A Novel Multiple Screw Distraction Reducer System in the Treatment of Scoliosis with a Severe Rib Hump
Zhipeng Deng and Liang Wang contributed equally to this work and should be considered co-first author.
Grant sources: This study was supported by Key R&D Projects of Sichuan Provincial Department of Science and Technology (2021YFG0240); Science and Technology Project of the Health Planning Committee of Sichuan (2022NSFSC1528); the 1–3-5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYGD21001); Project funded by China Postdoctoral Science Foundation (2023M732469); and the Sichuan University Postdoctoral Interdisciplinary Innovation Fund (JCXK2205).
Disclosure: On behalf of all authors, the corresponding author states that there is no conflict of interest.
Abstract
Objectives
The treatment of scoliosis with a severe rib hump remains a major challenge. Traditional vertebral rotation techniques are not satisfactory, and thoracoplasty has many pulmonary complications that limit its application. A novel surgical device, the multiple screw distraction reducer (MSDR) system, provides longitudinal distraction during the corrective operation while at the same time providing lateral translation and axial derotation, which may facilitate the correction of a rib hump. This study was performed to investigate the effectiveness of the MSDR system for adolescent idiopathic scoliosis (AIS) with a severe rib hump.
Methods
This was a case-matched study of patients with retrospectively collected data from our hospital between January 2017 and December 2021. Sixty-eight patients who underwent one-stage posterior pedicle screw-instrumented spinal fusion were matched by the Cobb angle of the main curve and rib hump. All patients underwent a minimum of 2 years of follow-up. The patients were divided into two groups: the MSDR group (using the MSDR system, n = 34) and the DVR group (using direct vertebral derotation, n = 34). The patients were evaluated for the height of the rib hump, deformity correction, complications, and SRS-30 scores. The unpaired Student's t-test and Pearson's χ2-test were used to compare the outcome measures between the two groups. Multiple linear regression analysis was used to examine the variables that affected the correction of a rib hump.
Results
The rib hump was 30.21 ± 6.21 mm versus 29.35 ± 6.52 mm (p = 0.583) preoperatively and 9.18 ± 4.06 mm versus 13.82 ± 5.54 mm (p < 0.001) at the last follow-up in the MSDR and DVR groups, respectively. The correction rates were 70.83% and 53.56%, respectively (p < 0.001). Preoperatively, the main thoracic curve was 58.43° ± 7.97° and 57.84° ± 6.32° (p = 0.736) and was corrected to 10.92° ± 5.47° and 19.14° ± 5.32° (p < 0.001) at last follow-up in the MSDR and DVR group, respectively. Thoracic kyphosis was restored from 18.24° ± 5.19° and 17.98° ± 5.28° (p = 0.836) in the MSDR and DVR group to 24.59° ± 4.41° and 19.32° ± 4.96° (p < 0.001), respectively. Correction of apical vertebra rotation and translation in the main thoracic curve were significantly better in the MSDR group than in the DVR group (p < 0.05). There was no significant difference in the Lenke type, implant density, estimated blood loss, or follow-up duration between the two groups, whereas the operation time in the DVR group was significantly less than that in the MSDR group. There were only two minor pulmonary complications in the MSDR group. At the last follow-up, the MSDR group scored higher in terms of appearance and satisfaction (p < 0.05).
Conclusion
The MSDR system, enabling better coronal alignment, thoracic kyphosis, and axial derotation, could be a safe and effective technique for severe rib hump correction in AIS.
Introduction
The rib hump, associated with adolescent idiopathic scoliosis (AIS) secondary to the rotation and lateral migration of the vertebral body, often affects the patient's appearance and psychological health.1, 2 Pedicle screw instrumentation systems combined with vertebral derotation techniques, such as direct vertebral rotation (DVR), vertebral column manipulation (VCM), and vertebral coplanar alignment (VCA), have been developed to improve deformity correction.3-5 However, these techniques cannot achieve ideal orthopaedic effects for severe rib humps. The correction rate of rib humps with DVR has been reported to be 54%,6 and there is little to suggest that VCM or VCA can achieve better improvement for a rib hump. Thoracoplasty was introduced as a procedure to further correct rib prominences by cutting the involved ribs adjacent to the costovertebral joint.7, 8 A preoperative rib hump greater than 20–30 mm was considered to be the indication for thoracoplasty,8, 9 and the correction rate of rib humps with thoracoplasty has been reported to be 70%.8 The common perioperative complications of thoracoplasty are pneumothorax, haemothorax, and pleural effusion. Permanent damage to pulmonary function is even more worrying.10 There was a statistically significant decrease in the percent-predicted forced vital capacity with a mean decrease of 4.84% and a significant decrease in the percent-predicted forced expiratory volume in 1 s with a mean decrease of 3.92%.10 Therefore, we raised a question: Can the corrective effect of rib hump deformity be further improved through advancements in surgical technique?
