Economic burden of gastrointestinal cancer under the protection of the New Rural Cooperative Medical Scheme in a region of rural China with high incidence of oesophageal cancer: cross-sectional survey
Abstract
enObjective
To evaluate the financial burden of oesophageal cancer under the protection of the new Rural Cooperative Medical Scheme (NCMS) and to provide evidence and suggestions to policymakers in a high-incidence region in China.
Methods
We analysed inpatient claim data for oesophageal cancer, gastric cancer and colorectal cancer from 1 January to 31 December 2013. The data were extracted from the NCMS management system of Hua County, Henan Province, a typical high-risk region for oesophageal cancer in China. Cancer-specific health economic indicators were calculated to evaluate the financial burden under the protection of the local NCMS.
Results
The total cost of oesophageal cancer was 2.7–3.6 times higher than that of gastric cancer and colorectal cancer, respectively, due to high incidence of oesophageal cancer. For each hospitalisation to treat oesophageal cancer, the average total cost and out-of-pocket expenses after reimbursement equalled an entire year's gross domestic product per capita and per capita disposable income, respectively, for the local area. The average total cost per hospitalisation for oesophageal cancer increased monotonically with hospital level for surgical hospitalisations, and it increased more rapidly for non-surgical hospitalisations (from $301 to $2589, 860%) than for gastric cancer (from $289 to $1453, 503%) and colorectal cancer (from $359 to $1610, 448%). Vulnerable groups with less access to high-level hospitals were found in different gender and age groups.
Conclusions
Oesophageal cancer imposes serious financial burdens on communities and patients' households in this high-incidence region, and no preferential policy from the local NCMS has been designed to address this issue. A special supportive policy should be developed on the basis of local disease profiles and population characteristics to alleviate the financial burden of populations at high risk for certain high-cost diseases.
Abstract
frObjectif
Evaluer la charge financière du cancer de l’œsophage sous la couverture du Nouveau Schéma Médical Cooperatif Rural (NSMCR) et fournir des données et des suggestions aux décideurs dans une région à incidence élevée en Chine.
Méthodes
Nous avons analysé les données de malades pour le cancer de l'oesophage, gastrique et colorectal du 1er janvier au 31 décembre 2013. Les données ont été extraites du système de gestion du NSMCR du comté de Hua, dans la province du Henan, une région à risque élevé, typique pour le cancer de l’œsophage en Chine. Les indicateurs économiques de la santé, spécifiques du cancer ont été calculés pour évaluer la charge financière sous la couverture du NSMCR local.
Résultats
Le coût total du cancer de l’œsophage était 2,7 à 3,6 fois plus élevé que celui du cancer gastrique et du cancer cancer colorectal, respectivement, en raison de l'incidence élevée du cancer de l’œsophage. Pour chaque hospitalisation pour le cancer de l’œsophage, le coût total moyen et les dépenses directes payées de la poche après remboursement équivalaient au PIB d'une année entière par habitant et au revenu disponible par habitant, respectivement, pour la région. Le coût total moyen par hospitalisation pour le cancer de l’œsophage augmentait de façon monotone avec le niveau de l'hôpital pour les hospitalisations chirurgicales et augmentait plus rapidement pour les hospitalisations non chirurgicales (de 301 $ à 2589 $, 860%) par rapport au cancer gastrique (de 289 $ à 1453 $, 503%) et au cancer colorectal (de 359 $ à 1610 $, 448%). Les groupes vulnérables avec moins d'accès aux hôpitaux de haut niveau ont été trouvés dans différents groupes d’âge et de sexe.
Conclusions
Le cancer de l'oesophage impose des charges financières importantes sur les communautés et les ménages des patients dans cette région à haute incidence, et aucune politique préférentielle du NSMCR local n'a été conçue pour répondre à cette question. Une politique de soutien spécial devrait être mise au point sur la base des profils des maladies locales et des caractéristiques de la population pour alléger la charge financière des populations à risque élevé pour certaines maladies coûteuses.
Abstract
esObjetivo
Evaluar la carga financiera del cáncer de esófago bajo la protección del nuevo Sistema Médico Cooperativo Rural (SMCR) y proveer evidencia y sugerencias a los políticos en una región de alta incidencia en China.
