The Quality of Life of the Patients with Thoracic Ossification of the Ligamentum Flavum after Surgery Using EQ-5D-5L
Junhu Li and Zhipeng Deng contributed equally to this study and shared first authorship.
Disclosure: The authors confirm that they have no conflict of interest with respect to the manuscript content or funding.
Abstract
Objective
There is a lack of studies on the quality of life (QoL) after posterior laminectomy in patients with thoracic ossification of the ligamentum flavum (TOLF), and risk factors associated with poor prognosis remain controversial. Therefore, the present study was conducted to illustrate the QoL for TOLF patients after surgery and determine its relationship with their demographic, surgery-related, clinical characteristics and imaging data.
Methods
One hundred and eighteen patients diagnosed with thoracic myelopathy because of TOLF were enrolled in this retrospective study. They all underwent posterior decompressive laminectomy from August 2010 to January 2022. The QoL was evaluated based on the EQ-5D-5L. Collecting gender, age, number of operations, compressed segments, Frankel grade, complications, body mass index (BMI), symptoms and duration, modified Japanese Orthopaedic Association (mJOA) score (preoperative), follow-up time and type of ossification, increased signal on Sagittal T2-weighted Images (ISST2I), occupancy rate and analyzing by Mann–Whitney U-test, Kruskal–Wallis test, the χ2-test, and logistic regression tests.
Results
Average follow-up 70.8 months (18–149), the mean age was 59.74 ± 9.81 years and the mean score for the QoL based on the EQ-5D-5 L and visual analogue scale (VAS) score were 0.71 ± 0.28 and 78.88 ± 10.21 at the final follow-up. Moderate and severe problems were found in the pain/discomfort in 22.0% of the patients. These mobility and usual activities numbers were slightly higher (24.6% and 30.4%, respectively). The mean scores for QoL and VAS were significantly higher in patients with mild and moderate neurological impairment, normal BMI, <60 years of age, no dural tears, symptom relief at hospital discharge, unilateral and bilateral ossification on axial CT scan, ≤ 50% spinal canal occupancy on CT and MRI, and none or fuzzy on ISST2I.
Conclusion
QoL after posterior laminectomy in TOLF patients is generally satisfactory compared to preoperative levels. Preoperative mJOA score, Age, comorbid diabetes, the major symptom is activity limitation, BMI, ISST2I, Intraoperative dural tears and spinal canal occupancy rate correlate significantly with the corresponding dimensions and are predictive. Age, spinal canal occupancy rate, ISST2I, preoperative mJOA score, BMI are significantly associated with and have predictive value for overall postoperative QoL.
Introduction
The heterotopic ossification of the ligament is known as ossification of the ligamentum flavum (OLF), it is most common in the thoracic spine. The OLF often leads to slowly progressive neurological impairment of the spinal cord, with clinical symptoms such as sensory and motor dysfunction of the lower limbs, positive pathological signs, and hyperreflexia.1 In 1920, Polgar2 first reported that thoracic ossification of the ligamentum flavum (TOLF) was closely associated with thoracic myelopathy. Previous studies showed that TOLF often occurs in Asian populations, with a prevalence of approximately 36% in the Japanese population3 and 3.8% in the Chinese population,2 and it has also been reported in Caucasian, African and Arab populations as well.4 TOLF is prevalent in the lower thoracic segment, with the highest occurrence in T10-11 and T11-12. Its prevalence increases with age.5 Once a patient with TOLF develops clinical symptoms, surgical decompression is usually the only effective treatment, with posterior decompression laminectomy of the posterior spinal canal being the primary surgical procedure.6 However, although the spinal canal decompression was complete and the operation went well, the surgical outcomes of TOLF are not always satisfactory.
Prior research shows that age, gender, body mass index (BMI), symptomatology, duration of symptoms, preoperative modified Japanese Orthopaedic Association (mJOA) score, imaging changes in intramedullary signal intensity, and the degree of spinal cord compression are associated with postoperative functional recovery.7, 8 However, there is still no consensus on the relationship between these factors and postoperative QoL. In addition, thoracic myelopathy resulting from TOLF often requires long-term rehabilitation exercises and psychological support, which places greater demands on long-term post-operative care. The associated costs, the reduction in social and family communication interactions, and the deterioration of the patient's lifestyle are often significant issues affecting the patient's family, social and economic situation. Therefore, surgeons need experience in predicting the outcome of TOLF surgery and identifying risk factors associated with poor surgical prognosis, as they help surgeons accurately predict the outcome of TOLF surgery using relevant preoperative demographic information and imaging information. However, there is still no consensus on risk factors, and most studies have focused only on postoperative neurological recovery, neglecting quality of life (QoL) aspects, including patients' psychological status, subjective feelings, and personal expectations.
