Automated external defibrillator location selection considering myocardial infarction risk and medical resources
Abstract
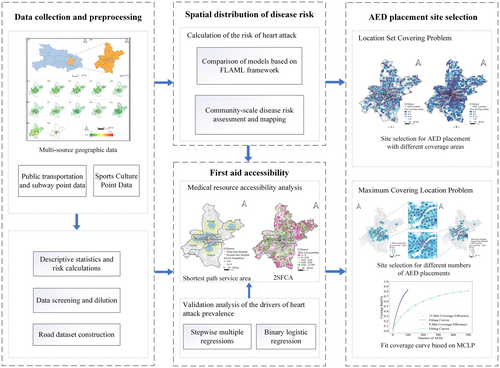
The effective deployment of medical emergency equipment, such as automated external defibrillator (AED), is essential to myocardial infarction (MI) patients. However, there are shortcomings in current studies that simultaneously consider the risk of MI and the availability of medical resources when siting the AEDs. In this study, an AED site recommendation framework was proposed to address the lack of consideration for both the MI risk and medical resources when siting the AEDs. It conducts the AED sitting under different scenarios considering the spatial distribution of MI risk and healthcare accessibility in Chinese cities. First, an automated machine learning framework data is proposed to estimate the MI risk at the community scale based on multi-source spatio-temporal. Second, the accessibility of medical resources was calculated by an improved Gaussian two-step moving search algorithm. Finally, the AED siting in multiple scenarios is conducted based on the coverage model. The performance of the AED siting model was evaluated at Wuhan city. The results show that MI risk is impacted by both socioeconomic and cultural characteristics (municipal utilities, streetscape environment, educational and commercial facilities). There is a strong spatial heterogeneity in the distribution of both MI risk and medical resources in Wuhan, and an unreasonable match between the two was detected in some regions. Medical resources need to be strengthened in some high-risk areas, such as rural areas and tourist attractions. In addition, 1015 AED candidate sites were identified by the location set covering problem model, with a 15-min accessibility rate of 96.5%. Given the limited resources, mobile AEDs which have about 15-min service range can be deployed based on the maximum covering location problem model to meet the demand in central urban areas efficiently. This study can contribute to more rational selection of AED sites and the prevention of myocardial infarction among residents, particularly when supported by policies that promote balanced regional development of pre-hospital medical emergency networks.
1 INTRODUCTION
Myocardial infarction (MI) poses a significant risk to human health (Coughlin & Young, 2020), and is recognized as one of the leading causes of out-of-hospital cardiac arrest (OHCA) (Bergman et al., 2016). Automated external defibrillators (AEDs) are essential facility to rescue sudden cardiac arrest (Kiyohara et al., 2020), which are necessary parts of public health systems (Morin et al., 2022). In order to provide effective treatment within the “golden four minutes” of MI (Hong & Dorian, 2005), governments have initiated strategies for AED deployment to reduce mortality from cardiac emergencies (Delhomme et al., 2019). Compared to developed countries, developing country, such as China, has a lower penetration of AED deployment (Shaozhou et al., 2019) and uneven AED deployment among different cities or regions (Zhang et al., 2019). Compared to the rapid urbanization, its AED deployment is seriously lagging, with problems such as a lack of social awareness, limited medical resources, and a lack of scientific and practical siting plans (Wang et al., 2022). There is an urgent need to improve the optimal layout of AEDs to reduce the risk of death from OHCA, especially OHCA patients caused by MI with higher mortality rate (Tømte et al., 2011).
How to more rationally deploy and balance the emergency medical system under government budget constraints is very important. At this time, the siting of AEDs is controlled by two main factors, exposure to risk and healthcare accessibility. First, AEDs need to be prioritized and deployed in high-risk areas (Chan et al., 2016). Therefore the spatial distribution of risk has an important influence on the siting of AEDs (Derevitskii et al., 2020). Some scholars consider patients' health condition (Rathore et al., 2018), environmental pollution (Raziani & Raziani, 2021), the percentage of green in the streetscape (Yao, Xu, et al., 2022), socioeconomic environment (Leung et al., 2021; Roth et al., 2019), and mental health factors (Jackson et al., 2018) on the drivers of MI. The spatial mapping and assessment of the MI risk are little discussed. To address this problem, Derevitskii et al. (2020) used risk-based data to generate artificial OHCA data to optimize the placement of AEDs and achieved better results compared with historical OHCA data. Other researchers evaluate the spatial risk of OHCA from the perspectives of land use and population density (Chen et al., 2015; Chrisinger et al., 2016), and conduct research on the location selection of indoor (Chan, 2017) and outdoor (Chen et al., 2023) AEDs based on OHCA risk. The results illustrate the validity of optimal AED siting based on risk data. Yao, Xu, et al. (2022) constructed an RFA-based SHAP interpretable model to explore the spatiotemporal risk factors for MI. However, there is a widespread incompleteness of data on MI risk due to incomplete hospital records and privacy concerns (Nowbar et al., 2019). To address this difficulty, a data-driven approach based on machine learning has been proposed to predict MI risk with high accuracy (Alaa et al., 2019).
