Comparison of Cervical Sagittal Parameters among Patients with Neck Pain and Patients with Cervical Spondylotic Radiculopathy and Cervical Spondylotic Myelopathy
Tao Liu and Shuo Tian contributed equally to this study.
Abstract
Objective
Previous studies have shown that cervical sagittal alignment is strongly associated with cervical deformity, myelopathy, and cervical adjacent-segmental disease, and these cervical sagittal parameters are correlated with health-related quality of life. However, less attention has been paid to cervical sagittal balance in various cervical disorders. This study aimed to compare cervical sagittal parameters between patients with nonspecific neck pain (NS-NP) and patients with cervical spondylotic radiculopathy (CSR) and cervical spondylotic myelopathy (CSM).
Methods
We retrospectively examined 236 patients from between January 2020 and October 2022. We divided them into three groups (NS-NP, CSR, and CSM) and collected general information and cervical sagittal parameters for these patients. The variation of parameters between the size of these parameters and gender differences was analyzed. Pearson's or Spearman's correlation was applied to analyze the association of cervical sagittal parameters of all patients between the three groups.
Results
There were significant differences in age and sex among the three groups (p < 0.001), with the NS-NP group being the youngest and NS-NP being more common in women. The parameters of cervical sagittal position significantly differed among the three groups (p < 0.05). Pearson's or Spearman's correlation result showed that the C2–C7 Cobb angle was negatively associated with the C2–C7 sagittal vertical angle (SVA), and the C2–C7 Cobb angle and T1 slope (T1s) were negatively associated with the spino-cranial angle (SCA). There was a positive correlation between the C2–C7 Cobb angle and C7 slope (C7s), C2–C7 SVA and T1s, C2–C7 SVA and SCA, and C7s and T1s.
Conclusion
This study showed that between the three groups, patients with nonspecific neck pain had smaller SCA, and among patients with NS-NP, women had more significant SCA. The smaller anteroposterior diameter of the thorax in women might explain this difference.
Introduction
Common causes of neck pain include neurogenic cervical spondylosis and spinal cord cervical spondylosis.1 Previous studies have reported a close association between cervical sagittal alignment and cervical spine disease. Sagittal alignment and balance of the cervical spine, including the cervical Cobb angle, the sagittal vertical axis (SVA), and a series of parameters at the cervico–thoracic junction, maintain cervical sagittal balance and are important indicators for evaluating cervical degeneration and cervical spine stability.2-4 Therefore, analysis of cervical sagittal parameters is essential to assess cervical sagittal balance and predict clinical outcomes.
Nonspecific neck pain (NS-NP) refers to neck pain (with or without radiation) without evidence of a specific systemic disease or pathology as the underlying cause.5 NS-NP is a heterogeneous disorder where multiple factors, such as pain sensitivity or pain extent, influence central and peripheral mechanisms.6 It is necessary to study further the correlation between NSNP patients and cervical sagittal balance from the cervical sagittal perspective. Much work has been done on the sagittal parameters of the cervical spine in patients with neck pain. Early imaging studies of the cervical spine by Gore et al. suggested that degenerative changes in C6/C7 might be considered a risk factor for the development of neck pain in the future.7 In addition, Moon and Choi et al.8 conducted a cross-sectional study of Air Force pilots, and they found a lower C2–C7 angle in subjects with neck pain. In 2019, Jouibari et al.9 further showed that a population of patients with non-specific neck pain had a significantly lower slope of the upper endplate of the T1 vertebrae body (T1 slope) compared to the healthy population. They suggested that this may be related to a compensatory mechanism that shifts the center of head gravity back to the spinal axis. In contrast, some studies have proposed global sagittal balance measurements, and Grob et al. conducted a study of global sagittal parameters in patients with neck pain and found no significant differences between subjects with and without neck pain.10 This finding was further supported by other studies.11, 12 Compared to the above studies, we believe that the sagittal parameters and study population categories related to the preoperative cervical spine are slightly underrepresented. According to recent reports in the relevant literature, three key cervical sagittal parameters, the spino-cranial angle (SCA), the C7 slope (C7s), the T1 slope (T1s), and the C2–7 sagittal vertical axis (C2–C7 SVA) are the focus of future studies.2, 13 SCA is an easily neglected but essential parameter for measuring the sagittal balance of the cervical spine and has attracted much attention in recent years.14-17 SCA is the first parameter that connects the cervical spine base with the head's weight, creatively raising the concept of head offset, which has yet to be extensively studied as a new parameter to evaluate sagittal plane balance.14, 15 The present study demonstrates the correlation between SCA and other parameters. Further, this study elevated the control study population to a more accessible cervical spine patient.