Métodos
Hemos analizado datos de solicitudes de reembolso de pacientes ingresados por cáncer de esófago, cáncer gástrico y cáncer color rectal entre el 1 de Enero y el 31 de Diciembre del 2013. Los datos se extrajeron sistema de gestión del SMCR en el Condado de Hua, Provincia de Henan, una región típica de alto riesgo para cáncer de esófago en China. Se calcularon los indicadores sanitarios económicos específicos para cáncer con el fin de evaluar la carga financiera bajo la protección SMCR local.
Resultados
Los costes totales de cáncer de esófago eran 2.7 y 3.6 veces más altos que los de cáncer gástrico o cáncer colorrectal, respectivamente, debido a la alta incidencia de cáncer de esófago. En cada hospitalización para tratar el cáncer de esófago, el coste promedio y los gastos de bolsillo después del pago de la devolución eran equivalentes a un año del producto doméstico bruto per cápita, y per cápita como ingreso disponible, respectivamente, para el área local. El coste promedio por hospitalización para el cáncer de esófago aumentó uniformemente según el nivel del hospital por hospitalizaciones quirúrgicas, y aumentó más rápidamente para hospitalizaciones no quirúrgicas (de $301 a $2589, 860%) que el cáncer gástrico (de $289 a $1453, 503%) y cáncer colorrectal (de $359 a $1610, 448%). Los grupos vulnerables con menor acceso a hospitales de alto nivel pertenecían a diferente género y grupo de edad.
Conclusiones
El cáncer de esófago impone una importante carga financiera sobre las comunidades y los hogares de los pacientes en esta región de alta incidencia, y no se ha diseñado una política de preferencias desde la SMCR local para abordar este problema. Debería desarrollarse una política de apoyo especial sobre la base de perfiles locales de enfermedad, y características de la población, para aliviar la carga financiera que recae sobre las poblaciones en alto riesgo de sufrir ciertas enfermedades con alto coste.
Introduction
Health insurance has the potential to lower financial barriers to health care access and reduces the risk of catastrophic expenditure due to severe diseases, thus improving the health status of insured people 1-3. Developing an efficient and equitable health insurance programme is a focus of attention in almost all countries worldwide 4. After the collapse of planned economy in 1980s in China, rural residents, who made up more than half of the country's total population, were uninsured and had difficulties in accessing affordable healthcare services. To address this crisis, the New Rural Cooperative Medical Scheme (NCMS) was launched by the central government in late 2002 5. NCMS is a government-run, voluntary, community-based, cost-sharing health insurance programme that covers each county as a unit 6. Its aim is to improve the rural population's access to health services and to alleviate poverty due to catastrophic health expenditure. NCMS is financed by contributions from participants and government at different levels. In 2013, the per capita premium increased to 370 Yuan (US$57.80) from an average of 113.36 Yuan in 2009, and NCMS covered 802 million rural residents, accounting for 99% of all rural residents in China 7.
In rural China, medical resources are still limited, so rationally allocating and efficiently utilising medical funds is one of the most crucial issues for NCMS. Like most other health insurance schemes in the world, the NCMS adopts a number of measures to regulate enrollees' utilisation of health services and doctors' medical practices, such as setting deductibles, establishing different reimbursement rates based on hospital level, adopting a national essential drugs list, giving priority to catastrophic diseases.
The Ministry of Health of China also authorised county-level governments to develop their own NCMS policies in compliance with local characteristics. For example, each county can determine its own benefits package. However, in reality, NCMS policies generally were developed by provincial health authorities, mainly due to poor administrative capability of county-level health authorities and the consideration of the administrative costs of the NCMS. Thus, diverse disease profiles and health expenditure patterns among different populations and regions, which were crucial to improve financial protection, have largely been ignored 8.
Cancer, as a major public health issue, is the leading cause of death in developed countries and the second leading cause in developing countries 9. China is one of the highest incidence countries for gastrointestinal cancer, particularly oesophageal and gastric cancer. About 50% of new oesophageal cancer cases and more than 30% of new gastric cancer cases each year are estimated to occur in China 10. Oesophageal cancer and gastric cancer are the 5th and 2nd most prevalent types of cancer in China, respectively, accounting for 20.41% of all cancer cases and 34.81% of cases in rural China 11. With the development of socio-economics and changes in lifestyle, colorectal cancer is also more prevalent in China than before, ranking 3rd in overall cancer incidence, up from 6th, 30 years ago 11.