Second, the spatial and temporal accessibility of AED devices has a great impact on their spatial placement and service coverage (Karlsson et al., 2019). Due to the suddenness of OHCA which may caused by MI or any other reasons, the “golden 4 minutes” of efficient treatment time is an important reference for AED deployment (Weisfeldt & Becker, 2002). In addition, in terms of urban public service coverage, scholars have proposed a “15-minute community living circle” to guide urban planning based on multi-source spatiotemporal data and matching supply and demand (Li et al., 2019; Pozoukidou & Chatziyiannaki, 2021; Wu et al., 2021). It is widely used in healthcare (Li, 2022) and provides a reference for validating the rationality of AED site selection.
In the assessment of spatial accessibility in public health, scholars have used regional availability models (Luo & Wang, 2003), kernel density models (Guagliardo, 2004), closest distance models (Liu et al., 2019), gravity models (Shi et al., 2022), and floating catchment model (Chen & Jia, 2019) to carry out the study. These methods have been widely used in studies on the spatial accessibility of AEDs, and the Bayesian spatial model (Tierney et al., 2019), indoor AEDs accessibility spatial search algorithm (Yang et al., 2021), topological catchment areas (Gianquintieri et al., 2019) and other models are also proposed for different application scenarios. However, some problems exist in these studies such as the lack of spatial detail and low computational efficiency (Kim et al., 2018). The 2-Step Floating Catchment Area (2SFCA) method can assess medical accessibility by integrating the supply and demand of healthcare. It can compensate for the shortcomings of the above models by refining the data sources, which can accurately reflect accessibility at smaller spatial scales. For example, Pan et al. (2018) combined human actual travel behavior to construct the Enhanced Two-Step Floating Catchment Area (ESFCA) method to assess the accessibility of medical facilities in Shenzhen, China. Lin et al. (2016) investigate the local risk and optimal deployment of AEDs based on the Multi-Criterion 2-Step Floating Catchment Area (MC2SFCA) algorithm. Karlsson et al. (2018) evaluate the accessibility of each AED by calculating the actual distance between the OHCA and AED. However, few scholars have utilized the spatial risk distribution pattern of MI to measure AED accessibility. According to data from Duerschmied et al.'s relevant study, approximately two-thirds of OHCA patients in their hospital have severe and sustained MI (Duerschmied et al., 2020). This highlights the representativeness and importance of MI risk for OHCA risk. Furthermore, there is a research gap in analyzing AED accessibility based on cardiac arrest risk data, which has a more precise quantitative ability to evaluate the suitability of AEDs for emergency treatment of OHCA. Thus, there is a lack of further research on optimal AED siting.
Along with the abundance of multi-source spatio-temporal data and the development of geo-information technology, more advanced AED siting models have been proposed. Studies have used coverage models (Pourghaderi et al., 2022), P-median models (Jia et al., 2014), cross-median models (Chen et al., 2020), and the exact center of gravity models (Hanifha et al., 2020) to analyze the spatial siting of urban public health facilities, and have been partially applied to the siting of AEDs (Lee et al., 2019). However, the impact of accessibility to the existing healthcare system for MI on the siting of AEDs has generally not been considered. With the development of transportation tools such as drones, the deployment and timely application of mobile AEDs have also received widespread attention (Morin et al., 2022; Nelson et al., 2015). Hajari et al. (2020) modeled public buses as mobile platforms carrying AEDs and showed that AED coverage was greatly improved. But this study also found that mobile AEDs cannot be used as a stand-alone deployment strategy.
The optimal siting of AEDs based on the combination of MI risk and medical accessibility is an innovative and vital issue. The incidence of sudden cardiac death and its location is an essential reference for the spatial allocation of emergency medical services (Priori et al., 2004). However, due to the complexity of spatial and temporal factors and differences in resource availability in different regions, there are difficulties in obtaining data and integrating methods to fully consider the risk of MI and medical accessibility in the AED siting process (Tierney et al., 2019). It is also difficult to measure the impact of socio-demographic and economic factors in AED siting based directly on the risk of MI without considering community accessibility, resulting in AED siting results that do not match actual needs (Brown et al., 2022).
This study aims to address two scientific questions: (1) How to assess the accessibility of existing medical resources at the community scale? and (2) How to select the location for additional AEDs under different resource conditions based on accessibility to medical facilities? A multi-source spatiotemporal data-driven model was proposed to conduct the AED location recommendation. It consists of the MI mapping based on an automated machine learning framework and the medical accessibility estimation based on 2SFCA. Based on this, the coverage model is coupled to explore the siting of AED in multiple scenarios. Wuhan, Hubei Province, was selected as the study area to verify the performance of the proposed model. The location set covering problem (LSCP) model and maximum covering location problem (MCLP) model are compared to provide a reference for AED delivery in Chinese cities.
2 MATERIALS AND METHODS
This study consists of three main steps: First, based on the risk data of MI patients, an automated machine learning framework is used to complement the spatial distribution pattern of MI prevalence risk at the community scale in Wuhan City. Second, this study uses 2SFCA to evaluate the accessibility of MI to existing medical resources in the study area. Multiple regression and binary logistic regression analyses were used to characterize the association between accessibility and socioeconomic characteristics in different regions. The driving factors of MI were explored. Finally, based on the accessibility, the siting of AED devices under different conditions is discussed based on the LSCP and the MCLP model to provide a theoretical basis for improving the healthcare system (Figure 1).