Therefore, the purpose of this study is to (i) compare the cervical sagittal parameters between nonspecific neck pain (NS-NP) and cervical spondylotic radiculopathy (CSR) and cervical spondylotic myelopathy (CSM) and (ii) illustrate the relationship between each cervical parameter.
Materials and Methods
The institutional review board of our institution approved the current retrospective research, and a waiver of consent was acquired (Approval 2022–113-1).This paper assessed patients who presented to our hospital with posterior neck discomfort between January 2020 and October 2022. Inclusion criteria: (i) patients with nonspecific neck pain were diagnosed by questioning, physical examination, and imaging to rule out neck pain due to specific systemic diseases; (ii) patients diagnosed with cervical spondylotic radiculopathy and cervical spondylotic myelopathy after hospitalization; and (iii) complete imaging and patient information data. Exclusion criteria: (i) history of previous spinal surgery, cervical spine infection, cervical spine trauma, spinal tumor, and congenital spinal deformity; (ii) incomplete patient information data records; and (iii) the T1 vertebrae cannot be fully revealed on cervical X-ray for various reasons (e.g., patients with obesity and short neck) and other conditions. Ultimately, 236 patients were selected as the research objective, and their general characteristics, such as age, sex, height, and weight, were recorded prior to imaging evaluation.
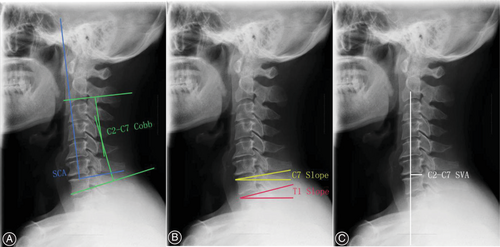
Radiological Measurement
Lateral cervical spine films were obtained for all subjects using a picture archiving and communication system, with the subjects in a neutral position and looking straight ahead. The C2–C7 angle, C2–C7 SVA, T1 slope (T1s), C7 slope (C7s), and spino-cranial angle (SCA) were measured on cervical radiographs. All concerning sagittal parameters were evaluated (Fig. 1)2, 4, 9: (i) C2–C7 Cobb angle, the angle between the lower plate of C2 and the lower plate of C7; (ii) C2–C7 sagittal vertical angle (SVA), the distance from the posterior, superior corner of C7 to the plumbline from the centroid of C2; (iii) T1 slope (T1s), the angle between a horizontal line and the superior endplate of T1; (iv) C7 slope (C7s), the angle between a horizontal line and the superior endplate of C7; and (v) spino-cranial angle (SCA), the angle between the C7 slope and the straight line joining the middle of the C7 end plate and the middle of the sella turcica.
Statistical Analysis
Two independent observers determined measurements. Then, two measurements were taken by two spine surgeons for each covariate, and the intragroup correlation coefficient (ICC) was analyzed as the mean of each observer's measurements. Intra- and inter-observer agreement was excellent, with ICC values ranging from 0.976 to 0.984. The measurement data are the mean ± standard deviation, and the counting data are totals and percentages. SPSS software (version 26.0; SPSS, Chicago, Illinois) was adopted to perform all analyses. If the data between the three groups met the normality and homogeneity of variance test, one-way ANOVA was used, and the Bonferroni test was used for pair-to-group comparison. If the variances were inconsistent, the Welch test was used, and pairwise comparisons between groups were performed using Tamhane's T2 test. The Kruskal–Wallis test was used for nonnormality or inconsistent variance data. The parameters between the groups’ sexes approximately met the normality and homogeneity of variance test, and an independent t-test was used. The χ2-test was used for classified data. Pearson's or Spearman's correlation analysis was used to assess the correlation between all patients’ cervical sagittal parameters between the three groups. p < 0.05 was considered statistically significant.