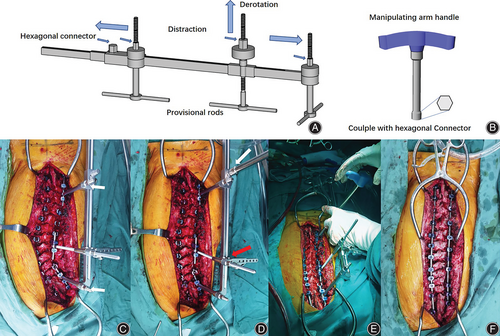
We developed a novel device with strong orthopaedic ability to achieve satisfactory correction for severe scoliosis (Cobb angle ≥90°) in one-stage posterior fixation fusion.11 In this approach, provisional rods are placed on the concave side of the spine proximally and distally; these rods are then linked to an external distraction reduction device called the multiple screw distraction reducer system (MSDR). Such a device provides longitudinal distraction during the corrective operation while at the same time providing lateral translation and axial derotation. This system may facilitate the correction of a rib hump, and its application in mild–moderate scoliosis with a severe rib hump has not yet been reported.
The purpose of the current study was to investigate the following: (i) the effectiveness of MSDR for mild–moderate scoliosis with a severe rib hump and (ii) the strength of MSDR compared to DVR for mild–moderate scoliosis with a severe rib hump with respect to radiographic outcomes, surgical information, and health-related quality outcomes, particularly focusing on rib humps.
Methods
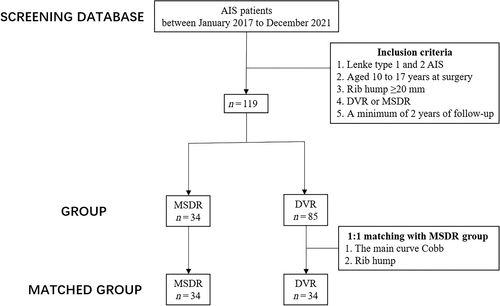
This was a case-matched study of patients with retrospectively collected data from our hospital, and it was approved by the ethics committee of our hospital (No. 2019852). The inclusion criteria were: (i) Lenke type 1 and 2 AIS patients aged 10 to 17 years at surgery between January 2017 to December 2021; (ii) patients who underwent one-stage posterior pedicle screw instrumented spinal fusion with DVR or MSDR; (iii) severe rib hump ≥20 mm and (iv) a minimum of 2 years of follow-up. Patients with incomplete clinical data were excluded. Overall, 34 patients underwent the MSDR system, serving as the MSDR group. To eliminate the selective bias, we performed 1:1 matching according to the Cobb angle of the main curve and rib hump. There were 34 patients in the DVR group, Figure 1.