2.1 Study area and data
2.1.1 Study area
The selected study area in Wuhan, Hubei Province, which is a mega-center city with a population of over 10 million (Figure S1a,b). With a total area of 8569.15 km2 and a resident population of 13,648,900, it is the economic and geographical center of central China. Wuhan has 13 administrative districts, of which Hankou (Hanyang, Jiangan, Jianghan, and Qiaokou Districts) is the commercial and financial center with high population density. Wuchang and Hongshan districts are educational centers (university cities) with a high density of universities. Qingshan District is an industrial area with a developed energy industry. The districts of Huangpi, Xinzhou, Jiangxia, Hannan, Caidian and East–West Lake are more rural and less densely populated suburban areas. Three hundred sixty-two hospitals and three emergency centers were located in Wuhan in 2020. Compared to its large urban area and high population density, the emergency medical system in Wuhan is still inadequate, and the number of AEDs available to the community is <1000 (Hou et al., 2021), resulting in an imbalance in medical resources and a high mortality rate of acute MI in remote areas (Hubei Health Commission, 2022). Therefore, the study of accessibility and optimal AED siting in Wuhan is an essential reference for the siting of new AED devices and effective disease prevention in megacities in China.
2.1.2 Data on myocardial infarction patients
This study used data from patients with MI who attended a tertiary hospital in Wuhan between 2016 and 2019 at that hospital (Yao, Yin, et al., 2022). The data has been pre-processed for privacy protection and will not reveal the patient's identity. The data content is shown in Table S1. In order to better assess the community-scale risk, which is the basic unit of urban space with an average area of 2.43 km2, this study used the natural breakpoint method to classify patients into 10 levels of risk (Figure S2), based on the length of hospitalization and health care consumption of MI patients (Loudon et al., 2016). Studies have shown that in-hospital treatment of acute MI has increased which also illustrates the broad representation of data on in-hospital MI patients (McNamara et al., 2016; Mozaffarian et al., 2016). MI is one of the important causes of OHCA (Bergman et al., 2016), and OHCA patients with MI have a higher risk of death (Kosugi et al., 2020; Tømte et al., 2011). These further demonstrate the validity of using data from patients with MI to assess the risk of OHCA. Of course, the actual patient's data are often insufficient due to the lack of unrecorded data outside the hospital, but the neighborhood characteristics of the geographical distribution of MI risk will make the risk spatial distribution pattern have the same law as a whole (Kihal-Talantikite et al., 2017). Based on this idea, we use multi-source spatial–temporal data to carry out risk prediction processing, so as to fit its risk spatial distribution law as much as possible.
2.1.3 Multi-source geographic data
This study collected OSM (OpenStreetMap) road network data and Point of Interest (POI) data for healthcare facility accessibility analysis. OSM is a representative spontaneous geographic information (VGI) data with global project coverage and free and easily accessible data, which can be used for access route planning and research related to healthcare facility location (Das & Alam, 2014).
Points of interest (POIs) mainly refer to geographical entities closely related to people's lives and are widely used in urban public health and safety evaluation (Huang et al., 2022; Psyllidis et al., 2022; Yao, Yin, et al., 2022). A total of 377,000 POI data were used in this study, covering transportation, sports and culture, municipal utilities, health care, education, and business and finance, which can be used as a comprehensive measure of the city's economic development and public health resources (Tu et al., 2022). In addition, location data of existing second and third-degree hospitals in Wuhan were obtained to support the accessibility evaluation of existing medical facilities and the siting of new AEDs.
Population density is one of the important influencing factors for the spatial distribution of healthcare facilities (Kim et al., 2018). This work collected Wuhan Tencent time-series population density data, including the time-series population density of a weekday, rest day and holiday in Wuhan in 2019, with a spatial resolution of 25 m and a temporal resolution of 1 h (https://heat.qq.com/bigdata/production.html). The data records the location of Tencent users every hour, among which approximately 570 million users use WeChat every day, which is more than one-third of China's population (Yao, Yin, et al., 2022). So the Tencent time-series population density data can effectively reflect the population's activity patterns and socioeconomic characteristics (Li et al., 2021; Yao, Xu, et al., 2022). In this study, it is used to predict the risk level of MI at each community scale (Figure S1).
Studies have shown that meteorological and street-level environmental data have a significant impact on the incidence of MI (Münzel et al., 2021). This work explores the spatial characteristics of the risk of MI based on such data. In particular, meteorological data were obtained from the Public Meteorological Service Centre of the China Meteorological Administration (https://www.cma.gov.cn/), based on the time and spatial matching before and after the patients' admission, including temperature, air quality index and concentration indicators of various air pollutants. The street view data is based on the deep learning model proposed by Yao et al. (2019), which is based on Tencent Street View images to obtain the street view feature occupancy ratio, with a training accuracy of 0.81 and a testing accuracy of 0.67 (Yao et al., 2019).
2.2 Exploring spatial patterns of myocardial infarction prevalence and risk prediction
Exploring the distribution patterns of OHCA risk calculated by MI risk data can provide a spatial reference for AED siting considering accessibility (Moran, 2021). As mentioned before, MI is one of the important causes of cardiac arrest, and cardiac arrest patients are closely related to heart disease patients. There are commonalities between two groups (such as the elderly population, high blood pressure, etc.), so we believed that it is effective to measure urban emergency risk and assist in the deployment of AED equipment based on existing MI data. However, our data exhibits sparse spatial distribution. In such circumstances, constructing a model based on additional variables to densify the spatial data proves to be an effective approach to mitigate data bias and incompleteness. In this work, spatial autocorrelation analysis was first used to characterize the spatial clustering of MI risk, followed by a multi-source spatio-temporal data-driven approach to predict the risk pattern.