Health-related quality of life (HRQoL) is one of the most widely measured treatment outcomes and is used to self-assess the impact of illness on health and to monitor the physical, psychological, and social aspects of an individual's health. It is influenced by individual expectations, beliefs, perceptions, and experiences.9 Some widely used tools to assess QoL are the SF-12, SF-36, and EQ-5D, created by Brook et al. in 1991.10 The EQ-5D is one of the most feasible tools for assessing an individual's QoL, integrating the physical, psychological, and social performance of the patients. It has been validated and used to assess QoL in many chronic diseases such as diabetes, chronic lung disease, chronic mental illness, cerebrovascular disease, and so forth.9 The EQ-5D is currently available in three versions, the EQ-5D-3L, EQ-5D-5L, and EQ-5D-Y. The Level 5 EQ-5D was launched by the EuroQoL Group in 2009 and had a higher sensitivity as well as a smaller ceiling effect than the other versions.11 In this study, the EQ-5D-5L is a concise questionnaire that patients could complete quickly, improving patient cooperation at follow-up and thus replacing the usual QoL questionnaires.
Therefore, this study aimed to: (i) describe the QoL status of TOLF patients after surgery; (ii) assess the relationship of patients' QoL with relevant demographics, surgery-related, clinical characteristics, and imaging information; and (iii) look for independent risk factors associated with poorer QoL.
Methods
Participants
Based on the inclusion criteria, this retrospective study included 118 out of 181 patients who were enrolled between August 2010 and January 2022. The ethics committee of West China Hospital, Sichuan University, approved this study (No. 2023241). The inclusion criteria were as follows: (i) patients with thoracic myelopathy caused by TOLF; (ii) patients who have sensory and/or motor impairment; (iii) patients who underwent posterior laminectomy either as a single surgery or multiple surgeries; and (iv) patients are followed up for at least 1 year. Exclusion criteria were as follows: (i) patients with systemic severe diseases or who had not undergone surgical treatment; (ii) patients with incomplete clinical symptoms and imaging data; (iii) patients with mental or psychological illnesses that prevent them from cooperating with the investigation; and (iv) patients with spinal or spinal cord trauma, infections, and tumors. The imaging data were analyzed and confirmed by the relevant radiologists and spinal surgeons.
Clinical Data
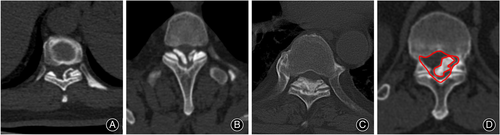
Demographic and clinical data collected include gender, age, number of surgeries, compressed segments, number of compressed segments, Frankel grade at admission, diabetes and hypertension, BMI, main symptoms and their duration, relief of symptoms at leaving the hospital (physical examination at the time of discharge showed improvement in sensory or motor function or increased muscle strength.), and the preoperative mJOA score. Surgery-related data including duration of surgery, intraoperative blood loss, and dural tears. The imaging data collected include: types of ossification on axial CT scan (unilateral, bilateral, bridge) and sagittal MRI (round, beak),12 spinal canal occupation ratio on axial CT and sagittal MRI (Figures 1 and 2)13, 14 and increased signal on Sagittal T2-weighted Images (ISST2I) (Figure 1).15 In addition, follow-up times were also collected to compare the effect of the length of follow-up time on QoL.

Main Outcomes
In order to collect patient-related information, three tools have been used, including the mJOA scales for evaluating the neurological function of the patient's lower limbs on day 3 before surgery, the EQ-5D-5L and SF-12 scales, which used to assess patients' QoL on preoperative day 3 and at the last follow-up time. We collected surgery-related, demographics and imaging data from the case system, measuring the spinal canal occupation ratio on axial CT with image J (V1.8.0) (Figure 2). Patients were followed up through clinic and telephone calls, and relevant questionnaires were collected.