Surgical Procedure
In the MSDR group, the MSDR correction technique was performed as previously reported.11 First, screw placement and multilevel Smith-Peterson and Ponte osteotomy were performed. The provisional rods were attached to the proximal, apical, and distal segments and fixed on the concave side of the spine. Second, the manipulating arms of the MSDR were inserted over the provisional rods. The first maneuver addressed the coronal deformity with multiple rounds of consistent distraction between the proximal and distal segments. The second maneuver aimed to correct the apical vertebral rotation and restore the thoracic kyphosis and was performed by rotating a hexagonal connector through the threaded shaft fixed on the concave side of the apical vertebrae. Third, the permanent rod was fixed on the convex side screw to further correct the scoliosis and vertebral body rotation through convex side compression and direct vertebral rotation.3 Finally, after MSDR device removal and in situ bending, a permanent fixation rod was placed on the concave side, and the final scoliosis correction was completed with concave side distraction (Figure 2). In the DVR group, scoliosis correction was completed through rod derotation, translation, and direct vertebral derotation.3
Clinical and Radiographic Evaluation
Information regarding age, sex, implant density, operation time, intraoperative blood loss, and complications was recorded. In a forward bending position, the hump height was measured as the vertical distance from the apex of the rib hump on the convex side to the apex of the concave rib. X-rays of the whole spine were taken preoperatively, postoperatively, and at the final follow-up. Apical vertebra translation (AVT) was defined as the distance from the center of the apical vertebra to the central sacral vertical line (CSVL). The measurement of AVR was performed according to the method described by Ho et al.12 According to the Cobb angle protocol, the degrees of proximal thoracic curve (PTC), main thoracic curve (MTC), and thoracic kyphosis (TK) were assessed. Preoperative side-bending X-ray films were used to assess the flexibility of the MTC. The horizontal distance between the C7 plumb line and CSVL (C7PL-CSVL) and the sagittal vertical axis (SVA) represented the coronal and sagittal balance, respectively. One orthopaedist (Z.P.) conducted all measures twice over a 2-week period. Another orthopaedist (L.W.) also measured these parameters. The intraobserver and interobserver reliability was evaluated by the intraclass correlation coefficients (ICCs). The mean intraclass coefficients (ICCs) of the intraobserver and interobserver reliability were 0.942 and 0.913, respectively.
Scoliosis Research Society-30 Questionnaire
To evaluate health-related quality outcomes, each patient completed the Scoliosis Research Society (SRS)-30 questionnaire during the final follow-up. The questionnaire consisted of 30 questions, which were categorized into five groups: function/activity, pain, self-image/appearance, mental health, and satisfaction. The responses measured people's satisfaction with their quality of life using a five-point Likert scale, ranging from favorable to unfavorable opinions. The domain scores were calculated using the SRS suggested scheme, which used a five-point scale to determine the outcome of each domain. A score of 5 indicated the best outcome, while a score of 1 represented the poorest outcome.
Statistical Analysis
Statistical analyses were carried out with SPSS 23.0 (SPSS, Chicago, Illinois, USA). Numerical variables are expressed as the mean ± standard deviation and were analyzed using unpaired Student's t-test and the Mann–Whitney U-test according to the distribution of these variables. Pearson's χ2-test and Fisher's exact test were used to compare categorical variables. A multiple linear regression analysis was used to examine the variables that affected the correction rate of rib humps. A p-value less than 0.05 was considered to indicate a significant difference. The G*power calculator was used to calculate the power of the test (1 − β) based on measurements of the rib hump. If 1 − β > 0.8, then the sample size was considered adequate.
Results
The present study included 68 patients (16 males, 52 females) with an average age of 14.9 years (range 12–17 years). The mean duration of follow-up was 30.4 months (range 24–59 months). The MSDR group and the DVR group each had 34 patients. The two groups were well matched in terms of the Cobb angle of the main curve, flexibility of the main curve, and rib hump. The demographic data and preoperative radiological characteristics are shown in Tables 1 and 2, and there was no significant difference in Lenke type, implant density, estimated blood loss, or follow-up duration between the two groups, whereas the operation time in the MSDR group (222.47 ± 24.77 min) was significantly longer than that in the DVR group (195.41 ± 23.93 min). Setting the significance level (α) to 0.01, the value of 1 − β in this study was greater than 0.99.