2.2.1 Spatial autocorrelation analysis of the risk of myocardial infarction
2.2.2 FLAML-based risk prediction for the development of community-scale myocardial infarction
In this work, the risk of MI was predicted based on FLAML. Firstly, the number of MI patients in the community and the corresponding risk levels were counted, and the community risk was classified into 10 levels according to the quantile method, with higher levels implying a higher risk of disease. Secondly, a multi-source multi-variables MI risk model was constructed to predict the risk level of the surrounding areas, using the number of POIs, population and plot area at the community scale as independent variables and the risk level of the central city of Wuhan as dependent variables. Finally, the model constructed using the LightGBM algorithm was chosen for prediction. LightGBM is a gradient boosting framework rooted in the decision tree algorithm. In each iteration, a new decision tree model is trained based on the negative gradient of the loss function, and the optimal split point is determined through the histogram algorithm to maximize the gain. This approach significantly diminishes memory usage and training time while exhibiting superior performance on sparse data. Above all, the results were spatially analyzed to provide mapping support for exploring the inadequate spatial distribution of medical facilities and disease prevention.
2.3 Accessibility assessment to AED for myocardial infarction based on Gaussian two-step moving search algorithm
- Calculate the hospital the ratio of supply to demand. The number of suppliable beds is determined according to the hospital class and recorded as Sj. The total population within a buffer zone radius of d0 is calculated to obtain the supply/demand ratio for that hospital. The calculation is as follows.
- Calculating hospital accessibility. The accessibility of each community is the sum of the supply and demand ratios of all hospitals within the threshold range d1 of the center of gravity. A Gaussian distance decay function and a risk level for MI were introduced to make the model more reasonable for predicting the actual situation, which was calculated as follows (Abubakar, 2021).
In addition, we analyzed the existing hospital service areas using the shortest path method. The spatial distribution of risk and accessibility is explored through comparative and regression analyses.
2.4 Site selection for AED devices based on coverage models
Equation (10) indicates that the number of AED candidate points is negatively correlated with accessibility, where the value of c can be adjusted according to the number of candidate points and Acc is the level of access to care for MI determined by population density, risk of MI, supply and demand.
To further discuss the siting of AED devices under different resource constraints, this work uses the Maximum Covering Location Problem (MCLP) model to meet as many requests for coverage as possible with a limited number of AEDs to improve service efficiency (Taiwo & Orunmuyi, 2021).
In this study, public transportation facilities (e.g. bus stations) and sports facilities were regarded as the potential location to deploy the AEDs. They have higher pedestrian flow and can reduce the consumption of space and human resources to a certain extent (Chrisinger et al., 2013). We use nearest neighbor analysis of point sets and draw thinning methods to select candidate points with different spatial densities according to accessibility levels. We constructed accessibility matrices for the candidate sites according to certain thresholds. The PuLP python library was used to conduct the linear programming to complete the site selection analysis under different coverage rules (Welscher et al., 2022). In order to verify the coverage capacity of AED sites, we calculate the percentage of the reachable area in the “golden 4-minute” and “15-minute living circle” to measure the rationality of AED siting.
3 RESULTS
3.1 Spatial distribution of myocardial infarction risk
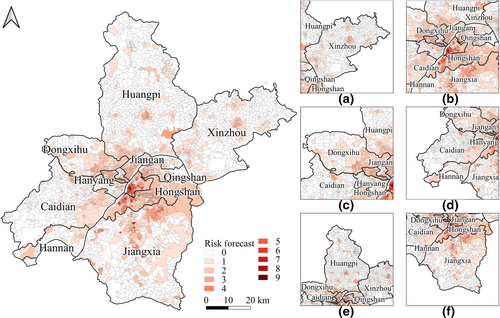
According to the spatial autocorrelation results of the risk of MI, the global Moran's I index was 0.466 (p-value<0.001), indicating a significant positive correlation (Salima & Bellefon, 2018). Meanwhile, the local Moran index was 0.307, and the high and low clustering results indicated that high-value clustering was presented in the central city of Wuhan, while low-value clustering was raised in the peripheral areas (Figure S5). This is probably due to the existence of data bias of MI patients from the hospital. Based on the original infarction risk pattern (Figure S3), we found that the risk of the disease was higher in the central urban areas of Wuhan, such as Wuchang, Jiangan, and Hanyang districts along the river. In the suburbs of Wuhan, patients in Caidian, Huangpi, and Xinzhou districts were unevenly distributed. The extremely small amount of data in the suburbs makes it challenging to uncover meaningful spatial patterns.
Risk prediction models constructed from multiple sources of spatio-temporal data can effectively reduce errors associated with a single source of MI patient data (Palaniyandi, 2012; Sahoo et al., 2016) and generate a more representative MI risk map covering more areas, which can provide a basis for accessibility assessment and AED siting. In this work, the existing patient data from Wuchang District and its surrounding communities were used as the training set to train and predict the risk of MI prevalence in other areas of Wuhan City with multiple classifications, and the results were divided into 10 levels corresponding to the community risk. As shown in Table S4, the model with the best results was LightGBM, which achieved an OA of 71.7% on the validation set and increased the number of communities covered by 24.9%. The distribution of the number of communities by risk level is shown in Figure S4. The traditional medical field roughly describes the risk of diseases as mild, severe and critical (Han et al., 2020). The community risk levels were reclassified as low (1–3), medium (4–6), and high (7–10), at which point the classification accuracy reached 82.4%. In addition, we explored the drivers of MI morbidity and mortality using regression analysis, and the results are shown in Tables S2 and S3. The results are shown in Tables S2 and S3. It can be found that patients' gender and age, traffic conditions of their residence, nighttime population density, the proportion of green in the streetscape and air pollution conditions are significantly associated with the incidence of MI.