There is distinct geographical variation in the prevalence of some cancers in China. Hua County of Henan Province, a less-developed county in northern China, belongs to the so-called Central Asian Esophageal Cancer Belt and has one of the highest incidences of oesophageal squamous cell carcinoma in the world 12. The incidence is more than 60/105 in Hua County, which is approximately six times of the national average 11, 13.
The NCMS was introduced in Hua County in 2006. The participation rate has reached 99.9%, covering 1 130 126 people in Hua County in 2010. Deductibles and reimbursement rates by hospital level are shown in Table 1. The NCMS has been the most important and often the only security that local people have in terms of their health 14. However, little consideration was given to the heavy burden of oesophageal cancer when the NCMS reimbursement policy in this county was designed and the real financial burden after NCMS reimbursement remains unknown.
| Hospital level | Deductible (Yuan) | Total hospitalisation cost (Yuan) | Reimbursement rate (%) |
|---|---|---|---|
| Township | 100 | – | 95 |
| County | 500 | – | 85 |
| Prefecture | |||
| Grade 2 or belowa | 1000 | 1000–4500 | 50 |
| >4500 | 70 | ||
| Grade 3a | 1500 | 1500–4500 | 50 |
| >4500 | 70 | ||
| Province | |||
| Grade 2 or belowa | 2000 | 2000–8000 | 45 |
| >8000 | 65 | ||
| Grade 3 or outside Henan Provincea | 3000 | 3000–8000 | 45 |
| >8000 | 65 | ||
- a According to the function, facilities and professional level, hospitals in China are categorised into three grades, with grade 3 as the highest.
In this study, we analysed the reimbursement data extracted from the NCMS management system of Hua County and compared the hospitalisation costs of three gastrointestinal cancers under the NCMS policy. From these findings, we aim to evaluate the financial burden of oesophageal squamous cell carcinoma under the protection of NCMS and to provide evidence and suggestions on policymaking.
Methods
Data source and collection
We obtained claim data for three gastrointestinal cancers – oesophageal, gastric and colorectal – from the NCMS Management System of Hua County. Because outpatient costs account for a small proportion (about 10%) of total medical expenses in cancer therapy 15, in this study, we used inpatient costs to demonstrate financial burden of these diseases. Hospitalisation data of the three types of cancer were indexed and extracted according to the International Classification of Diseases (10th revision, ICD-10), specifically, codes C15.051 to C15.901 for oesophageal cancer, codes C16.001 to C16.906 for gastric cancer and codes C18.201 to C21.853 for colorectal cancer. Cardia cancer (C16.001 to C16.051) and non-cardia gastric cancer (C16.101 to C16.906) were grouped into gastric cancer.
We used an annual timeframe based on the date of reimbursement and included all inpatient claim data from 1 January 2013 to 31 December 2013, irrespective of the time of disease onset. In total, data from 2375 hospital discharges of 1211 patients with the studied gastrointestinal cancers were collected, with 40.13% (486 patients) of those claims having more than one hospitalisation during the study period.
The contents of their medical abstract form consisted of NCMS ID card number, patient name, age, gender, admission and discharge dates, reimbursement date, name of hospital, therapy method (surgical or non-surgical treatment depending on whether ‘surgery operation fee’ was reimbursed), length of stay, diagnosis (disease name and ICD code) and the claim data, including total hospitalisation cost, the cost covered by NCMS, reimbursements and deductibles. Patients' information was anonymised before analysis.
Statistical analyses
We calculated a series of cancer-specific indicators to reflect financial burden, including annual total cost of hospitalisation, average cost per hospitalisation, average out-of-pocket cost per hospitalisation, total cost relative to gross domestic product (GDP) of Hua County in 2011, cost per hospitalisation relative to GDP per capita of Hua County in 2011, out-of-pocket cost per hospitalisation relative to per capita disposable income of Hua County in 2011 and out-of-pocket proportion (the proportion of out-of-pocket costs per hospitalisation to total cost per hospitalisation). For the purpose of comparison among the three types of cancer, indicators of cost and out-of-pocket cost per hospitalisation were adjusted for age and gender using a general linear regression model.