| Variables | MSDR group (n = 34) | DVR group (n = 34) | t/χ2 | p |
|---|---|---|---|---|
| Age at surgery (years) | 14.09 ± 1.94 | 14.65 ± 2.08 | −1.142 | 0.257 |
| Male/female | 9/25 | 7/27 | 0.327 | 0.776 |
| Lenke type (I/II) | 24/10 | 22/12 | 0.269 | 0.796 |
| Flexibility of MTC | 39.79 ± 11.61 | 38.69 ± 11.42 | 0.395 | 0.694 |
| Implant density | 1.23 ± 0.16 | 1.20 ± 0.11 | 0.859 | 0.393 |
| Operation time (min) | 222.47 ± 24.77 | 195.41 ± 23.93 | 4.581 | <0.001 |
| Estimated blood loss (mL) | 827.35 ± 108.69 | 791.76 ± 101.61 | 1.395 | 0.168 |
| Follow-up duration (months) | 29.74 ± 7.38 | 30.68 ± 7.72 | −0.514 | 0.609 |
- Abbreviation: DVR, direct vertebral rotation; MSDR, multiple screw distraction reducer; MTC, main thoracic curves;
| Variables | MSDR group (n = 34) | DVR group (n = 34) | t/χ2 | p |
|---|---|---|---|---|
| Rib hump (mm) | ||||
| Preoperative | 30.21 ± 6.21 | 29.35 ± 6.52 | 0.552 | 0.583 |
| 3 months | 8.24 ± 3.11 | 12.12 ± 3.98 | −4.488 | <0.001 |
| Last follow-up | 9.18 ± 4.06 | 13.82 ± 5.54 | −4.453 | <0.001 |
| The amount of correction | 21.03 ± 3.05 | 15.53 ± 3.54 | 6.868 | <0.001 |
| Correction rate | 70.83 ± 8.44 | 53.56 ± 9.26 | 8.041 | <0.001 |
| PTC (°) | ||||
| Preoperative | 29.40 ± 9.06 | 28.97 ± 7.60 | 0.213 | 0.832 |
| 3 months | 7.56 ± 5.44 | 8.80 ± 5.14 | −0.996 | 0.337 |
| Last follow-up | 7.62 ± 5.53 | 9.32 ± 4.91 | −1.346 | 0.183 |
| MTC (°) | ||||
| Preoperative | 58.43 ± 7.97 | 57.84 ± 6.32 | 0.338 | 0.736 |
| 3 months | 8.34 ± 5.66 | 16.73 ± 5.38 | −6.256 | <0.001 |
| Last follow-up | 10.92 ± 5.47 | 19.14 ± 5.32 | −6.281 | <0.001 |
| The amount of correction | 47.51 ± 7.94 | 38.70 ± 5.37 | 5.361 | <0.001 |
| Correction rate (%) | 81.38 ± 9.05 | 67.07 ± 7.91 | 6.938 | <0.001 |
| TK (°) | ||||
| Preoperative | 18.24 ± 5.19 | 17.98 ± 5.28 | 0.208 | 0.836 |
| 3 months | 26.12 ± 4.84 | 20.76 ± 4.55 | 4.696 | <0.001 |
| Last follow-up | 24.59 ± 4.41 | 19.32 ± 4.96 | 4.625 | <0.001 |
| AVT (mm) | ||||
| Preoperative | 40.82 ± 13.30 | 38.82 ± 12.70 | 0.635 | 0.528 |
| 3-months | 7.48 ± 9.72 | 13.41 ± 10.36 | −2.433 | 0.018 |
| Last follow-up | 8.65 ± 8.19 | 14.26 ± 9.18 | −2.625 | 0.010 |
| The amount of correction | 32.17 ± 12.36 | 24.56 ± 11.48 | 2.630 | 0.011 |
| Correction rate (%) | 78.87 ± 19.51 | 62.11 ± 25.72 | 3.210 | 0.002 |
| AVR (°) | ||||
| Preoperative | 17.08 ± 3.02 | 16.94 ± 3.11 | 0.190 | 0.850 |
| Postoperative | 9.77 ± 2.65 | 11.30 ± 3.08 | −2.191 | 0.032 |
| The amount of correction | 7.31 ± 2.92 | 5.64 ± 3.15 | 2.262 | 0.027 |
| Correction rate (%) | 42.34 ± 13.58 | 32.78 ± 17.66 | 2.505 | 0.015 |
| C7PL-CSVL (mm) | ||||
| Preoperative | 13.18 ± 8.38 | 11.55 ± 10.07 | 0.726 | 0.470 |
| 3 months | 12.34 ± 7.19 | 12.53 ± 10.44 | −0.084 | 0.993 |
| Last follow-up | 8.60 ± 6.34 | 9.67 ± 7.40 | 0.640 | 0.525 |
| SVA (mm) | ||||
| Preoperative | 15.73 ± 11.45 | 17.36 ± 13.08 | −0.545 | 0.588 |
| 3 months | 13.87 ± 8.96 | 14.64 ± 9.63 | −0.339 | 0.735 |
| Last follow-up | 11.83 ± 6.54 | 12.25 ± 6.39 | −0.270 | 0.788 |
- Note: The bold values highlighted that the difference between the groups was statistically significant (p < 0.05).