The adjusted distribution of risk levels for MI in Wuhan is shown in Figure 2. Comparing the changes before and after the adjustment (Figure S6), 35.4% of the communities in the central city had an increased risk of MI, with an average risk increase of 1.78 in the changed areas. Five hundred twenty-five communities in the distant urban regions had their risk of MI adjusted, with 56.4% of the communities in the East–West Lake area have an increased risk of MI. These areas are primarily suburban or rural and are relatively poorly served by medical resources and transport. It has been suggested that although there is some regional variation in cardiovascular disease at the global scale (Jagannathan et al., 2019), at smaller urban scales, the morbidity pattern can be dependent on economic development and urbanization (Khan et al., 2020). This dependence also suggests that the risk of MI is closely related to urban structure. The original spatial distribution of MI risk was more concentrated and covered a smaller area, while the processed risk probability map contained a wider area, which was smoother and more uniform than the previous one. In addition, the spatial characteristics of the estimated risk in the central and distant urban areas are also more consistent with the urban structure under the strategic planning of polycentric development in Chinese mega-cities (Liu & Liu, 2018). This indicates that the risk map processed by the risk estimation model is more representative of MI incidence.
3.2 Myocardial infarction medical accessibility assessment
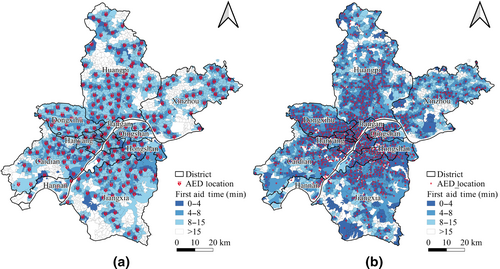
In order to analyze the community-scale accessibility of existing hospitals in Wuhan, this work evaluates the accessibility of medical service areas and MI using the shortest path method and 2SFCA, respectively, based on OSM road network and existing second- and third-degree hospitals. The community-scale accessibility results based on the most straightforward path calculation are shown in Figure 3a. When measuring the range of medical emergency services, previous scholars found that the demand for medical care within 8 km can be well met (Alhomaidhi, 2019; Asemahagn et al., 2020), and 15 km is the marginal distance for efficient emergency care (Fu et al., 2021). Therefore, we set the service radius to 8 and 15 km respectively, and evaluate the service capacity of the hospital by calculating the road network distance from the center of gravity of the community (Apparicio et al., 2017). It can be found that there are good access conditions in the central city of Wuhan (including Jiangan, Qingshan, Hanyang, Wuchang, and Hongshan Districts), while rural areas in the suburbs need to be improved.
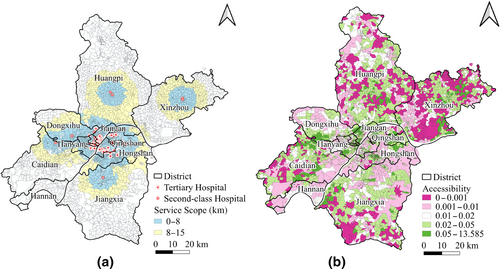
Figure 3b shows the community-scale accessibility of medical treatment based on 2SFCA, and the results are graded using the equal-quantity Method. Considering the population size, area, risk of MI, and the decayed Gaussian function, the results can better reflect the efficiency of access to medical care for MI and the imbalance of medical resources and facilities in the suburbs of Wuhan. It can help in the selection of new medical facilities.The accessibility index ranges from 0 to 13.585, with a mean value of 0.16 and a standard deviation of 0.56 (Figure S7), with larger values implying higher accessibility for MI patients (Tao et al., 2020). 13.7% of communities have above-average accessibility, while 21.9% of communities have approximately zero accessibility, reflecting the need for improvement in Wuhan's response to This reflects the need for improvement in Wuhan's response to sudden MI.
The results show that among the central urban areas of Wuhan, the university city area (central Hongshan District, etc., accessibility mean: 0.06), areas with developed industrial and energy industries (eastern Qingshan District, etc., accessibility mean: 0.05), and some tourist scenic areas (eastern Hongshan District, etc., accessibility mean: 0.006) all had the MI problem with low accessibility to medical care. The eastern part of Hanyang District and Jiangan District, where medical conditions are well developed, have high accessibility to MI (accessibility mean: 0.43). In the suburbs of Wuhan, rural and peripheral areas (southern Jiangxia and northern Huangpi districts, accessibility mean: 0.01) need to be improved.
To further analyze the mismatch pattern between healthcare accessibility and the spatial distribution of population and disease risk, we examined the spatial relationship among population, MI risk, and medical accessibility. The results are presented in Figure S8. It can be observed that issues such as uneven population distribution, relatively low first aid accessibility, and relatively high risk of disease are prevalent in the suburbs of Wuhan, particularly in parts of western Huangpi and southern Xinzhou. In the central urban area of Wuhan, characterized by relatively dense spatial population distribution, challenges such as higher risk of MI and uneven distribution of medical accessibility are evident. Findings from spatial mismatch analysis can offer more intuitive insights to facilitate decision-making regarding the macro-adjustment of AED delivery.