EQ-5D-5 L Descriptive System
In the description system, there are five health dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression); each dimension is rated on a five-level scale (no problems, slight problems, moderate problems, severe problems, extreme problems).11 For each dimension, a one-digit code is generated for the patient based on their selection. For example, “Having a little difficulty” (“I find it difficult to walk around”) is recorded as “2.” Using the five dimensions, a five-digit code will be generated. For instance, 21,111 indicates that the respondent has a little difficulty walking around but no problems in other dimensions. However, a patient's health cannot be determined by the code's arithmetic properties or size. Therefore, a generalized score needs to be calculated from the “utility value set.” In this study, the value set of EQ-5D-5L recommended by previous studies for Chinese residents was used.16 As stated in the EQ-5D-5L user guide, each dimension has two levels: “no problems” (level 1) and “problems” (levels 2 to 5), changing the profile into reported problem frequencies.11 To look for correlates affecting overall QoL, the group with a better overall QoL is distinguished from the worse by using the median of the EQ-5D-5L value set.
EQ-5D-5 L Visual Analogue Scale (VAS)
The EQ-VAS is a 0–100 scale conceptually distinct from the EQ-5D utility value set in that the EQ-VAS scores represent the patient's perspective and are intensely subjective, in contrast, most utility value sets represent society's research perspective (i.e., the value of this state of health as judged by the general population) and are relatively objective. According to the EQ-VAS, patients self-rate their health on a vertical visual analog scale from 0 to 100, where the endpoints are labeled as “The best health you can imagine” and “The worst health you can imagine.” VAS 100 indicates the best health status, while VAS 0 represents the worst health status.11
EQ-5D-5 L Psychometric Properties
The Chinese version of the EQ-5D-5L questionnaire was used and tested on 10 patients at follow-up, and the results showed that all patients were able to understand the meaning of the questions. Factor analysis was undertaken on the five dimensions of the EQ-5D-5 L. The analysis produced a single component which accounted for 68.56% of the variance, indicative that the dimensions can be added together to create a single index score. Internal consistency was also assessed using the coefficient Cronbach's α, calculated at 0.88 for this questionnaire. To test the construct validity of the EQ-5D-5 L, the SF-12 questionnaire was administered to the subjects. Pearson's correlation coefficient was used to assess this type of validity and demonstrated that all the correlations were significant at the level of 0.01.
Statistical Analysis
Data were entered into SPSS 22 (SPSS Inc., Chicago, IL, USA) The continuous data were assessed with the Mann–Whitney U-test or Kruskal–Wallis test. The χ2-test was applied to compare the clinical categorical variables between the cohorts. Paired samples Wilcoxon signed rank test was chosen for paired samples. Statistical significance was inferred at α = 0.05.
In logistic regression model, the dependent variable (QoL, as measured by EQ-5D-5L) is dichotomized into “no problems” (level 1) and ‘problems’ (levels 2–5), and is used to analyze the risk factors associated with each dimension. The EQ-5D-5L value set obtained at the final follow-up is categorized into a relatively high QoL group and a relatively low QoL group. These are used to analyze the risk factors associated with overall poorer QoL. After entering independent variables into regression model including age, gender, number of operations, compressed segments, number of compressed segments, Frankel grading, complications, BMI, main symptoms, duration of symptoms, remission, mJOA score (preoperative), types of ossification on axial CT scan and sagittal MRI, spinal canal occupation ratio on axial CT and sagittal MRI, ISST2WI, duration of surgery, intraoperative blood loss, dural tears, and follow-up time. Single-factor logistic regression analysis was performed first, and variables with statistically significant differences in the single-factor analysis were then subjected to multi-factor unconditional logistic regression analysis to gradually incorporate the variables into the equation to summarize the data, only those variables that showed a significant relationship with a domain from EQ-5D-5 L were reported.