- Abbreviations: AVR, apical vertebra rotation; AVT, the horizontal distance between the C7 plumb line and the main thoracic apical vertebra; C7PL-CSVL, the distance from the C7 plumb line to the midline of the sacrum; DVR, direct vertebral rotation; MSDR, multiple screw distraction reducer; MTC, main thoracic curves; PTC, proximal thoracic curves; SVA, sagittal vertical axis; TK, thoracic kyphosis.
Rib Hump
The height of the rib hump was significantly reduced after surgery in both groups. In the MSDR group, the height of the rib hump improved significantly from 30.21 ± 6.21 mm preoperatively to 8.24 ± 3.11 mm postoperatively and to 9.18 ± 4.06 mm at the last follow-up, and the amount of correction was 21.03 ± 3.05 mm. In the DVR group, it improved from 29.35 ± 6.52 mm before surgery to 12.12 ± 3.96 mm postoperatively and to 13.82 ± 5.54 at the last follow-up, and the amount of correction was 15.53 ± 3.54 mm. The correction rates of hump height were 70.83% ± 8.44% and 53.56% ± 9.26% in the MSDR group and the DVR group, respectively. There was a significant difference in the postoperative height of the rib hump between the two groups. Comparing the amount and rate of correction between the two groups, the MSDR group was significantly superior to the DVR group.
Radiographic Outcomes
In the MSDR group, the preoperative main thoracic Cobb angle decreased from 58.43° ± 7.97° preoperatively to 8.34° ± 5.66°postoperatively. There was a slight loss of correction at the final follow-up of 10.92° ± 5.47°, and the amount of correction was 47.51° ± 7.94°. In the DVR group, the Cobb angle of the main thoracic region before, immediately after surgery, and at the last follow-up was 57.84° ± 6.32°, 16.73° ± 5.38°, and 19.14° ± 5.32°, respectively; and the amount of correction was 38.70° ± 5.37°. There was a significant difference between the two groups with respect to the 3-month postoperative and follow-up Cobb angle of the main curve (p < 0.001). The correction rates of the main thoracic curves were 81.38% ± 9.05% and 67.07% ± 7.91% in the MSDR group and the DVR group, respectively. The main curve correction rate of the MSDR group was significantly higher than that of the DVR group (p < 0.001). In the MSDR group, the preoperative thoracic kyphosis of 18.24° ± 5.19° was corrected to 26.12° ± 4.84° at the 3-month postoperative curve evaluation and to 24.59° ± 4.41° at the last follow-up. In the DVR group, the preoperative thoracic kyphosis of 17.98° ± 5.28° was corrected to 20.76° ± 4.55° at the 3-month postoperative curve evaluation and to 19.32° ± 4.96° at the last follow-up. There was a significant difference between the two groups with respect to 3-month postoperative and follow-up thoracic kyphosis. There were no significant differences between the two groups for PTC or coronal or sagittal balance at any time point (Table 2).
The preoperative AVT in MSDR and DVR group was 40.82 ± 13.30 mm and 38.82 ± 12.70 mm, and the preoperative AVR in MSDR and DVR group was 17.05° ± 3.04° and 16.94° ± 3.11°, with the values showing no significant difference between the two groups. The AVT and AVR significantly improved after surgery in both groups. The AVT correction in the MSDR group was better than that in the DVR group (7.48 ± 9.72 mm vs. 13.41 ± 10.36 mm, p = 0.018, postoperatively and 8.65 ± 8.19 mm vs. 14.26 ± 9.18 mm, p = 0.010, at the last follow-up). The amount of AVT correction was 32.17 ± 12.36 mm (correction rate: 78.87% ± 19.51%) in the MSDR group and in the DVR group was 24.56 ± 11.48 mm (correction rate: 62.11% ± 25.72%). Moreover, the postoperative AVR in the MSDR group and the DVR group were 9.77° ± 2.65° and 11.30° ± 3.08°, respectively (p = 0.032), and the MSDR group achieved a better correction than the DVR group (the amount of correction: 7.31° ± 2.92° vs. 5.64° ± 3.15°, p = 0.027; the correction rate: 42.34% ± 13.58% and 32.78% ± 17.66%, respectively, p = 0.015, Table 2).