All costs were expressed in 2011 prices and converted to 2011 US dollars. Data analyses were performed using Stata/SE 11.0 for Windows.
Results
In 2013, a total of 1211 patients with gastrointestinal cancer claimed reimbursements for hospitalisation expenditures, including 695 (57.4%) patients with oesophageal cancer, 341 (28.2%) patients with gastric cancer and 175 (14.5%) patients with colorectal cancer (Table 2). Most patients were between 60 and 69 years old, and there were more male patients than female ones, particularly for gastric cancer (78.01% vs. 21.99%). Due to multiple hospitalisations for some patients, a total of 2375 discharges occurred in 2013, and 53.1% of those were due to oesophageal cancer. Nearly, half of the gastrointestinal cancer patients chose county-level hospitals to have their cancer treated, followed by prefecture- and province-level hospitals; only 5–10% chose township health centres. About one-quarter of the patients underwent surgical procedures during hospitalisation, and others were mainly treated with internal medicine protocols. Oesophageal cancer patients had the longest median length of stay (11 days) compared with gastric cancer patients (9 days) and colorectal cancer patients (7 days).
| Characteristics | Oesophageal cancer | Gastric cancera | Colorectal cancer |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Age group (years) | |||
| <40 | 4 (0.58) | 5 (1.47) | 17 (9.71) |
| 40–49 | 21 (3.02) | 27 (7.92) | 30 (17.14) |
| 50–59 | 96 (13.81) | 46 (13.49) | 32 (18.29) |
| 60–69 | 318 (45.76) | 139 (40.76) | 57 (32.57) |
| 70–79 | 180 (25.90) | 104 (30.50) | 28 (16.00) |
| ≥80 | 76 (10.94) | 20 (5.87) | 11 (6.29) |
| Median (IQR) | 66 (60.72) | 65 (59.72) | 57 (45.66) |
| Gender | |||
| Female | 284 (40.86) | 75 (21.99) | 83 (47.43) |
| Male | 411 (59.14) | 266 (78.01) | 92 (52.57) |
| Totalb | 695 (100.00) | 341 (100.00) | 175 (100.00) |
| Hospital levels | |||
| Township level | 121 (9.60) | 30 (4.52) | 23 (5.11) |
| County level | 522 (41.40) | 334 (50.30) | 207 (46.00) |
| Prefecture level | 440 (34.89) | 213 (32.08) | 132 (29.33) |
| Province level | 180 (14.27) | 87 (13.10) | 88 (19.56) |
| Therapy methodsc | |||
| Non-surgical treatment | 922 (73.12) | 517 (77.86) | 342 (76.00) |
| Surgical treatment | 339 (26.88) | 147 (22.14) | 108 (24.00) |
| Length of stay | |||
| ≤7 days | 373 (29.58) | 282 (42.47) | 244 (54.22) |
| 8–14 days | 379 (30.06) | 188 (28.31) | 77 (17.11) |
| 15–21 days | 169 (13.40) | 96 (14.46) | 64 (14.22) |
| ≥22 days | 340 (26.96) | 98 (14.86) | 65 (14.44) |
| Median (IRQd) | 11 (7,23) | 9 (6,16) | 7 (5,16) |
| Totalb | 1261 (100.00) | 664 (100.00) | 450 (100.00) |
- a Gastric cancer includes cardia cancer and non-cardia gastric cancer.
- b For gender and age distribution, cancer patients were adopted as a calculation unit, and for hospital levels, therapy methods and inpatient days of hospitalisation were adopted as calculation units.
- c Patients were categorised into surgical and non-surgical groups on the basis of whether the patient accepted surgical treatment within the corresponding hospitalisation.
- d Interquartile range.