3.3 Siting result of AED
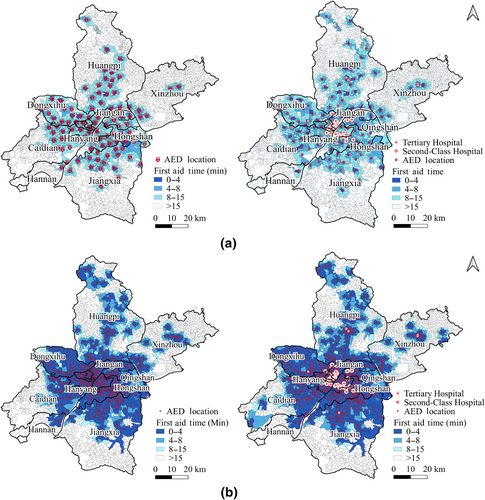
We performed the siting of the AED based on the LSCP model (Figure 4a). We chose the candidate point accessibility matrix threshold to be set at 15 min, at which point a total of 2071 candidate points were included. Of these, 203 are metro station candidates, 1292 are bus stop candidates, and 576 are sports facility candidates. The LSCP model was used to ensure that each candidate point can access at least one AED. The results included a total of 207 AED sites, with a community coverage rate of 74.0% for 15-min accessibility and 12.5% for 4 min accessibility (golden 4 min).
In order to further improve the siting of AEDs with adequate medical resources, this study extended the number of candidate sites and set the threshold of the candidate site accessibility matrix to 4 min. At this point, a total of 4741 candidate sites were included, of which 1996 were bus stops and 2543 were sports facilities. The results (Figure 4b) included a total of 1015 AED sites, whose community coverage rate of 15 min accessibility reached 96.4% and the golden 4-min emergency accessibility rate reached 55.4%.
Comparative analysis of the spatial distribution patterns between medical accessibility and medical distance before and after AED deployment can further elucidate the spatial disparities between patients and medical resources (see Figure S9). The spatial accessibility pattern, which takes into account disease risk and population distribution comprehensively, provides a more accurate assessment of the demand and supply of medical services compared to merely considering direct medical distance, especially in the suburbs of Wuhan, where a more balanced distribution is observed. A comparison reveals that the distance to medical treatment has been effectively optimized across the entire area following AED site selection and deployment.
In order to explore the service efficiency and coverage variation of the MCLP, this work fitted different numbers of AED service capacity transformation conditions. The AED service range was set to 4 and 15 min, respectively, and the candidate point coverage curves were plotted and fitted, and the results are shown in Figure S10. As the number of AEDs placed increases, the curve tends to grow slower, which means that the efficiency of AED utilization gradually decreases. The results indicate that the use of a larger area can be met with only a relatively small amount of AEDs. The inflection point of the fitted curve shows that the optimal number of AEDs to be placed is 107 for the 15-min curve and 446 for the 4-min curve, when the AED service is more efficient.
To meet the demand as much as possible with the limited number of AEDs, we further use the MCLP to locate AEDs among the candidate sites based on the MCLP coverage efficiency curve. It has been shown that AEDs within 1 km can serve the surrounding community well (Tierney et al., 2019). This work further extends the service radius to 3 km to assess its coverage efficiency. This study considers AED delivery strategies regarding accessibility to MI care, the number of candidate sites, and service areas. The comprehensive AED delivery strategies under multiple perspectives are shown in Table 1.
| Model | The number of the candidate point | Number of AED placements | 15-min accessibility coverage (%) | 4-min accessibility coverage (%) | AED service radius |
|---|---|---|---|---|---|
| LSCP | 2070 | 207 | 74.0 | 12.5 | 100% (3 km) |
| LSCP | 4741 | 1015 | 96.4 | 55.4 | 100% (1 km) |
| MCLP | 2070 | 100 | 37.9 | 6.1 | 83.1% (3 km) |
| MCLP | 2070 | 100 (consider existing hospitals) | 42.2 | 10.7 | 87.6% (3 km) |
| MCLP | 4741 | 400 | 68.3 | 38.6 | 80.7% (1 km) |
| MCLP | 4741 | 400 (consider existing hospitals) | 71.0 | 42.3 | 93.0% (1 km) |
This article further analyzes the spatial position of MCLP site selection results in Table 1. Figure 5a shows the results of sitting 100 AEDs, where the existing hospitals are not considered on the left and the existing hospitals are assessed on the right. Figure 5b shows the siting results of 400 AEDs. The results show that with the same number of AED emergency devices put in place, there is a significant increase in AED coverage when existing secondary and tertiary hospitals are considered. At this time, Wuhan's central city had high emergency MI coverage, with 100 AED stations achieving 93.6% coverage in 15 min and 400 AED stations achieving 90.8% coverage in 4 min in the central city, respectively. However, MI treatment services in marginal areas such as Jiangxia District and Huangpi District need to be improved.