Multivariate Predictor on Correction Rate of Rib Hump
A multiple regression analysis showed that the use of MSDR was the significant predictor for the correction rate of the rib hump (b = 16.70, p < 0.001; adjusted R2 = 0.475; Table 3).
| Predictors on correction rate of rib hump | Unstandardized | Standardized coefficients | 95% Confidence interval | t | p | ||
|---|---|---|---|---|---|---|---|
| Coefficient β | SE | Beta | Lower limit | Upper limit | |||
| MSDR or DVR | 16.70 | 2.83 | 0.680 | 11.07 | 22.33 | 5.929 | <0.001 |
| Correction rate of MTC | 0.084 | 0.138 | 0.065 | −0.193 | 0.360 | 0.606 | 0.547 |
| TK at the last follow-up | −0.174 | 0.237 | −0.076 | −0.649 | 0.300 | −0.735 | 0.465 |
| AVT at the last follow-up | −0.162 | 0.128 | −0.119 | −0.418 | 0.093 | −1.270 | 0.209 |
| Correction rate of AVR | −0.018 | 0.075 | −0.024 | −0.169 | 0.132 | −0.245 | 0.807 |
- Note: MSDR = 1, DVR = 0, adjusted R2 = 0.475, p < 0.001. The bold values highlighted that the difference between the groups was statistically significant (p < 0.05).
- Abbreviations: AVR, apical vertebra rotation; AVT, the horizontal distance between the C7 plumb line and the main thoracic apical vertebra; DVR, direct vertebral rotation; MSDR, multiple screw distraction reducer; MTC, main thoracic curves; TK, thoracic kyphosis.
Complications and Scoliosis Research Society-30 Score
In the MSDR group, one patient experienced pleural effusion and atelectasis. After 1 week of respiratory training, a chest X-ray examination revealed the absorption of pleural effusion and pulmonary atelectasis. No other pulmonary complications occurred in either group. Neurological or implant-related complications, such as screw misplacement, loosening, and breakage, did not occur in either group. In comparison to the DVR group, the MSDR group had higher overall SRS-30 scores, particularly in the self-image domain (4.13 ± 0.44 vs. 3.91 ± 0.39, p = 0.030), satisfaction domain (4.35 ± 0.53 vs. 4.09 ± 0.51, p = 0.044), and total average (4.21 ± 0.18 vs. 4.06 ± 0.25, p = 0.007) (Table 4). However, there was no significant difference found in comparisons between the function/activity domain, pain domain, and mental health domain.
| MSDR group (n = 34) | DVR group (n = 34) | t/χ2 | p | |
|---|---|---|---|---|
| Pain | 4.16 ± 0.56 | 4.01 ± 0.51 | 1.098 | 0.276 |
| Self-image/appearance | 4.13 ± 0.44 | 3.91 ± 0.39 | 2.223 | 0.030 |
| Mental health | 4.17 ± 0.43 | 4.12 ± 0.26 | 0.613 | 0.542 |
| Satisfaction | 4.35 ± 0.53 | 4.09 ± 0.51 | 2.053 | 0.044 |
| Function/activity | 4.24 ± 0.59 | 4.18 ± 0.64 | 0.393 | 0.696 |
| Total average | 4.21 ± 0.18 | 4.06 ± 0.25 | 2.781 | 0.007 |
- Abbreviations: DVR, direct vertebral rotation; MSDR, multiple screw distraction reducer.
Discussion
A novel MSDR system that provides powerful forces of distraction, derotation, and translation has been reported to achieve satisfactory correction of severe rigid scoliosis by one-stage posterior surgery.11 This study further explores the application of the system in the treatment of mild–moderate Lenke 1 and 2 type scoliosis with a severe rib hump. The study shows that the use of the MSDR system produces greater improvement in the rib hump as well as better coronal and sagittal correction compared to that of DVR. According to the SRS30 questionnaire, patients in the MSDR group had higher scores in the appearance and satisfaction domains.