Table 3 shows the financial burden of gastrointestinal cancer. The annual inpatient cost of gastrointestinal cancer totalled $4.44 million, accounting for 4.62% of total all-cause hospitalisation expenditure in Hua County in 2013 or 1.86‰ of the annual GDP of the county in 2011. To treat oesophageal cancer, $2.7 million were spent, accounting for 1.13‰ of the annual GDP and 2.80% of the all-cause hospitalisation expenditure of the whole county; these expenditures were 2.7 times higher than those for gastric cancer and 3.6 times higher than those for colorectal cancer. Oesophageal cancer also resulted in the highest cost per hospitalisation (1.05 years' GDP per capita) and out-of-pocket cost per hospitalisation (0.94 years' per capita disposable income).
| Oesophageal cancer | Gastric cancerb | Colorectal cancer | |
|---|---|---|---|
| Combined | |||
| Total cost | 2 691 806.33 | 986 568.95 | 757 432.26 |
| Total cost/GDPc or total hospitalisation cost of all diseasesd | 1.13‰ or 2.80% | 0.41‰ or 1.03% | 0.32‰ or 0.79% |
| Cost per hospitalisation | 2075.16 | 1712.35 | 1516.18 |
| Cost per hospitalisation/GDP per capitae | 1.05 | 0.87 | 0.77 |
| Out-of-pocket cost per hospitalisation (out-of-pocket proportion, %f) | 1015.81 (49%) | 854.83 (50%) | 798.10(53%) |
| Out-of-pocket cost per hospitalisation/PCDIg | 0.94 | 0.79 | 0.74 |
| Surgical treatmenth | |||
| Total cost | 1 246 925.58 | 504 898.68 | 425 988.77 |
| Total cost/GDPc | 0.52‰ | 0.21‰ | 0.18‰ |
| Cost per hospitalisation | 3618.85 | 3710.65 | 3757.12 |
| Cost per hospitalisation/GDP per capitae | 1.83 | 1.88 | 1.90 |
| Out-of-pocket cost per hospitalisation (out-of-pocket proportion, %f) | 1824.56 (50%) | 1857.58(50%) | 1888.29 (50%) |
| Out-of-pocket cost per hospitalisation/PCDIg | 1.68 | 1.72 | 1.74 |
| Non-surgical treatmenth | |||
| Total cost | 1 444 881.40 | 481 670.10 | 331 443.44 |
| Total cost/GDPc | 0.61‰ | 0.20‰ | 0.14‰ |
| Cost per hospitalisation | 1507.57 | 1144.17 | 808.51 |
| Cost per hospitalisation/GDP per capitae | 0.76 | 0.58 | 0.41 |
| Out-of-pocket cost per hospitalisation (out-of-pocket proportion, %f) | 718.45 (48%) | 569.72 (50%) | 453.83 (56%) |
| Out-of-pocket cost per hospitalisation/PCDIg | 0.66 | 0.53 | 0.42 |
- a Indicators of cost and out-of-pocket cost per hospitalisation were adjusted for age and gender using a general linear regression model.
- b Gastric cancer includes cardia cancer and non-cardia gastric cancer.
- c GDP: Gross Domestic Product of Hua County in 2011.
- d Total hospitalisation cost of all diseases in Hua County in 2013.
- e GDP per capita: Gross Domestic Product per capita of Hua County in 2011.
- f Proportion of out-of-pocket cost per hospitalisation to total cost per hospitalisation.
- g PCDI: Per Capita Disposable Income of Hua County in 2011.
- h Patients were categorised into surgical and non-surgical groups on the basis of whether the patients accepted surgical treatment within the corresponding hospitalisation.
Stratum analysis by treatment measure showed that the indicators based on the total cost, which correlate with the overall incidence, were also highest for oesophageal cancer, for both surgical and non-surgical hospitalisations. Regarding the ‘per hospitalisation’-based indicators, for example average total cost per hospitalisation, the highest values were found for non-surgical hospitalisations for oesophageal cancer, whereas little difference was detected for surgical hospitalisations. Similar reimbursement rates among the three cancers were observed irrespective of the treatment measures.
Figure 1 shows the average total cost per hospitalisation and the actual reimbursement rates of gastrointestinal cancers in different levels of hospitals according to therapy methods. The average total cost per hospitalisation for surgical therapy was notably higher than that of non-surgical therapy across all levels of hospitals and also increased more sharply than did non-surgical therapy as the hospital-level rose.