Results
Demographic Data
Of the 181 patients who underwent posterior laminectomy, 118 patients were ultimately enrolled in this study. At least 1 year follow-up, average follow-up 70.8 months (18–149), 46 had a follow-up of ≤ 70.8 months, and 72 had a follow-up of > 70.8 months. As shown in Table 1, 63 (53.4%) were male, and 55 (46.6%) were female, average age of 59.74 ± 9.81 years (37.0–85.0). The majority of patients had only one operation (N = 86, 72.9%). The greatest number of compression segment is the lower thoracic segment (N = 60, 50.8%). The mean number of compressed segments was 3.21 ± 2.07. The highest number of patients with a Frankel grade D on admission (N = 79, 66.9%) and comorbid diabetes mellitus (N = 36, 30.5%), and hypertension (N = 42, 35.6%). The BMI distribution is: thin (N = 0), normal (N = 44, 37.3%), and overweight (N = 74, 62.7%). Numbness/pain was the main symptom for 40 people (33.9%), with activity limitation in 21 (17.8%), and numbness and pain with activity limitation in 57 (48.3%). Duration of symptoms 0.5–276 months, mean 44.06 ± 51.08 months. Seventy eight (66.1%) patients had remission of symptoms at hospital discharge and 40 (33.9%) had no remission/presence of deterioration; in 18 of these patients, there was immediate postoperative neurological deterioration (15.3%). Of the preoperative mJOA scores, 32 (27.1%) had severe neurological deficits, 38 (32.2%) had moderate neurological deficits, and 48 (40.7%) had mild neurological deficits. There are 59 patients with operation time ≤ 200 min (50.0%) as well as > 200 min (50.0%), 66 with intraoperative blood loss ≤ 450 mL (55.9%) and 52 with > 450 mL (44.1%). Twenty-five patients with dural tears (21.2%).
| Characteristics | N (%) | |
|---|---|---|
| Sex | Female | 55 (46.6%) |
| Male | 63 (53.4%) | |
| Age (years) | ≤ 60 | 69 (58.5%) |
| > 60 | 49 (41.5%) | |
| Number of operations | 1 | 86 (72.9%) |
| > 1 | 32 (27.1%) | |
| Compressed segments | Upper/Mid | 19 (16.1%) |
| Lower | 60 (50.8%) | |
| Series | 39 (33.1%) | |
| Number of compressed segments | ≤ 3 | 76 (64.4%) |
| > 3 | 42 (35.6%) | |
| Frankel grade | B/C | 39 (33.1%) |
| D | 79 (66.9%) | |
| Complications | Diabetes | 36 (30.5%) |
| Hypertension | 42 (35.6%) | |
| BMI | Normal | 44 (37.3%) |
| Overweight | 74 (62.7%) | |
| Main symptoms | Numb/pain | 40 (33.9%) |
| Activity limitation | 21 (17.8%) | |
| Above | 57 (48.3%) | |
| Duration of symptoms | ≤ 24 | 61 (51.7%) |
| > 24 | 57 (48.3%) | |
| Remission of symptoms | No/Worse | 40 (33.9%) |
| Yes | 78 (66.1%) | |
| mJOA Score (preoperative) | Serious | 32 (27.1%) |
| Moderate | 38 (32.2%) | |
| Mild | 48 (40.7%) | |
| Duration of surgery | ≤ 200 min | 59 (50.0%) |
| > 200 min | 59 (50.0%) | |
| Intraoperative blood loss | ≤ 450 mL | 66 (55.9%) |
| > 450 mL | 52 (44.1%) | |
| Dural tears | Yes | 25 (21.2%) |
| No | 93 (78.8%) | |
| Follow-up time | ≤ 70.8 month | 46 (39.0%) |
| > 70.8 month | 72 (61.0%) | |
- Abbreviations: BMI, body mass index; mJOA, modified Japanese Orthopaedic Association score.
As shown in Table 2, the imaging data collected showed types of ossification on axial CT scan unilateral 30 (25.4%), bilateral (32.2%), bridging (42.4%), and on sagittal MRI Round 52 (44.1%), and beak 66 (55.9%). The spinal canal occupation ratio on sagittal MRI was 13.0%–96.0%, with a mean of 50.53% ± 21.87%; on axial CT, 11.0%–90.0%, mean of 41.99% ± 20.13%. Increased signal on sagittal T2-weighted image: none 29 (24.6%), fuzzy 41 (34.7%), and clear 48 (40.7%).