Results
General Data
- 70 patients with NS-NP (22 males and 48 females)
- 74 patients with CSR (37 males and 37 females)
- 92 patients with CSM (58 males and 34 females).
The characteristics of these patients are summarized in Table 1. There were significant differences in age and sex among the three groups (p < 0.001); the age of the NS-NP group was the youngest (41.77 ± 12.00), and NS-NP was more common in women. No significant differences in height, weight, or body mass index (p > 0.05) existed.
| Variables | Patients with NS-NP | Patients with CSR | Patients with CSM | χ2-value/F-value | p-value |
|---|---|---|---|---|---|
| Number of patients (n) | 70 | 74 | 92 | ||
| Age (years) | 41.77 ± 12.00 | 51.35 ± 9.63 | 54.10 ± 11.70 | 25.491 | <0.001*** |
| Male/Female | 22/48 | 37/37 | 58/34 | 15.902 | <0.001*** |
| Weight (kg) | 68.04 ± 7.06 | 68.45 ± 9.64 | 68.80 ± 10.98 | 0.150 | 0.861 |
| Height (m) | 1.66 ± 0.08 | 1.65 ± 0.08 | 1.66 ± 0.08 | 0.663 | 0.516 |
| BMI (kg/m2) | 24.84 ± 2.97 | 25.18 ± 2.51 | 24.91 ± 3.11 | 0.279 | 0.757 |
- Abbreviations: BMI, body mass index; CSM, cervical spondylotic myelopathy; CSR, cervical spondylotic radiculopathy; NS-NP, nonspecifc neck pain; SD, standard deviation.
- *** p < 0.001.
Cervical Imaging Parameters
Table 2 summarizes the values and changes in each cervical sagittal parameter among the three groups. There were significant differences in each cervical sagittal parameter between the three groups for the C2–C7 Cobb angle (p < 0.001), C2–C7 SVA (p = 0.001), C7s (p = 0.009), T1s (p = 0.008), and SCA (p = 0.002).
| Variables | Patients with NS-NP | Patients with CSR | Patients with CSM | F-value | p-value |
|---|---|---|---|---|---|
| C2–C7 Cobb angle (degree) | |||||
| Total | 16.00 ± 8.86 | 9.65 ± 12.11 | 9.73 ± 12.02 | 9.892 | <0.001 |
| Male | 18.58 ± 10.21 | 10.21 ± 12.73 | 11.58 ± 13.61 | ||
| Female | 14.81 ± 8.01 | 9.09 ± 11.60 | 6.58 ± 9.11 | ||
| t-value | −1.528 | −0.394 | −2.149 | ||
| p-value | 0.136 | 0.695 | 0.034* | ||
| C2–C7 SVA (cm) | |||||
| Total | 1.78 ± 0.77 | 2.32 ± 0.90 | 2.19 ± 0.99 | 6.968 | 0.001 |
| Male | 1.94 ± 0.87 | 2.37 ± 0.89 | 2.17 ± 1.06 | ||
| Female | 1.72 ± 0.72 | 2.27 ± 0.92 | 2.21 ± 0.86 | ||
| t-value | −1.109 | −0.504 | 0.163 | ||
| p-value | 0.271 | 0.616 | 0.871 | ||
| C7 slope (deg) | |||||