4 DISCUSSION
4.1 Scientific findings
In this study, we performed siting of AED facility placement under different scenarios based on coverage models, taking into account the community-scale risk of MI onset and the accessibility of existing medical facilities. Our model predicted the OA accuracy of community risk by 71.7%, and the number of communities covered by the infarct risk map increased by 24.9%. The AED siting results showed that the best results based on the LSCP model included 1015 AED facility sites with a prime 4-min reach rate of 55.4% and a 15-min reach rate of 96.4%. Since Wuhan city has not carried out large-scale AED deployment planning before and there is a serious lack of emergency resources, the first AED distribution studies were done in this work, mainly for high-risk groups, in an effort to meet as many emergency needs as possible with cost control. In the subsequent study, we will put in new AEDs based on the first batch of AED siting results obtained from this study to improve the emergency medical system further. This work's algorithmic innovations and findings include the following four main aspects.
First, this study proposes a framework for predicting the risk of MI prevalence based on multi-source spatio-temporal data and FLAML. It can be applied to exploring spatial patterns of MI onset and analyzing the accessibility to medical care. It can be complemented with geographic regression analysis (Chang et al., 2021) and spatial cluster analysis (Soleimani & Bagheri, 2021) to provide new ideas for generating MI prevalence risk maps from a data-driven perspective. Based on the spatial distribution pattern of the risk of MI at the community scale, it is known that the risk of MI is relatively higher in the relatively developed areas of commerce, education, and tourism (Wuchang District, Hongshan District, etc.). The potential reason for this may be that economically developed urban areas have more population flow or pollution, which would increase the risk of MI among residents of these areas (Liu et al., 2022). Some studies have confirmed that both sleep quality and life stress have an impact on the development of MI (Andrechuk & Ceolim, 2015; Kivimäki & Steptoe, 2018). Meanwhile, the risk of MI is relatively lower was areas with better transportation access, better environment or better public facilities such as parks and seating (Hanyang district, Caidian district, etc.) (Nieuwenhuijsen, 2018; Yao, Yin, et al., 2022), suggesting that a good community environment will help reduce the risk of MI.
Secondly, a multi-perspective assessment of accessibility for MI patients was conducted by analyzing the current distribution of community-scale medical supplies in Wuhan, and this study explored the spatial differences in the distribution of medical resources and accessibility from two perspectives: service area and supply–demand ratio. Compared with previous studies (Lin et al., 2016; Zhang et al., 2021), the accessibility analysis in this work takes into account real factors such as population density, disease risk, and transportation network. The results show that the service area of existing medical facilities tends to expand hierarchically along the city center to the outer circle, and new medical centers are formed in the suburbs to meet urban demand. In terms of accessibility to medical care for MI, in the central city of Wuhan, the accessibility is higher with more complete municipal utilities and more dense streetscape greenery and parks (Jiangan District, etc.), which have a relatively higher standard of living and better living environment (Beauchamp et al., 2022). In contrast, in some dense areas of universities and tourist attractions (university towns, riverbanks, forest parks, etc.), there is a high population flow and a relative lack of emergency medical resources, resulting in low accessibility to MI care.
Third, this work confirms a significant association between the functional structure of the city and the accessibility to medical care for MI (Franco et al., 2015; Khan et al., 2020). Previous studies have shown a significant association between air pollutants and MI prevalence (Raziani & Raziani, 2021), and the present study quantitatively confirms this finding. Qingshan District is a major industrial area in Wuhan, and its air quality is poor due to factory processing and pollutant emissions. Industrial areas are often located in non-city center areas, which can make its accessibility to MI low and require an increase in the number of AED devices placed. In high-tech development zones (Guanggu, etc.), the wide range of areas leads to more obvious spatial differences in accessibility, with overall higher accessibility the closer to urban areas (Luo et al., 2018). The areas connecting the central city with the suburbs (eastern Hongshan District, etc.) are exceptionally densely populated, with traffic congestion and slower travel, making emergency accessibility lower. Under the strategic plan of megacity polycentric development in China, the new urban centers formed in the suburbs (central Huangpi District, etc.) have relatively well-developed transportation road networks and medical resources, and have higher accessibility to MI (Liu & Liu, 2018). In addition, the climatic environment, especially extreme weather, can significantly impact cardiovascular disease occurrence (Kienbacher et al., 2021). In rural and marginal urban areas, poor allocation of health resources and insufficient capacity to cope with weather extremes contribute to their low accessibility to MI (Wang, Chai, et al., 2021).
Fourth, this study discusses AED siting in multiple scenarios from the perspective of accessibility to MI and in conjunction with LSCP model. Compared with AED siting based on OHCA data (Moon et al., 2015) or mathematical optimization methods (Sun et al., 2020), this work takes into account the existing medical resources and urban layout characteristics more comprehensively, and can better meet the demand for new AED siting in cities. According to the AED siting results of the LSCP model, it can be found that the overall distribution of new AEDs is more uniform, which can effectively cope with the uneven spatial distribution of AEDs. The number of new AED devices is also higher in areas with high population density and more high-rise buildings (Wuchang District, Jiangan District, etc.). At the same time, in the suburbs of Wuhan City, where medical resources are relatively lacking, tourist attractions with high population flow and some areas where universities are located also need more AED devices. The north and south ends of Wuhan City are located in lakes or rural areas, there is a certain lack of AED deployment problem.
