Congenital Abnormality of the Vagina Complicated by Haemato-Pyocolpos in a 1-Year Labrador Retriever
Contents
A 1-year-old female Labrador retriever was referred with a few days history of haematic-like vulvar discharge. Physical examination, vaginal inspection and palpation did not reveal any remarkable finding. Transabdominal ultrasound showed echogenic fluid accumulation in the vagina suggesting haemato-pyocolpos. An exploratory laparotomy was performed: a well-delimited ectasic vagina was identified. Ovariohysterectomy and partial vaginectomy and vaginoplasty were performed to spay the bitch and to remove the ectasic vagina. Post-operative recovery and 12-month follow-up were uneventful. Clinical, morphological and histological findings were consistent with a congenital abnormality of the muscular layer of the vagina complicated by haemato-pyocolpos. The disorganization of the vaginal tunica muscularis may have acted as locus minoris resistentiae in the vaginal wall. The organ was dilated and atonic due to the gradual accumulation of physiological fluids complicated by an overgrowth of genital bacteria. This congenital disorder has to be taken into account as differential diagnosis of haemato-pyocolpos with vaginal discharge in young bitches.
Introduction
Disorders of the ontogenic differentiation of the foetal reproductive system result in several forms of congenital abnormalities. Among those affecting the vagina, septa, strictures and segmental aplasia have been documented (Root Kustritz et al. 1995; Johnston et al. 2001a; England 2009). The true incidence is unknown, but septa and strictures are the most commonly reported in the bitch (Purswell 2003).
These disorders can be asymptomatic, but depending on the severity of the abnormalities, difficult mating and delivery, and recurrent vaginitis may occur.
Partial obstructions can result in an oestrous bitch experiencing pain and refusing mating and, in cases where conception is achieved by artificial insemination, abnormalities in the vagina can lead to dystocia (Johnston et al. 2001b).
Furthermore, the defective canalization might impair the normal flow of physiological fluids that can be retained in the vagina becoming a substrate for bacterial growth. Thus, a vaginal accumulation of the physiological secretions, prooestrous fluids or urine is often involved in the pathogenesis of recurrent vaginitis.
The present report describes a clinical case of a congenital abnormality of the vagina complicated by haemato-pyocolpos in a 1-year-old Labrador retriever and discusses its clinical and pathological features.
Case Report
A 1-year-old female Labrador retriever (28 kg bodyweight) was referred with a few days history of haematic-like vulvar discharge, an occasional episode of vomiting the day before, overall good appetite, but slight general dullness. The bitch was presented to the Department, and a complete physical examination, serum haematology, biochemistry and instrumental examinations were performed.
Upon presentation, the dog was quiet, but alert and responsive, with a good body condition score. Mucosal membranes were pink, capillary refill time was 2 s, and peripheral pulses were good. Rectal temperature was 39°C, heart rate was 116 beats/min, and respiration rate was 36 breaths/min. The physical examination did not reveal any anomaly other than the vulvar discharge.
The deep abdominal palpation revealed a mass consistent (approximately 10 cm) with a fluid accumulation dorsal to the bladder and determined a further evacuation of serosanguineous fluid from the vulva. A vaginal swab was performed for microbiological evaluation. The vaginal inspection and palpation did not reveal any remarkable finding. Transabdominal ultrasound (Medison SonoAce 8000; Medison Co. Ltd., Seoul, Korea) showed hyperechogenic accumulation of fluid in the cranial vagina suggesting haemato-pyocolpos.
The vaginal smear revealed a late prooestrous/early oestrous phase of the cycle with a high number of red blood cells and superficial cells from the stratified squamous epithelium, such as anuclear cells, cells with pycnotic nuclei and large intermediate cells. Haematology and serum biochemistry profiles were within the normal ranges.
Based on the investigational findings, an exploratory laparotomy was performed. The dog was pre-medicated with acepromazine (0.01 mg/kg) by subcutaneous injection and methadone 0.2 mg/kg intravenously. General anaesthesia was induced with propofol (4 mg/kg IV) and maintained with 2% isoflurane administered in 100% oxygen via an 11.0-mm endotracheal tube. Cephazolin (22 mg/kg) was given IV following induction. Fluid therapy was administered during the surgical procedure (NaCl 0.9%, 10 ml/kg/h).
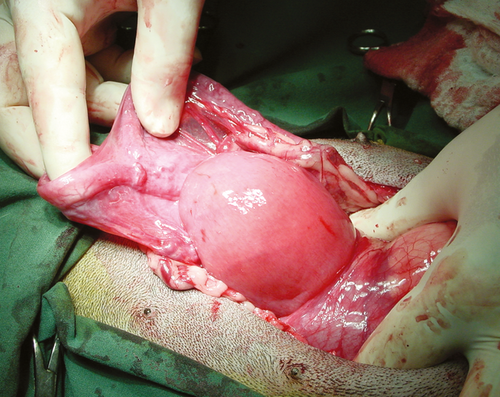
After routine preparation for an exploratory laparotomy, the bitch was placed in dorsal recumbency and a 10F urinary catheter was inserted to drain the urine and identify the urethra. During exploratory laparotomy, the ectasic cranial vagina was identified (Fig. 1). The accumulation appeared to be cranially well delimited, but adhesions on the bladder and on the ureters were present.
A free-hand aspiration of the lesion was performed with a 21-gauge needle to collect 5 ml of the contained fluid for microbiological evaluation.