Corrective Effect of Multiple Screw Distraction Reducer System for Rib Humps
Surgical correction of severe rib humps is still one of the main challenges in the treatment of AIS. In Hwang et al., the rib hump spontaneous corrected in AIS using the pedicle screw instrumentation system, and the correction was close to 40%.6, 8 Hwang et al. reported that the rib hump was further improved to 54% with the pedicle screw system and DVR technique.8 It was not ideal to correct a rib deformity by previous surgical techniques alone, and some surgeons think that thoracoplasty is necessary for severe rib deformities. Suk et al. reported that the preoperative hump height was reduced from 32.3 ± 9.7 mm to 13.4 ± 4.7 mm postoperatively (57% correction) when performing thoracoplasty and from 32.4 ± 9.2 mm to 9.4 ± 5.9 mm (70% correction) when performing both DVR and thoracoplasty.8 However, the pulmonary complications associated with thoracoplasty and the postoperative residual and obvious rib hump due to inadequate rib excision have made the application of thoracoplasty controversial. This study introduced a new system for the treatment of scoliosis patients with severe rib hump deformity. The rib hump was reduced from 30.21 ± 6.21 mm preoperatively to 9.18 ± 4.01 mm postoperatively, with an average correction rate of 70.83%. It was significantly higher than that of the DVR technique for the correction of rib humps.
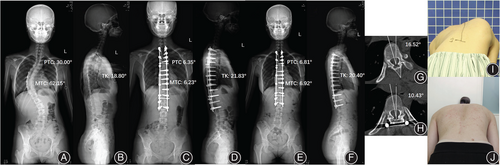
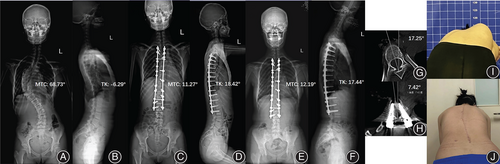
Vertebral body derotation and the improvement of lateral vertebral translation are considered to be crucial for the treatment of rib humps.13-15 The Pearson correlation coefficient between the rib hump deformity with AVR was 0.36 and with vertebral translation, it was 0.687,16 implying that the correction of the scoliosis itself facilitated the correction of the rib hump. The average rotational correction of the apical vertebra was 32.78% in the DVR group, which was similar to the previously reported results.14 Notably, the MSDR group achieved better derotation with an average AVR correction rate of 42.34%. There were two possible reasons for this difference. On the one hand, the longitudinal distraction of the spine itself could produce a derotation effect.17-19 Jhaveri et al. reported that the overall mean AVR, as measured using the Nash–Moe scale, of the major structural curve was 3.1 ± 0.8 preoperatively, and it was reduced to 2.4 ± 0.6 intraoperatively following skeletal (skull femoral) traction for the correction of large-magnitude idiopathic and neuromuscular scoliosis.20 The MSDR system performs internal longitudinal distraction on the scoliotic spine and may produce stronger traction that is more conducive to the correction of vertebral rotation. On the other hand, the system provided a derotational torque by pulling the apex vertebrae on the concave side. Furthermore, multiple rounds of distraction and simultaneous drawing back reduction translated the periapical vertebrae to the midline, which resulted in a significant reduction in AVT and Cobb in the MSDR group. Overall, the translation and derotation of vertebrae were performed at the same time as the distraction, and the MSDR group of rib deformity correction was satisfactory. Typical cases are shown in Figures 3 and 4. We also noted that patients with scoliosis have a deformity in the thoracic cavity itself,21 and this deformity may be greater in patients with a larger rib prominence. Therefore, we cautiously applied the MDSR system to patients with rib deformity height of 20–40mm. Further studies are needed to determine whether MDSR can also achieve good orthopaedic results in such patients.