Our results show that deploying a relatively small number of AED devices according to the MCLP model can meet the medical demand in central urban areas well. The site selection results based on MCLP show that without considering existing hospitals, there are relatively more new AEDs in university cities, tourist attractions, and along-river areas (Hongshan District, Wuchang District, etc.), and the site locations partially overlap with existing hospitals, which further illustrates the rationality of making full use of existing hospitals to improve the efficiency of MI emergency. The coverage capacity of AEDs has been significantly improved by considering the existing second- or third-degree hospitals, and the new AED devices show a trend of spreading to the edge. With the deployment of 100 AED stations, the 15-min coverage rate in the central city of Wuhan reached 93.6%. Some studies have shown that the effective coverage of mobile AED sites is about three times that of fixed AEDs (Hajari et al., 2020; Kinoshi et al., 2018), so with limited resources, using public transportation or drones to carry a relatively small number of mobile AED devices can largely reduce human and material resource overhead and simultaneously better meet the need for emergency care (Bhatt et al., 2018; Ślęzak et al., 2021). Comparing the siting results in this work, it can also be found that AEDs based on the LSCP model have a high service capacity in both central and distant urban areas, but require a high number of AEDs. In contrast, the AEDs based on the MCLP model have a dense distribution and high coverage in central urban areas, but unbalanced coverage of suburban areas. Therefore, to address the shortage of emergency medical resources in Chinese cities, the MCLP model and the LSCP model can be used to deploy both fixed AEDs and mobile AEDs to respond to sudden MI, in order to meet as many emergency needs as possible with limited AED resources.
4.2 Policy implications
- Improve the data completeness of hospitals in remote areas. Analysis of the myocardial infarction risk prediction results at the community level reveals a concentration of existing patient data in central urban areas, with limited data from patient visits in remote regions. The State Council of China has advocated for the creation of a national medical and health information hierarchical open application platform to facilitate cross-regional sharing and integration of foundational data (General Office of the State Council, 2016). Therefore, it is imperative to enhance attention to remote areas by conducting visiting surveys or establishing a unified hospital data service platform.
- Focus on the unbalanced distribution of emergency medical resources in rural areas. The limitations of transportation conditions and the current unbalanced distribution of medical resources in rural areas between urban and suburban areas have led to significant shortcomings in their response to sudden MI. Some policies indicate that there are gaps in medical services in China at both the social and regional levels (The Xinhua News Agency, 2021). Therefore, the development mode needs to shift from scale expansion to improving quality and efficiency. So balancing the distribution of medical resources between urban and suburban areas and improving the level of emergency medical care in rural areas are of great significance to high-quality medical and health development, especially the construction of rural China.
- The deployment of new AED devices should be prioritized in tourist attractions as well as commercial and educationally developed areas. In these areas, where the population flow is high and emergency medical resources are relatively scarce, the risk of MI is high and the accessibility of medical treatment is low. The National Health Commission of China points out that in the process of constructing the pre-hospital emergency medical care network, it is necessary to improve the level of AED deployment to promote the integrated development of urban and rural emergency medical care systems and regional balance (Chinese Medical Career Development Center, 2020). So this work suggests that the focus should be on strengthening the emergency medical system in these areas to ensure the efficiency of treatment for sudden-onset diseases.
4.3 Limitations and future works
There are still some unresolved issues in this study. First, in the study of the spatial distribution pattern of the risk of MI, we could not use out-of-hospital cardiac arrest (OHCA) data to assist in the generation of MI risk maps due to difficulties in data acquisition. Second, in the study on the accessibility of medical facility layout and the siting of AED delivery, the selection of candidate sites in rural areas was deficient. Third, since AEDs in public places are influenced by the opening hours of the areas where they are located, taking into account the effects of time constraints and utilization efficiency constraints in the process of AED delivery is also a direction that needs to be improved in the future. In future studies, we will expand the data sources of MI patients and combine OHCA data to better fit the risk of MI. It is also necessary to consider the spatial and temporal differences in the utilization efficiency of AEDs at different locations to constrain their optimal site selection in order to obtain better site planning recommendations.
5 CONCLUSION
Dealing with the severe shortage of AEDs in China's megacities, this study examines the siting of AEDs from multiple perspectives, based on an assessment of the risk of MI and accessibility to medical care. Regarding the risk of MI, Wuhan shows a spatial distribution pattern of high internal and low external risk. The risk of MI is relatively low in areas with convenient transportation, good public facilities and beautiful environments. In contrast, the risk of MI is higher in areas with higher noise levels or poorer environments. In terms of accessibility to MI care, accessibility is lower in areas with more developed business and education, higher population density or more severe air pollution, and needs to be improved. In terms of AED locations, priority should be given to tourist attractions and commercial and educational areas, and focusing on the imbalance in the distribution of emergency medical resources in rural areas. The LSCP model based on accessibility can well meet the needs of urban public health development. Given the limited resources available, the MCLP model can be used to deploy mobile AEDs which have about 15-min service range to achieve a coverage rate of 93.6% in central urban areas with only 100 AED stations, which can meet the medical needs of the city. In order to improve the emergency medical system in the urban development process and increase the efficiency of MI treatment, it is necessary to increase the number of AEDs deployed, raise the level of social awareness, and target the placement of AEDs in areas with high population flow and low accessibility to MI treatment.
ACKNOWLEDGMENTS
We would like to thank the editors and anonymous reviewers for their constructive suggestions and comments for improving this manuscript. Open Access funding enabled and organized by Projekt DEAL.
CONFLICT OF INTEREST STATEMENT
No conflict of interest exists in this article, and the article was approved by all authors for publication.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.