| Total | 19.84 ± 6.48 | 16.77 ± 7.86 | 16.60 ± 7.01 | 4.860 | 0.009** |
| Male | 23.28 ± 6.24 | 17.17 ± 8.50 | 17.50 ± 7.61 | ||
| Female | 18.27 ± 6.01 | 16.38 ± 7.24 | 15.07 ± 5.63 | ||
| t-value | −3.204 | −0.430 | −1.317 | ||
| p-value | 0.002** | 0.668 | 0.191 | ||
| T1 slope (deg) | |||||
| Total | 23.51 ± 6.11 | 19.95 ± 8.12 | 20.30 ± 7.94 | 4.969 | 0.008** |
| Male | 26.16 ± 5.07 | 20.50 ± 8.61 | 21.13 ± 9.00 | ||
| Female | 22.29 ± 6.21 | 19.41 ± 7.67 | 18.88 ± 5.56 | ||
| t-value | −2.560 | −0.571 | −1.619 | ||
| p-value | 0.013* | 0.570 | 0.109 | ||
| SCA (degree) | |||||
| Total | 76.81 ± 7.76 | 81.80 ± 8.86 | 80.61 ± 9.30 | 6.439 | 0.002** |
| Male | 72.66 ± 10.14 | 81.06 ± 9.36 | 78.88 ± 10.39 | ||
| Female | 78.71 ± 5.54 | 82.54 ± 8.39 | 83.55 ± 6.14 | ||
| t-value | 2.624 | 0.715 | 2.710 | ||
| p-value | 0.014* | 0.477 | 0.008** |
- Abbreviations: CSM, cervical spondylotic myelopathy; CSR, cervical spondylotic radiculopathy; deg., degrees; NS-NP, nonspecifc neck pain; SCA, spino-cranial angle; SD, standard deviation.
- * p < 0.05;
- ** p < 0.01.
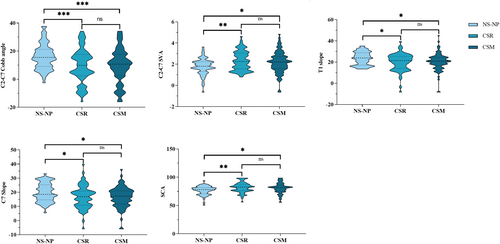
Figure 2 shows the differences between the three groups for a two-by-two comparison of each imaging parameter. For the C2–C7 Cobb angle, the mean value of the NS-NP group was significantly greater than that of the CSR group (16.00 ± 8.86 vs. 9.65 ± 12.11, p < 0.001) versus the CSM group (16.00 ± 8.86 vs. 9.73 ± 12.02, p < 0.001). For C2–C7 SVA, the mean value of the NS-NP group was significantly lower than that of the CSR group (1.78 ± 0.77 vs. 2.32 ± 0.90, p < 0.01) and CSM groups (1.78 ± 0.77 vs. 2.19 ± 0.99, p < 0.05). For C7s, the mean value of the NS-NP group was higher than that of the CSR group (19.84 ± 6.48 vs. 16.77 ± 7.86, p < 0.05) and CSM groups (19.84 ± 6.48 vs. 16.60 ± 7.01, p < 0.05). For T1s, the mean value of the NS-NP group was also higher than that of the CSR group (23.51 ± 6.11 vs. 19.95 ± 8.12, p < 0.05) and CSM groups (23.51 ± 6.11 vs. 20.30 ± 7.94, p < 0.05). For SCA, the mean value of the NS-NP group was significantly lower than that of the CSR group (76.81 ± 7.76 vs. 81.80 ± 8.86, p < 0.01) and CSM groups (76.81 ± 7.76 vs. 80.61 ± 9.30, p < 0.05). However, there were no significant differences in cervical sagittal parameters between the CSR group and the CSM group (p > 0.05).