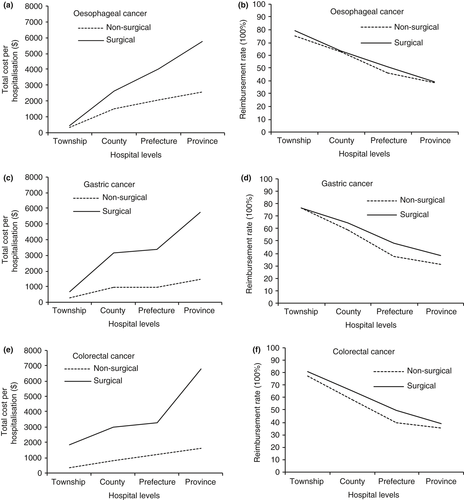
Two characteristics of oesophageal cancer therapy can be summarised in comparison with the other two types of cancer: First, the total cost per hospitalisation increased monotonically with the elevation of hospital level in the surgical group, whereas similar total costs per hospitalisation between county- and prefecture-level hospitals were observed for gastric and colorectal cancers. Second, in the non-surgical group, the corresponding increasing rate of the average total cost per hospitalisation from township health centres to province-level hospital for oesophageal cancer ($301 vs. $2589, 860%) was much higher than those for either gastric cancer ($289 vs. $1453, 503%) or colorectal cancer ($359 vs. $1610, 448%). The actual reimbursement rates for the three gastrointestinal cancers fell with rising hospital level and were similar among the three cancers at the same hospital level.
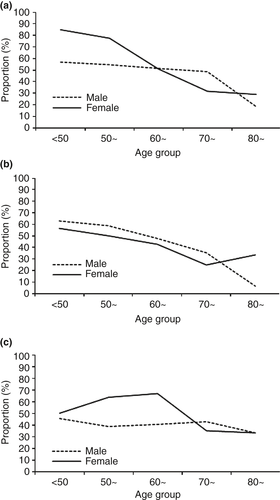
As shown in Figure 2, the proportion of patients who chose to have their cancer treated at a high-level (prefecture or provincial) hospital generally declined with increasing age, a trend that was most distinct among female oesophageal cancer patients and male gastric cancer patients. Overall, patients older than 70 years were least able to access high-level hospitals. Regarding gender, men with oesophageal cancer and men with colorectal cancer who were younger than 60 years were more limited in their choice of high-level hospitals than were female patients.
Discussion
In this study, we analysed NCMS claim data to evaluate the financial burden of gastrointestinal cancer and the protection effect of NCMS in a high-incidence region for oesophageal cancer in rural China. Compared with that of gastric and colorectal cancers, the total burden of oesophageal cancer is particularly serious, and no special protection in the NCMS was designed in the county. An entire year's GDP per capita and per capita disposable income could be expended to the community and the patient's household for a single hospitalisation to treat oesophageal cancer. Unequal access to high-level medical service to treat cancer was also detected, which might be mainly due to economic concerns. To our knowledge, this report is the first evaluation on the disease burden and protection effect of the NCMS focusing on gastrointestinal cancer in a Chinese high-incidence region.
The NCMS is a crucial step in narrowing the insurance gap and improving equity in access to healthcare for rural populations in China. Through years of development, the security level and coverage of the scheme have been greatly increased. Although study results are inconclusive on whether the NCMS has lightened the financial burden for rural residents, the scheme has improved the situation of hard-to-receive healthcare services 16. The NCMS provides a representative model for all countries, especially for developing countries, which face fewer resources and a heavy healthcare burden.
Costs of cancer care are rising and consume an increasing share of expenditures at all budgetary levels, from individual to national 17, 18. We found that oesophageal cancer imposes a serious medical burden to a high-risk population, with its prevalence of hospitalisation ranked first among different cancers. The total hospitalisation costs of oesophageal cancer accounted for 2.80% of all-cause hospitalisation costs in Hua County in 2013 and were 2.72 higher than those for gastric and 3.54 times higher than those for colorectal cancer. Almost 1 year of per capita disposable income was used for one hospitalisation for oesophageal cancer treatment after reimbursement, which was more than for gastric and colorectal cancers that enjoy very similar reimbursement rates from the NCMS. Moreover, the average length of stay for oesophageal cancer was longer than for the other two gastrointestinal cancers, leading to higher direct costs of medical therapy and indirect costs due to monetary losses. However, special reimbursement policies for oesophageal cancer are still lacking in the NCMS policy.