| Characteristics | N (%) | |
|---|---|---|
| Types of ossification (CT) | Unilateral | 30 (25.4%) |
| Bilateral | 38 (32.2%) | |
| Bridging | 50 (42.4%) | |
| Types of ossification (MRI) | Round | 52 (44.1%) |
| Beak | 66 (55.9%) | |
| ISST2I | None | 29 (24.6%) |
| Fuzzy | 41 (34.7%) | |
| Clearly | 48 (40.7%) | |
| Occupancy rate (MRI) | ≤ 50% | 63 (53.4%) |
| > 50% | 55 (46.6%) | |
| Occupancy rate (CT) | ≤ 50% | 79 (66.9%) |
| > 50% | 39 (33.1%) | |
- Abbreviation: ISST2I, increased signal on Sagittal T2-weighted images.
EQ-5D-5 L Results
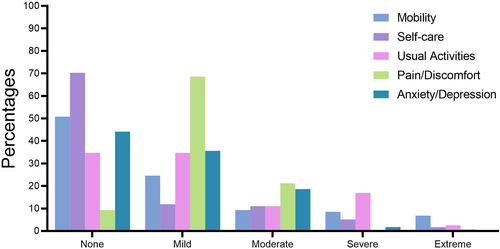
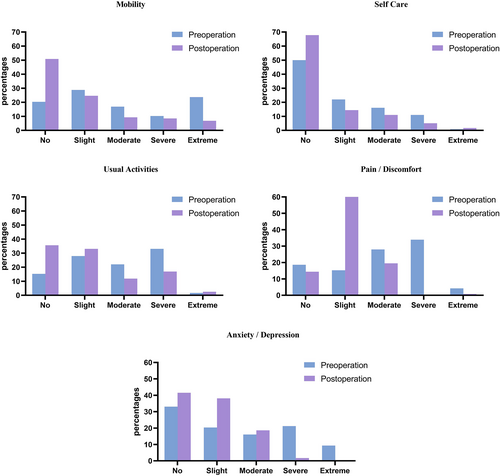
At the last follow-up, the mean score for the QoL based on the EQ-5D-5L questionnaire was 0.71 ± 0.28 (CI: 0.66–0.76), and the mean score of VAS scale was 78.88 ± 10.21 (CI: 77.02–80.74), compared to preoperative, QoL (0.44 ± 0.37) and VAS scale (62.31 ± 14.28) are significantly improved. Most of the patients did not report any problems or declared mild problems in various dimensions from the EQ-5D-5 L questionnaire. A higher percentage of patients reported no problems with mobility (50.80%), self-care (70.30%); however, there were more than moderate problems with usual activities (30.4%), pain/discomfort (22.0%), and mobility (24.6%). In Figure 3, percentages of each level of problems are shown in five dimensions. In Figure 4, the change in the proportion of choices for each dimension at preoperative and final follow-up is demonstrated.
Factors Associated with QoL
In the preoperative mJOA score, the QoL was significantly better for mild (0.84 ± 0.13) and moderate (0.74 ± 0.24) than for severe nerve injury (0.49 ± 0.37). These scores for the VAS scale were 82.67 ± 8.32, 80.16 ± 8.41, and 71.69 ± 11.23. (p < 0.001). The mean score for the QoL and the VAS scale were compared in Table 3 using patients' demographic and clinical characteristics versus the mJOA score. To improve readability, only statistically significant indicators are reported in the table.