Correlation Analysis of Cervical Sagittal Parameters
Pearson's or Spearman's correlation analysis was performed to determine correlations between different cervical sagittal parameters in all patients among the three groups (Table 3). There were positive correlations between the C2–C7 Cobb angle and C7s (r = 0.618, p < 0.01), C2–C7 Cobb angle and T1s (r = 0.653, p < 0.01), C2–C7 SVA and C7s (r =0.181, p < 0.01), C2–C7 SVA and T1s (r = 0.154, p < 0.05), C2–C7 SVA and SCA (r = 0.285, p < 0.01), and C7s and T1s (r = 0.861, p < 0.01). There were negative correlations between the C2–C7 Cobb angle and C2–C7 SVA (r = −0.265, p < 0.01), C2–C7 Cobb angle and SCA (r = −0.841, p < 0.05), C7s and SCA (r = −0.678, p < 0.01), and T1s and SCA (r = −0.620, p < 0.01).
| Parameters | Age | BMI | C2–C7 Cobb angle | C2–C7 SVA | C7 slope | T1 slope | SCA |
|---|---|---|---|---|---|---|---|
| Sex | 0.031 | 0.023 | 0.085 | 0.090 | 0.118 | 0.135* | −0.167** |
| Age | −0.011 | −0.055 | 0.055 | −0.028 | −0.031 | 0.034 | |
| BMI | −0.039 | 0.036 | −0.072 | −0.001 | 0.109 | ||
| C2–C7 Cobb angle | −0.265** | 0.618** | 0.653** | −0.841** | |||
| C2–C7 SVA | 0.181** | 0.154* | 0.285** | ||||
| C7 slope | 0.861** | −0.678** | |||||
| T1 slope | −0.620** |
- Abbreviation: SCA, spino-cranial angle.
- * p < 0.05
- ** p < 0.01.
Sex-Related Changes in Cervical Sagittal Parameters
To observe the differences in cervical sagittal parameters between sexes, the three case groups were grouped separately according to sex in this study (Table 2). In the NS-NP group, both C7s and T1s were significantly larger in men than in women (23.28 ± 6.24 vs. 18.27 ± 6.01, p < 0.01) and T1s (26.16 ± 5.07 vs. 22.29 ± 6.21, p < 0.05), while SCA was smaller in men than in women (72.66 ± 10.14 vs. 78.71 ± 5.54, p < 0.05). In the CSM group, the C2–C7 Cobb angle was greater in men than in women (11.58 ± 13.61 vs. 6.58 ± 9.11, p < 0.05), and the SCA in men was significantly smaller than in women (78.88 ± 10.39 vs. 83.55 ± 6.14, p < 0.01). There were no significant differences in cervical sagittal parameters between men and women in other groups (p > 0.05).
Discussion
Our study compared cervical sagittal parameters between patients with NS-NP and CSR and CSM by cervical spine radiographs. Our analysis of the results revealed smaller C7s, T1s, and C2–C7 Cobb angles and greater SCA, and C2–C7 SVA in patients with NS-NP compared to patients with CSR and CSM. In the NS-NP group, both C7s and T1s were significantly more prominent in men than in women and T1s, while SCA was smaller in men than in women.
Characteristics of Changes in Cervical Sagittal Parameters between the Three Groups of Patients
Our results showed that the C2–C7 sagittal axial distance (SVA) and spinal cranial angle (SCA) of patients in the NS-NP group were significantly greater than those in the CSR and CSM groups. In contrast, the C2–C7 anterior convex angle, C7s, and T1s of patients in the NS-NP group were significantly smaller than those in the CSR and CSM groups. This is similar to the results of previous studies.9, 18, 19 In people with degenerative cervical spondylosis, the physiological curve of the cervical spine becomes progressively straighter or more lordotic, which leads to a forward shift of the head's center of gravity, resulting in a progressive increase in C2–C7 SVA and SCA and an increase in C7s and T1s to compensate for the sagittal balance of the spine. In contrast to CSR and CSM patients, NS-NP patients may have mainly localized muscle fatigue or stiffness, and patients often complain of localized neck pain.20-22 However, in slowly progressive diseases, such as myelopathy, the nature of patients’ complaints is less likely to be localized, and their perception of disability suggests that the sagittal position of the cervical spine in the population of patients with degenerative cervical spondylosis is affected by large variations.19 Jouibari et al.9 reported that there were no differences in the changes in cervical sagittal parameters in patients with neck pain compared with the asymptomatic population, except for the decrease in T1s. It also better explains our results showing that NS-NP patients are less affected by changes in cervical sagittal parameters than patients with cervical spondylosis and tend to present similar results as the average population.
