Machine Learning for Predicting Waitlist Mortality in Pediatric Heart Transplantation
Funding: This work was supported by the Jefferson Trust and AHRQ grant 1R21HS029548-01A1.
ABSTRACT
Background
Waitlist mortality remains a critical issue for pediatric heart transplant (HTx) candidates, particularly for candidates with congenital heart disease. Listing center organ offer acceptance practices have been identified as a factor influencing waitlist outcomes. We utilized machine learning (ML) to identify factors associated with waitlist mortality, combining variables associated with institutional offer acceptance practices as well as candidate-specific risk factors.
Methods
We analyzed the Organ Procurement and Transplantation Network database for pediatric HTx candidates listed between 2010 and 2020. Various statistical and ML models were employed to identify predictors of waitlist mortality or clinical deterioration leading to waitlist removal. The dataset was split into training (82%) and testing (18%), and the final model was selected based on predictive performance. SHAP values were used to assess variable importance.
Results
Among 5523 pediatric candidates, overall waitlist mortality was 9.8%. The CatBoost model achieved the highest predictive performance with an AUC-ROC score of 0.74 and a recall score of 0.75. Key predictors included candidate diagnosis, age/size, ventilator use, eGFR, serum albumin, ECMO, and institutional factors such as high offer refusal rates and low transplant volume.
Conclusions
Institutional organ offer acceptance practices influence waitlist outcomes for pediatric HTx candidates. Centers with higher organ refusal rates are associated with worse outcomes, independent of candidate-specific risk factors, underscoring the need for standardizing organ acceptance criteria across institutions to reduce variability in decision-making and improve waitlist survival. Additionally, addressing modifiable risk factors such as malnutrition and renal dysfunction could further optimize patient outcomes.
Abbreviations
-
- AUC-ROC
-
- area under the receiver operating characteristic curve
-
- eGFR
-
- estimated glomerular filtration rate
-
- GAM
-
- generalized additive model
-
- HRSA
-
- health resources and services administration
-
- ML
-
- machine learning
-
- OPTN
-
- organ procurement and transplant network
-
- UNOS
-
- united network of organ sharing
-
- VAD
-
- ventricular assist device
1 Introduction
Waitlist mortality and clinical deterioration remain significant challenges for pediatric patients awaiting heart transplantation. Over the past two decades, several medical and bioengineering breakthroughs, including the utilization of ABO-incompatible allografts, improved mechanical circulatory support devices, and enhanced alloantibody desensitization modalities, among others, have improved waitlist survival [1-3]. Despite these advances, waitlist mortality or clinical deterioration resulting in waitlist removal for pediatric patients in the United States remains around 12%, and is over 20% for those with congenital heart disease [4-6]. A recent Organ Procurement and Transplantation Network (OPTN) report identified candidates < 1 year old who remain at highest risk for waitlist mortality, and the proportion of transplant candidates with congenital heart disease has increased nearly 20% over the last decade, now comprising 64% of all pediatric candidates [4].
The disparity between the number of pediatric heart transplant candidates and available donors is a major contributor to waitlist mortality, resulting in prolonged waitlist times for these critically ill patients. Remarkably, 39% of pediatric donor hearts are not utilized by pediatric candidates, despite 63% of these donors having normal echocardiograms [7]. Institutional offer acceptance practices, including an institution's prior year offer acceptance rate, appear to have an undue influence on organ offer decisions, likely contributing to longer waitlist times for candidates at institutions with higher offer refusal rates [7, 8]. This is supported by a recent OPTN database analysis which showed institutions with higher offer refusal rates had longer candidate waitlist times, as well as higher rates of waitlist removal for candidate mortality or clinical deterioration [9]. Previous studies have employed various statistical techniques to characterize waitlist mortality in this population, but none have incorporated both candidate variables and variables associated with listing center offer acceptance practices [3, 9-11].
Machine learning (ML) is an innovative modeling approach that offers enhanced predictive capabilities due to its robust handling of categorical variables, improved management of multiple interactive variables, and non-linear relationships [12]. In this study, we applied ML to analyze the OPTN database to better characterize factors associated with waitlist mortality or clinical deterioration resulting in waitlist removal among pediatric candidates awaiting heart transplantation. We included several variables related to listing center offer acceptance practices to assess their contribution to this outcome. Understanding these factors has the potential to improve waitlist outcomes in this vulnerable population by influencing institutional practices and expediting revision of the current OPTN pediatric heart allocation policies, which do not adequately capture candidate risk profiles [11].