Corrective Effect of Multiple Screw Distraction Reducer System for Scoliosis
Idiopathic scoliosis is a complex three-dimensional “coupling” of deformity, with the coronal translation, sagittal hyperkyphosis or hypokyphosis, and axial rotation.22 Based on the coupled motions of the spine, three-dimensional correction with DVR is a crucial component in scoliosis correction and has been reported to achieve excellent orthopaedic results. Previous studies presented 64%–73% correction in the coronal plane using DVR technology.23, 24 In the presented study, DVR provided a similar improvement in coronal correction. However, the MSDR system seems to be more compatible with this “coupling,” enabling longitudinal distraction while derotation and translation during the orthopaedic process, which achieved better axial and coronal correction. For the sagittal plane, intraoperative lifting and reduction of the apical vertebrae using MSDR may have a stronger ability to restore kyphosis. The results confirmed that the MSDR group exhibited superior results in achieving a better coronal curve and thoracic kyphosis when compared to the use of DVR.
Complications and Health-Related Quality of Life
The two pulmonary complications in the MSDR group were probably due to pleural irritation due to difficult nail placement or atelectasis due to a weak cough. Intraoperative complications related to internal fixation were also a concern, and they did not occur in this cohort of patients. The orthopaedic forces distributed to the attached pedicle screws and the uncoupled vertebrae released by osteotomy provided an opportunity for effective and safe correction. Rib hump deformity is the most cosmetically dissatisfying attribute patients note and affects postoperative cosmetic satisfaction.2 Pankowski et al. further found that postoperative self-image and satisfaction were linearly correlated with rib hump deformity improvement rate.14 Compared to the DVR group, the MSDR group had better rib hump correction and scored higher in terms of appearance and satisfaction. Therefore, the MSDR system could be a safe and effective technique for severe rib hump correction in mild–moderate AIS.
The Advantages of the Multiple Screw Distraction Reducer System
The MSDR system takes advantage of a powerful manipulating arm that connects the proximal and distal spinal segments, where each segment is fixed with two to three pedicle screws. The multi-screw linkage system distributes the powerful longitudinal distraction force generated in each segment, resulting in a safe distraction process and preventing screws from pulling out or loosening. The multiple rounds of distraction applied to the manipulating arms provide the coronal correction as well as translating the lateral migrated vertebrae to the midline. The manipulation of the middle provisional rod generates an upward lift pull and provides a derotational torque to achieve sagittal correction and true axial derotation of the whole spine and chest wall. Subsequently, while MSDR hold the correction, the permanent rod was fixed on the convex side screw to further correct the scoliosis through convex side compression and direct vertebral rotation. The MSDR system induces longitudinal distraction, lateral translation, and axial derotation at the scoliotic spine to provide an effective and safe opportunity for the correction of scoliosis with a severe rib hump.
Prospects of Clinical Application
In our medical center, the MSDR system with powerful forces of derotation has been applied to scoliosis of main curves located in lumbar spine, which is often accompanied by severe rotation of the vertebral body. The preliminary results showed that it has excellent results in vertebral derotation and lumbar scoliosis correction. In addition, the system can provide longitudinal distraction and generate an upward lift pull simultaneously, which has been used in the severe fracture and dislocation of the spine and has initially achieved good reduction. Research on the application of the MDSR system in other diseases is ongoing.
Limitations
There were several limitations of this study. In this cohort study, the number of patients with a severe rib hump using the MSDR system and long-term follow-up was relatively small. Due to the limited sample size, we did not conduct further stratified analysis of rib humps of different heights. In addition, this study was retrospective and a single-center study. Considering the radiation injury, chest computed tomography examinations were not performed routinely postoperatively, and we failed to analyze the thoracic morphology between the two surgical techniques.
Conclusion
This retrospective and case-matched study demonstrated that the MSDR system can achieve better correction of severe rib hump deformity than DVR technique. The MSDR system showed better coronal alignment, thoracic kyphosis, and axial derotation and patient satisfaction and self-image scores. Therefore, our results indicated that the MSDR system may be an ideal surgical technique for severe rib humps.
Acknowledgments
We wish to thank all patients who generously agreed to be interviewed for this study.
Author Contributions
All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: L.L. and Y.S. Acquisition of data: Z.D. and L.W. Analysis and interpretation of the data: Z.D., L.W., X.Y., and L.L. Drafting of the manuscript: D.Z. and L.W. Critical revision of the manuscript for important intellectual content: X.Y. and L.W. Statistical analysis: Z.D., and L.W. Obtained funding: Y.S. Study supervision: L.L. and Y.S.
Ethics Statement
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the West China hospital (No.2019852). Written informed consent was obtained from the patients.