Correlation Analysis and Interpretation of Cervical Sagittal Parameters
We performed a correlation analysis of cervical sagittal parameters, and the results of our study showed a significant negative correlation between the C2–C7 Cobb angle, C2–C7 SVA, and T1 slope and SCA angle, which is consistent with previous findings.2, 15, 17 In recent studies, a new cervical sagittal parameter, SCA, has gradually been proposed to assess the relationship of SCA with other cervical sagittal parameters and postoperative recovery indices. It has been proposed that SCA can be considered another critical parameter to predict imbalance and that higher SCA is positively correlated with NDI in cervical spine patients.14, 15 Wang et al.14 reported that patients with a higher SCA had a lower T1 slope (T1s) and C2–C7 Cobb angle, preoperatively, postoperatively, and at follow-up. The results of this study also showed positive correlations between the C2–C7 Cobb angle and C7 slope, C2–C7 Cobb angle and T1 slope, C2–C7 SVA and C7 slope, C2–C7 SVA and T1 slope, C2–C7 SVA, and SCA, and C7 slope and T1 slope, while the C2–C7 Cobb angle was negatively correlated with C2–C7 SVA. Iyer et al.19 showed a strong correlation between the C2–C7 Cobb angle, T1s, and T1s-C2–C7 Cobb angle. There was a strong correlation between high T1s and high C2–C7 Cobb angle, often found in the same subgroup of patients. The study further suggested that an increased C2–C7 Cobb angle, TS, and T1s-C2–C7 Cobb angle were all associated with decreased NDI. A low T1s-C2–C7 Cobb angle and high C2–C7 SVA were independent predictors of high preoperative NDI. These correlations indicate that the sagittal curvature of the cervical spine is closely related to the sagittal displacement of the cervical spine. In degenerative cervical spine diseases, cervical curvature changes are among the most common radiographs.23, 24 When the cervical spine is in prolonged flexion, and the muscle balance along the cervical spine is altered, the muscles and ligaments of the neck are subjected to abnormal mechanical loading, resulting in ligament and joint capsule laxity and loss of cervical physiological curvature (i.e., a decreased C2–C7 Cobb angle).9, 25 When the C2–C7 Cobb angle decreases, the center of gravity of the head (CGH) and C2 vertebrae moves forward, which will lead to the same increase of C2–C7 SVA to maintain balance and offset the adverse effects caused by CGH moving forward.26
In addition, we found that the C2–C7 Cobb angle was positively correlated with the T1 slope and C7 slope, suggesting that when the C2–C7 Cobb angle decreases, the T1 slope and C7 slope exhibit a compensatory decrease to restore the imbalance caused by the CGH forward shift.23, 27-29 Xing et al.18 found that T1s was positively correlated with the C2–C7 Cobb angle, and lower T1s decreased the C2–C7 Cobb angle, resulting in a sagittally balanced cervical spine and a relatively straight cervical spine. This mechanism might increase gravity-induced stress and accelerate cervical disc degeneration. A related study by Weng et al.28 also found a significant relationship between the C2–C7 angle and the T1 slope. T1 slope was the only parameter significantly correlated with the C2–C7 Cobb angle and C2–C7 SVA. Patients with higher T1s required greater cervical anterior convexity to maintain cervical physiological sagittal balance. When the physiological curvature of the cervical spine is reduced, many parameters of the cervical spine will change, and there is a correlation between these changes. Relevant experimental research results show that the changes in cervical sagittal are closely related to the complex compensation mechanism, which is also related to the spinal alignment, such as thoracic kyphosis and sacral inclination.3, 4, 30 In general, the implementation of compensatory mechanisms relies on excessive muscle contraction and tension in the spine and small disc joints, which can further accelerate the progression of spinal degeneration and cause a series of related clinical symptoms, such as low back pain, neck pain, and shoulder pain.31 Therefore, spine surgeons should consider the patient's cervical sagittal balance during cervical spine surgery and try to restore normal cervical physiological curvature, and studying cervical sagittal balance may help spine surgeons develop better treatment strategies.32-34