| Characteristics | EQ-5D | VAS | |||||
|---|---|---|---|---|---|---|---|
| Severe | Moderate | Mild | Severe | Moderate | Mild | ||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| Sex | Male | 0.63 ± 0.34 | 0.78 ± 0.22 | 0.82 ± 0.15 | 74.52 ± 12.53 | 81.46 ± 7.87 | 79.75 ± 9.65 |
| Female | 0.34 ± 0.35 | 0.68 ± 0.25 | 0.86 ± 0.11 | 68.47 ± 8.90 | 78.38 ± 9.05 | 85.58 ± 5.54 | |
| p-value | 0.012* | 0.137 | 0.239 | 0.132 | 0.162 | 0.049* | |
| Age (years) | ≤ 60 | 0.62 ± 0.41 | 0.87 ± 0.08 | 0.87 ± 0.10 | 82.33 ± 2.52 | 84.00 ± 5.19 | 83.97 ± 7.89 |
| > 60 | 0.42 ± 0.33 | 0.57 ± 0.26 | 0.74 ± 0.17 | 67.47 ± 6.54 | 75.41 ± 9.30 | 78.75 ± 8.70 | |
| p-value | 0.125 | 0.000* | 0.005* | 0.501 | 0.002* | 0.048* | |
| Times of operation | 1 | 0.56 ± 0.30 | 0.76 ± 0.24 | 0.84 ± 0.11 | 72.25 ± 10.58 | 81.15 ± 9.12 | 82.67 ± 8.58 |
| > 1 | 0.38 ± 0.46 | 0.68 ± 0.23 | 0.82 ± 0.20 | 70.75 ± 12.69 | 77.73 ± 6.00 | 82.67 ± 7.57 | |
| p-value | 0.346 | 0.190 | 0.482 | 0.501 | 0.035* | 0.938 | |
| BMI | Normal | 0.66 ± 0.32 | 0.83 ± 0.16 | 0.88 ± 0.07 | 77.00 ± 9.75 | 83.50 ± 6.75 | 83.58 ± 8.67 |
| Overweight | 0.41 ± 0.37 | 0.67 ± 0.26 | 0.82 ± 0.15 | 68.90 ± 11.16 | 77.73 ± 8.79 | 82.16 ± 8.23 | |
| p-value | 0.049* | 0.026* | 0.296 | 0.049* | 0.069 | 0.335 | |
| Duration of symptoms | ≤ 24 | 0.59 ± 0.39 | 0.80 ± 0.18 | 0.83 ± 0.15 | 74.36 ± 10.65 | 82.67 ± 6.22 | 81.34 ± 7.88 |
| > 24 | 0.42 ± 0.35 | 0.68 ± 0.27 | 0.84 ± 0.10 | 69.61 ± 11.54 | 77.90 ± 9.57 | 80.86 ± 9.01 | |
| p-value | 0.235 | 0.149 | 0.686 | 0.156 | 0.141 | 0.045* | |
| Remission of symptoms | No/Worse | 0.42 ± 0.39 | 0.57 ± 0.32 | 0.84 ± 0.12 | 68.13 ± 13.22 | 74.50 ± 9.51 | 84.38 ± 7.02 |
| Yes | 0.55 ± 0.35 | 0.81 ± 0.13 | 0.84 ± 0.13 | 74.82 ± 8.32 | 82.77 ± 6.51 | 82.03 ± 8.76 | |
| p-value | 0.230 | 0.009* | 0.981 | 0.064 | 0.002* | 0.395 | |
| Dural tears | Yes | 0.34 ± 0.31 | 0.60 ± 0.35 | 0.72 ± 0.11 | 65.75 ± 9.94 | 75.13 ± 11.41 | 77.80 ± 8.76 |
| No | 0.54 ± 0.38 | 0.75 ± 0.21 | 0.86 ± 0.12 | 71.75 ± 10.86 | 81.10 ± 7.81 | 83.77 ± 8.51 | |
| p-value | 0.900 | 0.047* | 0.005* | 0.820 | 0.038* | 0.014* | |
| Follow-up times | ≤ 70.8 month | 0.43 ± 0.29 | 0.75 ± 0.21 | 0.83 ± 0.16 | 68.42 ± 6.73 | 80.44 ± 7.45 | 86.95 ± 6.92 |
| > 70.8 month | 0.62 ± 0.32 | 0.60 ± 0.35 | 0.85 ± 0.11 | 69.76 ± 13.14 | 79.41 ± 9.91 | 81.21 ± 8.87 | |
| p-value | 0.347 | 1.000 | 0.853 | 0.026* | 0.804 | 0.014* | |
| Operation | Preop. | 0.13 ± 0.34 | 0.36 ± 0.35 | 0.67 ± 0.22 | 52.00 ± 14.03 | 59.89 ± 14.38 | 69.63 ± 9.80 |
| Postop. | 0.45 ± 0.36 | 0.72 ± 0.25 | 0.84 ± 0.13 | 69.18 ± 10.72 | 79.84 ± 8.86 | 83.19 ± 8.63 | |
| p-value | 0.004* | 0.000* | 0.000* | 0.000* | 0.000* | 0.000* | |
- Note: Bold fonts indicate the part of the p-value < 0.05.
