potential to improve adherence in sustainable, minimally supervised trials, such as participant involvement in goal setting [93, 94], flexibility to allow programs to be modified for individuals [1, 91, 93, 94], and intermittent followup [91, 94], warrant exploration.
The issue of adverse events was inadequately addressed in the trials included in this paper, with only 15 trials reporting monitoring for adverse events. In these 15 trials, 11 adverse events were reported, most of which were minor in nature (Table 1). However, when discussing and planning exercise and motor training options with people with PD, therapists need to be informed not only about the effectiveness of a given intervention but also about the nature and likelihood of any potential adverse events [95]. Similarly poor reporting of adverse events was found in a recent Cochrane review of progressive resistance training for older adults [95]. Notably, the Cochrane review found that adverse events were more likely to be detected in trials that used a clear definition of adverse events than in trials which did not use a definition. In the same way, the use of a definition for adverse events is likely to improve the assessment and reporting of adverse events in trials of exercise and motor training for people with PD.
This paper has examined several factors in the nature and reporting of trials of exercise and/or motor training which are likely to influence the way research is applied by therapists in clinical practice. However, this paper did not address whether or not trial protocols were reported in sufficient detail to allow therapists to emulate the research intervention in the clinic. This detailed reporting of trial interventions is critical in enabling research to be clinically applied [96]. The ability of many journals to provide online material which supplements the published article will aid the provision of such details despite the necessary word count limitations placed on authors.
5. Conclusions
Clinicians seeking to use research to inform their clinical practice rely heavily on the design and reporting of randomized controlled trials to reach their decisions. However, the nature and reporting of trials of exercise and/or motor training for people with PD are likely to provide challenges for therapists aiming to implement the interventions into clinical practice. The short duration, highly supervised and facility-based nature of many of the interventions, coupled with the tendency to include only cognitively-intact participants with mild-to-moderate disease, mean that findings may not generalise when therapists set out to apply them in the long-term management of people with PD. Infrequent reporting of adherence and adverse events compounds this problem and makes cost-benefit balancing more difficult. It is recommended that these issues be taken into account in the design and reporting of future trials.