Sex-Related Changes in Cervical Sagittal Parameters
We also performed a comparative analysis of sex differences in cervical sagittal parameters. The patients in the NS-NP group were the youngest. These findings are similar to those reported by Cohen et al.,1 neck pain is more common in middle-aged and young people, such as office and computer workers, manual laborers, medical workers, and professional drivers, who are more likely to experience neck and shoulder pain than others. Among patients with nonspecific neck pain, we found that female patients were often more common than male patients, which corresponded with other reports.21, 22 Kumagai et al.22 found that degenerative changes were associated with the severity of neck pain in women. The thorax's anteroposterior (AP) diameter is significantly smaller in women with chronic neck pain than in men. The size of the thoracic AP may predict neck pain, and the AP diameter of the uppermost thorax, the basis of head and neck motion fixation, is an important factor. The smaller the bottom, the more likely and frequent the head is to go beyond it, especially when the head is moving forward.35 It explains the greater SCA in women than men in the NS-NP group and that the cervical spine compensates for the forward shift of the head's center of gravity by decreasing C7s and T1s.27 Zhu et al.29 found that the C2–7 Cobb angle and C7s showed significant differences between male and female groups. These findings imply differences in the sagittal position of the cervical spine between males and females, suggesting that gender differences should be considered preoperatively.
Strengths and Limitations
The strengths of this study are as follows. First, this study reports the comparison of cervical sagittal parameters for the first time between patients with non-specific neck pain and those with cervical spondylotic radiculopathy and cervical spondylotic myelopathy. Second, it clarifies that these parameters are closely related to cervical spine disease and emphasizes the importance of cervical sagittal balance. As a simple, convenient, and noninvasive examination, lateral radiographs of the cervical spine are necessary to evaluate the sagittal balance of the cervical spine. Of course, there are also some shortcomings. First, the lack of clinical data in this study and the failure to compare preoperative and postoperative cervical sagittal parameters and some clinical outcomes in cervical spondylotic radiculopathy and cervical spondylotic myelopathy is a problem that we need to address in our subsequent studies. Second, this study only evaluated the parameters of the local sagittal position of the cervical spine, which may have specific limitations on the conclusion. Meanwhile, when measuring the SCA, we found that a few patients’ cervical sagittal X-rays showed a significant angle between the upper and lower C7 endplate lines, which may affect the SCA and the C2–C7 Cobb angle measurements. As a whole, this situation affects a minority of the X-rays of the patients we included and does not significantly affect the results of our study. The use of sagittal radiographs of the whole spine can be enhanced. Finally, this study is a single-institution center study. More research is needed to supplement and confirm the above results.
Conclusions
This study showed that between the three groups, patients with nonspecific neck pain had smaller SCA, and among patients with NS-NP, women had more significant SCA. The smaller anteroposterior (AP) diameter of the thorax in women might explain this difference. There was a strong correlation between each cervical sagittal parameter.
Disclosure Statement
All authors have nothing to disclose.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics Statement
All authors listed above meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors. All authors are in agreement with the manuscript.
Author Contribution
Dalong Yang and Zheng Wang conceived and designed the study. Tao Liu and Shuo Tian collected clinical and imaging data of the patients, and some imaging data. Tao Liu, Jianzhou Zhang, Mengzi He, Wenyuan Ding, and Longlian Deng analyzed and interpreted the patient data. Tao Liu wrote the paper. All authors read and approved the final manuscript.
Open Research
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.