2 Methods
2.1 Data Source
In this retrospective study, we used data from the OPTN. The OPTN data system includes data on all donors, waitlisted candidates, and transplant recipients in the US, submitted by the members of the OPTN. The Health Resources and Services Administration (HRSA), US Department of Health and Human Services, provides oversight to the activities of the OPTN contractor. The data reported here have been supplied by the United Network of Organ Sharing (UNOS) as the contractor for OPTN. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy of or interpretation by the OPTN or the US Government. This study was approved by the institutional review board of the University of Virginia.
2.2 Study Population
The OPTN database was queried for all pediatric (< 18 years) heart transplant candidates listed between January 1, 2010 and December 31, 2020. Candidates with a prior heart transplant, transferred to another center, listed in error, remained on the waitlist at the time of data collection, or with an unknown waitlist outcome were excluded. For candidates who were added to the waitlist multiple times during this period, only the initial listing period was included for analysis.
2.3 Data Collection
Prior to modeling, 42 candidate-specific variables at the time of waitlist registration were selected from the OPTN dataset based on a review of existing literature and clinical expertise (Data S1). Estimated glomerular filtration rate (eGFR) was calculated for each candidate using the Schwartz formula. Listing center code was included as a variable in the model to assess whether this influences the model's predictive ability. Three additional listing center variables were derived from the dataset through feature engineering: listing center transplant volume (number of pediatric heart transplants each listing center performed the previous year), median number of offer refusals per candidate at each listing center, and the overall proportion of offers refused at each listing center for all candidates during this period. We included listing year as well as the implementation date of the most recent pediatric heart allocation policy change (July 7, 2016) to assess whether they influence the model's predictive ability.
2.4 Statistical Analysis/Machine Learning Modeling
A comparative analysis of baseline demographics was made between groups. Categorical variables were compared using Chi-squared or Fisher's exact tests. Continuous variables were compared using the Wilcoxon rank-sum test. Several statistical and machine learning models were compared for overall performance using Area Under the Receiver Operating Characteristic Curve (AUC-ROC) as the evaluation metric. Models assessed include Lasso (logistic regression with Lasso penalty), generalized additive model (GAM), XGBoost, Random Forests, and CatBoost.
Further analysis was conducted to characterize variables most predictive of waitlist mortality or clinical deterioration resulting in waitlist removal. We utilized a binary classification model with CatBoost due to its improved predictive ability compared to the other models tested, as well as its improved handling of categorical variables [12]. The total population was split into training (n = 4523) and testing (n = 1000) data sets. We used the Python Optuna package [13] to optimize and select the best parameters using the training data. Optuna uses Bayesian optimization to search for the parameters that provide the best cross-validated predictive performance. Based on Optuna's tuning, the final model contained: depth 3 trees, 223 iterations, learning rate 0.04, and ridge regularization 11.95. We fit the final model using all the training data with Optuna's selected parameters and used the test data to calculate variable importance scores via SHAP values [14]. The SHAP importance scores indicate which variables have the most influence in and association for predicting the outcome (i.e., waitlist mortality or removal for clinical deterioration). The complete code for the final model, along with a detailed modeling report following the TRIPOD+AI checklist [15], is available in the Data S1.
3 Results
There were 5523 patients in this cohort, with an overall waitlist mortality of 9.8% as shown in Table 1. Patients who were successfully transplanted were older and more likely to have been supported with a ventricular assist device (VAD) at listing. By comparison, those who did not survive to transplantation were more likely to have renal insufficiency, require dialysis, mechanical ventilation, or ECMO, and were more likely to be blood Type O.
| Transplanted (n = 4983) | Waitlist mortality/deterioration (N = 540) | p | |
|---|---|---|---|
| Gender (% Female) | 44.1% | 43.1% | 0.709 |
| Age (years) | 4.0 [0.0, 10.5] | 0.0 [0.0, 1.6] | < 0.001 |
| Weight (kg) | 15.0 [0.0, 33.5] | 7.6 [2.4, 12.7] | < 0.001 |
| Height (cm) | 99.0 [55.0, 143.0] | 67.0 [45.6, 88.4] | < 0.001 |
| BMI (kg/m2) | 16.2 [13.7, 18.6] | 15.4 [13.6, 17.2] | < 0.001 |
| Blood Type A | 36.0% | 33.9% | 0.345 |
| Blood Type B | 13.6% | 11.5% | 0.190 |
| Blood Type AB | 4.1% | 2.2% | 0.042 |
| Blood Type O | 46.2% | 52.4% | 0.007 |
| Race White | 53.0% | 50.4% | 0.268 |
| Race Black | 20.0% | 23.0% | 0.123 |
| Race Other | 3.1% | 3.0% | 1.000 |
| VAD % | 13.3% | 8.5% | 0.002 |
| eGFR (mL/min/1.73 m2) | 96.1 [72.3, 120.0] | 82.2 [54.2, 110.2] | < 0.001 |
| Albumin (g/dL) | 3.6 [3.1, 4.1] | 3.3 [2.8, 3.8] | < 0.001 |
| Dialysis % | 1.2% | 4.8% | < 0.001 |
| Ventilator % | 15.8% | 35.0% | < 0.001 |
| ECMO % | 4.6% | 14.6% | < 0.001 |
- Note: Categorical variables reported as frequency (percentage). Continuous variables reported as median and interquartile range.