In 2012, the Chinese government initiated a nationwide healthcare programme to relieve the medical burden of 20 high-cost diseases based on NCMS, including oesophageal, gastric and colorectal cancers, by ensuring that their reimbursement rates would not be less than 70% 19. However, according to our study, gastrointestinal cancers, particularly oesophageal cancer, still impose a burden in this high-incidence region mainly because of self-financed treatment items particularly at high-level hospitals. Covering more expenditure items and further elevating the reimbursement rate at high-level hospitals should be effective in relieving the burden for both patients' households and the community in areas with high-prevalence diseases.
As expected, total cost per hospitalisation rose rapidly, and the real reimbursement rate fell as the hospital level increased, which was mainly due to different deductibles and reimbursement policies for hospitals of different levels. This economic leverage was designed to deter patients from crowding at high-level medical institutions. However, for patients with catastrophic diseases, such as oesophageal cancer, it may also result in economic obstacles for selecting appropriate medical institutions, particularly for certain vulnerable subgroups (e.g. elderly and impoverished patients).
Although NCMS coverage among the rural elderly is high, it is still insufficient to improve access to quality healthcare services for that population and to protect them from financial catastrophe and household impoverishment due to high co-payments 20-22. In Zhejiang and Shandong, two eastern provinces with relatively developed economics, as many as 52.2% of elderly rural residents still face affordability difficulty 23, 24. In our study, elderly rural residents were also more likely to be hospitalised at lower level hospitals with high reimbursement rates for low-cost treatment than were younger groups, which was particularly distinct for patients older than 70 years.
With regard to gender differences, we found that male patients younger than 60 years with oesophageal and colorectal cancers were more likely to choose lower level hospitals than female patients of the same age. This finding was unexpected because in traditional Chinese society, the social status of men is supposed to be higher than that of women, especially in rural China, which theoretically should lead to more access to higher levels of medical services for men. We speculated that, with the development of socio-economics in rural China, Chinese rural women are playing more important roles in both families and communities than ever before. Meanwhile, men in rural Chinese families have relatively lower health consciousness and are more likely than women to neglect their health due to intense work and life pressures 25, 26. This secular trend in Chinese society over the past several decades may potentially explain the vulnerability observed among younger male patients. Measures should be taken to narrow the healthcare gap between younger and older patients in rural China and to increase equity in healthcare service utilisation. Moreover, how to improve the health consciousness in men and simultaneously relieve them from the stresses of life is a complicated social problem rather than a single medical issue.
We also interviewed the director and staff of the Hua County NCMS Management Office about the local NCMS reimbursement policy. The Hua County NCMS Management Office is authorised only to regulate the reimbursement rates of county- and township-level hospitals under the guidance of the provincial management office, which was merely based on the balance of the NCMS fund rather than on disease profiles and local patterns of financial burden. Apart from the consideration of administration costs from the provincial government, limited management capability and motivation of county-level health authorities may also lead to the inflexible and non-specific NCMS policy. To populations at high risk for high-cost diseases, such as cancer in rural China, a special reimbursement policy should be established. In addition, human resource training for county-level NCMS management should also be conducted to enhance their management capacity of NCMS policy based on the pattern of local disease burden and the dynamic situation of the balance of the NCMS medical fund 27.
According to the NCMS regulation, a relatively large portion of NCMS funds should be frozen in the county-level NCMS account. As of 2013, the cumulative surplus of NCMS funds had reached approximately 50 million Yuan (US$7.81 million) in Hua County. Therefore, to address this critical issue, a portion of these NCMS funds should be used for high-incidence catastrophic disease reimbursement locally if the medical expenditure exceeds a certain limit (i.e. the annual per capita disposable income). If the local NCMS system cannot bear the burden, we suggest that the provincial or even national government initiate another medical support programme exclusively focusing on fatal and high-cost diseases in high-risk regions or populations on the basis of the population-specific disease profile, to relieve the extremely heavy burden brought by these diseases. From the perspective of ‘expenditure reduction’, hospitals and doctors should be encouraged to save costs by reforming the payment system to further relieve the burden brought by high-cost diseases in high-risk populations.