An ovariohysterectomy and a partial vaginectomy and vaginoplasty were performed to spay the bitch and remove the ectasic vagina. Vaginal mucosa was apposed with a 2-0 polyglactin 910 (Vycril; Ethicon, Somerville, NJ, USA) using continuous pattern absorbable suture. The muscular layer was sutured with a continuous pattern using 3-0 polyglactin 910. Subcutaneous layer was closed with continuous pattern using 3-0 polydioxanone (PDSII; Ethicon) and a simple, interrupted non-absorbable suture 2-0 polyamide (Ethilon; Ethicon) was used to close the cutaneous wound. Post-operative recovery was uneventful and the dog was discharged with a prescription of cephalexin (30 mg/kg bid PO), tranexamic acid (15 mg/kg sid SC) and an Elizabethan collar.
A bacteriologic examination revealed a severe presence (>103 CFU) of Pasteurella Multocida in vaginal swabs performed before the surgery and in the fluid collected intra-operatively.
The antibiotic sensitivity test (Table 1) revealed the sensitivity of bacteria to Marbofloxacin that was prescribed (2 mg/kg sid PO) 3 days post-surgery for 14 days.
| Amoxicillin | Resistant |
| Amoxicillin + Clavulanic Acid | Resistant |
| Cephalexin | Intermediate |
| Ceftriaxone | Susceptible |
| Clindamicin | Resistant |
| Doxycycline | Resistant |
| Enrofloxacin | Intermediate |
| Kanamicin | Intermediate |
| Marbofloxacin | Susceptible |
The genital tract was evaluated grossly and histologically as described below.
Follow-up
Vaginal discharge disappeared few days after the surgery. Ten days later, wound healing was satisfactory. One month after surgery, cranial vaginal swabs were sterile. Twelve months after surgery, the dog's general condition was good and no vaginal discharge was present.
Pathology
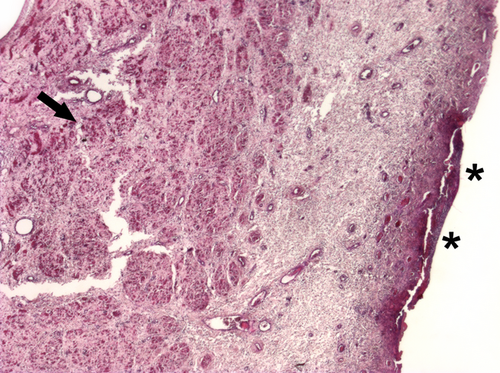
Grossly, on morphological examination, no ovarian abnormalities, while slight purulent accumulation in the uterus and a multifocally ulcerated mucosa of the vaginal dilatation, were observed. Fixed samples were routinary processed for histology and paraffin embedded. Section, 5 μm thick were obtained and stained with haematoxylin and eosin.
On histological examination, follicles at various stages of development, follicular cysts and other cysts filled by blood and lined by hyperplastic granulosa cells were identified in the ovarian tissue.
A slight purulent widespread endometritis was present, and the vaginal ectasia was characterized by an irregular muscular wall mixed with oedematous connective tissue. The mucosal epithelium was multifocally ulcerated, characterized by vascular damage (thrombi) and an active chronic purulent inflammation (Fig. 2).
Discussion
Clinical, morphological and histological findings were consistent with a congenital abnormality of the muscle layer in the cranial vagina that was completely disorganized and replaced by an irregular muscular wall mixed with oedematous loose connective tissue.
Most likely, this defect acted as a locus minoris resistentiae of the vaginal wall, and the organ was dilated and atonic due to the gradual accumulation of prooestrous bleeding. A subsequent overgrowth of genital bacteria resulted in haemato-pyocolpos.
Some studies described obstructive vaginal disorders (i.e. segmental aplasia, imperforate hymen) with accumulation of fluids in newborns or during puberty, both in women and in bitches, with a concurrent acquired inflammation resulting in hydro-haemato-pyocolpos (Wadsworth et al. 1978; Brevetti et al. 1997; Tseng et al. 2008; Ercan et al. 2011; Marinho et al. 2013).
In the present clinical case, congenital defective canalization of the vagina was not observed, and the histological findings suggest that ulcerative purulent inflammation was secondary to bacterial contamination of the fluid accumulation. Histologically, vaginal ectasia was characterized by an irregular muscular fibres intermingled with connective. The disorganization of the muscle layer of the cranial part of the vagina can be explained with the organogenesis during the foetal life. The cranial vagina develops from the paramesonephric ducts, whereas the urogenital sinus participates in the development of the caudal vagina (Constantinescu 2007). Furthermore, the vaginal layers derive from different structures, for instance, the muscle layer from the mesenchymal sheath, whereas the mucosal epithelium from the utero-vaginal canal (Tuchmann-Duplessis 1971). Therefore, the possibility that a single layer was affected by a congenital defect is sustainable and it has to be taken into account as differential diagnosis of haemato-pyocolpos with vaginal discharge in young bitches.
Surgery represents the gold standard treatment and vaginoplasty with or without ovariohysterectomy should be planned based on disorder severity (Moxon and England 2011).
In clinical practice, an early diagnosis of congenital abnormalities is recommended. A delayed diagnosis may result in severe consequences as haemato-pyocolpos complicated by uterine disorders, pelvic infection, adhesions and compromised reproductive performances.
Congenital abnormalities of the vagina are not frequently investigated in routine clinical veterinary care. Practitioners should perform a complete genital examination when the bitch is clinically examined for the first time and they should carefully investigate the history to evaluate a possible familiar pre-disposition to genital defects.
Acknowledgements
The authors thank Mr. M. Colombo for photographic support.
Conflict of interest
None of the authors have any conflict of interest to declare.
Author contributions
SA and GCL performed the examination of the clinical case and contributed to draft the article. Surgical procedure was carried out by SA, SR and GCL. Histological examination was performed by VG.