The five statistical and machine learning models were evaluated based on accuracy performance. CatBoost, XGBoost, and GAM demonstrated the highest performance, achieving AUC-ROC scores between 0.73 and 0.74. For further analysis, we selected the CatBoost model due to its AUC-ROC of 0.74 (95% CI 0.69–0.79) and high Recall score (sensitivity or true positive rate) of 0.75 (95% CI 0.60–0.78), indicating that it correctly identified 75% of cases where patients experienced waitlist mortality or were removed due to clinical deterioration.
Figure 1a illustrates the top 19 variables most influential in predicting waitlist mortality or removal for clinical deterioration using the CatBoost model. Candidate diagnosis of dilated cardiomyopathy was the most important variable in the model for predicting waitlist outcome, followed by candidate height and candidate diagnosis of congenital heart disease with prior cardiac surgery. As shown in the Beeswarm plot (Figure 1b), congenital heart disease with prior cardiac surgery is strongly associated with negative waitlist outcomes, whereas candidate diagnosis of dilated cardiomyopathy is a strong predictor of waitlist survival.
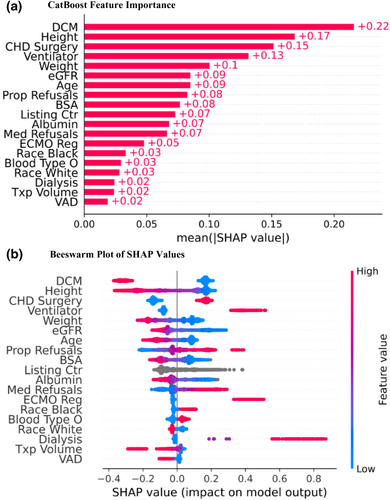
Candidate factors related to age and size were important variables identified by the model, with lower values for each of these variables predicting a negative waitlist outcome. Furthermore, candidate ventilator use, lower eGFR, lower serum albumin level, use of extracorporeal membrane oxygenation (ECMO), and dialysis were all associated with increased risk. Notably, candidate use of a ventilator, ECMO, and dialysis was very strongly associated with waitlist mortality/deterioration with very high SHAP values (Figure 1b). Demographic factors including African American race and blood Type O were also associated with higher mortality/deterioration risk. Figure 2 displays various partial dependency plots for continuous and ordinal variables to demonstrate the association between variable values and predicted waitlist outcome.

In addition to candidate-specific factors, the model identified two listing center-related variables as among the most important predictors: the overall proportion of offers refused at each listing center for all candidates during this period and the median number of offer refusals per candidate. In both instances, higher values were associated with worse waitlist outcomes. Furthermore, the previous year's heart transplant volume at listing centers also influenced the model, with lower transplant volumes correlating with worse waitlist outcomes.
4 Discussion
4.1 Listing Center Impact on Waitlist Mortality
Several studies have previously shown an association between candidate risk factors and waitlist mortality for pediatric patients awaiting heart transplantation [2, 3, 6, 10, 11], and others have highlighted the role listing center offer acceptance practice plays in waitlist outcomes [9, 16]. To our knowledge, this is the first study combining these potential risk factors to assess their relative impact on waitlist mortality or removal for clinical deterioration.
In a single center retrospective analysis, Hernandez et al. [16]. demonstrated that implementing institutional donor acceptance guidelines significantly reduced waitlist time, offer refusals for hearts with normal ejection fraction, and overall offer refusal rates, while also showing a trend toward decreased waitlist mortality or deterioration. In their subsequent analysis of the OPTN database, they showed that listing centers with high organ offer refusal rates had longer waitlist times, higher rates of death or deterioration, and were less likely to transplant candidates compared to centers with lower offer refusal rates [9]. Additionally, Rana et al. [17]. found that patients listed in low volume transplant centers (less than 3 transplants per year) had a significantly higher rate of waitlist mortality compared to those at high volume centers (more than 10 transplants per year).