This study has two limitations. First, the data are only from NCMS claims for hospitalisations, thus outpatient expenditures were not analysed, which leads to an underestimation of the financial burden to a certain extent. However, prior studies have shown that outpatient costs contribute a small portion (10%) of cancer treatment expenses 15, so the main conclusions of this study, especially the comparison among the three cancers, should not be significantly affected. Second, initial diagnosis cannot be distinguished based on the claim data, so we could calculate only the average cost per hospitalisation, although the initial cost is usually higher than subsequent costs 28.
Conclusion
In summary, in this high-incidence region in rural China, oesophageal cancer has imposed heavy financial burdens to patients' households and the community, and vulnerable groups also exist in terms of accessing high-quality medical service. However, no special consideration has been given to the disease profile in this population in designing local NCMS policy. To populations at high risk for high-cost diseases, such as cancer in high-incidence region of rural China, a special reimbursement policy should be established. Meanwhile, county-level health officials should also be trained to improve their management capacity so that the dynamic regulation of local NCMS reimbursement policy could take the pattern of local disease burden into account.
Acknowledgements
This work was funded by National Ministry of Health [201202014], the National Natural Science Foundation of China [81473033] and National Ministry of Science and Technology [2012AA02A209, 2012AA022502].
Appendix 1: Financial burden (converted to 2011 international dollars) of gastrointestinal cancer in Hua County, China, 2013 (cost and out-of-pocket cost per hospitalisation were true values)
| Oesophageal cancer | Gastric cancera | Colorectal cancer | |
|---|---|---|---|
| Combined | |||
| Total cost | 2 691 806.33 | 986 568.95 | 757 432.26 |
| Total cost/GDPb or total hospitalisation cost of all diseasesc | 1.13‰ or 2.80% | 0.41‰ or 1.03% | 0.32‰ or 0.79% |
| Cost per hospitalisation | 2134.66 | 1485.79 | 1683.19 |
| Cost per hospitalisation/GDP per capitad | 1.08 | 0.75 | 0.85 |
| Out-of-pocket cost per hospitalisation (out-of-pocket proportion, %e) | 1044.76 (49%) | 745.43 (50%) | 879.03 (52%) |
| Out-of-pocket cost per hospitalisation/PCDIf | 0.96 | 0.68 | 0.81 |
| Surgical treatmentg | |||
| Total cost | 1 246 925.58 | 504 898.68 | 425 988.77 |
| Total cost/GDPb | 0.52‰ | 0.21‰ | 0.18‰ |
| Cost per hospitalisation | 3678.24 | 3434.69 | 3944.34 |
| Cost per hospitalisation/GDP per capitad | 1.86 | 1.73 | 1.99 |
| Out-of-pocket cost per hospitalisation (out-of-pocket proportion, %e) | 1865.59 (51%) | 1666.28 (49%) | 2017.88 (51%) |
| Out-of-pocket cost per hospitalisation/PCDIf | 1.71 | 1.53 | 1.85 |
| Non-surgical treatmentg | |||
| Total cost | 1 444 881.40 | 481 670.10 | 331 443.44 |
| Total cost/GDPb | 0.61‰ | 0.20‰ | 0.14‰ |
| Cost per hospitalisation | 1567.11 | 931.66 | 969.12 |
| Cost per hospitalisation/GDP per capitad | 0.79 | 0.47 | 0.49 |
| Out-of-pocket cost per hospitalisation (out-of-pocket proportion, %e) | 742.96 (47%) | 483.59 (52%) | 519.39 (54%) |
| Out-of-pocket cost per hospitalisation/PCDIf | 0.68 | 0.44 | 0.48 |
- a Gastric cancer includes cardia cancer and non-cardia gastric cancer.
- b GDP: Gross Domestic Product of Hua County in 2011.
- c Total hospitalisation cost of all diseases in Hua County in 2013.
- d GDP per capita: Gross Domestic Product per capita of Hua County in 2011.
- e The proportion of out-of-pocket cost per hospitalisation to total cost per hospitalisation.
- f PCDI: Per Capita Disposable Income of Hua County in 2011.
- g Patients were categorised into surgical and non-surgical groups on the basis of whether the patients accepted surgical treatment within the corresponding hospitalisation.