Similarly, our study demonstrated that listing center offer acceptance rate is a strong predictor of waitlist outcomes, even when accounting for candidate risk variables. Listing center variables were among the most predictive variables along with established risk factors such as diagnosis, age/size, and end-organ dysfunction. Consistent with previous findings, our results indicate that a higher number of offer refusals per candidate, a greater proportion of offer refusals at a listing center for all candidates, and low transplant volume are associated with worse waitlist outcomes. Our group previously reported that organ acceptance is influenced by the listing center receiving the offer and the number of times the offer has been refused by other institutions [7, 8]. This current study suggests that variable organ acceptance practice among listing centers is associated with waitlist mortality, even when accounting for candidate specific risk factors. Considering the number of times a heart offer is refused for donor quality is not associated with post-transplant outcomes [18], these findings highlight a critical opportunity for improving offer acceptance practices within the transplant community in order to increase organ utilization and decrease waitlist mortality.
4.2 Modifiable Risk Factors
Management of pediatric patients with end-stage heart failure refractory to guideline-directed medical therapy is aimed at achieving the highest probability of long-term survival. Clinicians are often confronted with the difficult task of determining the optimal timing of waitlist activation once all medical and surgical options are exhausted, balancing the risk of delayed listing, which may contribute to negative outcomes. Once a patient is listed for transplantation, there remains a role for further risk reduction by optimizing candidate risk factors.
In an analysis of the OPTN database utilizing machine learning to assess variables associated with waitlist mortality in adult candidates, Hsich et al. [19]. demonstrated low serum albumin level and eGFR to be strongly associated with waitlist mortality. Similarly, our results show modifiable risk factors such as malnutrition (low serum albumin, lower body mass index) and renal dysfunction (low eGFR, need for dialysis) are important predictors of waitlist mortality in the pediatric population. This emphasizes the importance of optimizing fragile patients through targeted interventions, including ventricular assist devices, which have been shown to improve functional status [20], nutritional status [21], and waitlist outcomes in select populations, especially if waitlist duration is expected to be prolonged [2, 22-24].
Unfortunately, as shown in previous studies, our model identified African American race to be predictive of poor waitlist outcomes, whereas white race was associated with positive outcomes—underscoring the continuing health disparities that exist in this population of patients.
4.3 Organ Allocation Policy
The current OPTN pediatric heart allocation policy introduced in 2016 aimed to reduce waitlist mortality by prioritizing patients with the highest clinical acuity based on previously identified risk factors [25]. These policy changes reduced urgency status for dilated cardiomyopathy patients on inotropic support, whereas congenital heart disease patients on inotropic support remained at the highest urgency status. Additionally, it removed primary allocation by blood type for ABO incompatible listings to reduce wait times for infants. However, this policy still only stratifies patients into three tiers (Status 1A, Status 1B, Status 2), with the opportunity to submit an exception request for higher acuity listing.
Listing status was not included as a variable in our model in order to exclusively test the relationship between candidate/listing center risk variables to waitlist outcome. However, our modeling did not identify candidate listing year or listing prior to vs. after the policy change as correlates to waitlist outcome (Figure 2). Power et al. [11]. recently showed the ongoing limitations of the allocation policy, which fails to adequately capture the mortality risk for patients within the same listing status group and even between listing status groups. Our results highlight the interplay of multiple candidate variables, each contributing varying degrees of risk. This supports a revision of the current allocation policy to one that allows for a more granular assessment of waitlist mortality risk, such as would be found in a continuous distribution system.
5 Limitations
This study has limitations inherent to retrospective database analyses, including the potential for missing or inaccurate data, which will impact the accuracy of predictive modeling. Although our model demonstrated good accuracy, its predictive power could be improved by including additional clinically relevant data such as patient functional status, human leukocyte antigen sensitization, and cardiac biomarkers, which are either missing or incomplete in the OPTN/UNOS database. In addition, since data was collected at the time of candidate waitlist registration, any changes occurring during the waitlist period are not captured. Finally, although the model can identify the relative impact of variables on the predicted outcome, modeling results are not meant to be interpreted as being causal.
6 Conclusion
Despite a considerable reduction in waitlist mortality for pediatric patients awaiting heart transplantation over the last several decades, it remains unacceptably high. Listing center offer acceptance practice appears to be a key factor contributing to this issue. Although the reason for this is multifactorial, a standardization for organ acceptability criteria, as proposed by the 2020 International Heart and Lung Transplantation consensus statement [26], could have a beneficial impact. Moreover, addressing modifiable risk factors before listing through targeted interventions could enhance waitlist survival rates and potentially improve post-transplant outcomes. Future research should focus on developing a more robust model incorporating additional relevant data, as well as a comprehensive risk calculator that integrates the diverse risk factors affecting waitlist mortality. Such a tool could inform more effective organ allocation criteria, ultimately improving outcomes for pediatric heart transplant candidates.
Acknowledgments
Research reported in this publication was supported in part by the Jefferson Trust and AHRQ grant 1R21HS029548-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.