- Abbreviations: BMI, body mass index; mJOA, modified Japanese Orthopaedic Association score; QoL, quality of life.
- † Only statistically significant relevant indicators are shown in the table.
- * Statistically significant at p < 0.05.
In terms of gender, the differences in QoL and VAS scores between males and females overall did not show a statistically significant; however, among patients with severe nerve injury, men showed a higher QoL than women and was statistically significant (p = 0.012).
Both QoL and VAS were significantly lower in elderly patients aged > 60 years with moderate or mild nerve injury than in those ≤ 60 years (p < 0.001).
There was no statistically significant difference between QoL and VAS for patients who had a single procedure compared to those who had multiple procedures; however, in patients with moderate nerve injury, a higher and statistically significant VAS was observed in patients with a single procedure compared to those with multiple procedures (p = 0.035). Although the number of patients with compression in the lower thoracic spine was higher than in the other groups, the differences in QoL and VAS between the different compressed segments and the number of compressed segments were not statistically significant.
There was no statistically significant difference between the QoL and VAS of patients with a Frankel grade of D on admission and those with B/C. No statistically significant differences were found between QoL and VAS in patients with the presence of diabetes and hypertension compared to those without chronic complications.
QoL and VAS were lower in patients with overweight BMI compared to normal patients (p = 0.049), and this difference was more significant in patients with moderate nerve damage (p = 0.026).
In terms of symptom presentation, the difference between their QoL and VAS did not show a statistically significant difference, either in terms of numbness/pain, activity limitation, or both.
The mean VAS was lower in patients with mild nerve injury with a symptom duration > 24 months compared to those with ≤ 24 months (p = 0.045); however, there was no statistically significant difference between the two groups of patients with QoL.
Both QoL and VAS were significantly and statistically higher in patients with moderate nerve injury who had relief of symptoms at hospital discharge than in those with no relief or even worsening of symptoms (p = 0.009, p = 0.002).
In the surgery-related data, QoL (p = 0.047, 0.005) and VAS (p = 0.038, 0.014) were only found to be significantly lower in patients with intraoperative dural tears compared to those without dural tears. No statistically significant results were found in duration of surgery or intraoperative blood loss.
In terms of differences in follow-up time, only a significant difference in reported VAS was found between patients with mild and moderate neurological damage (p = 0.026, p = 0.014), with no statistically significant difference between QoL.
On imaging, as shown in Table 4, QoL and VAS were significantly higher in patients with severe and moderate nerve injury who showed unilateral ossification and bilateral ossification on axial CT than in those with bridging (p = 0.042, p = 0.009). However, the differences between the types of ossification on sagittal MRI were not statistically significant. QoL was significantly higher in patients with ≤ 50% spinal canal occupancy than those with > 50% (p = 0.001). In patients with moderate and mild neurological damage, ISST2I none and fuzzy had higher QoL scores than those with clear spinal cord signal increases (p = 0.008, p < 0.001).
| Characteristics | EQ-5D | VAS | |||||
| Severe | Moderate | Mild | Severe | Moderate | Mild | ||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| Type of ossification (CT) | Unilateral | 0.69 ± 0.32 | 0.81 ± 0.14 | 0.83 ± 0.19 | 76.50 ± 11.60 | 81.80 ± 6.18 | 85.00 ± 8.55 |
| Bilateral | 0.66 ± 0.33 | 0.84 ± 0.08 | 0.84 ± 0.11 | 81.75 ± 9.74 | 84.08 ± 3.73 | 82.82 ± 7.16 | |
| Bridging | 0.35 ± 0.36 | 0.61 ± 0.30 | 0.84 ± 0.12 | 66.78 ± 8.90 | 76.19 ± 10.50 | 81.00 ± 9.73 | |
| p-value | 0.042* | 0.049* | 0.541 | 0.009* | 0.047* | 0.365 | |
| Type of ossification (MRI) | Round | 0.56 ± 0.36 | 0.68 ± 0.25 | 0.86 ± 0.10 | 70.67 ± 12.46 | 78.95 ± 9.60 | 83.19 ± 7.35 |
| Beak | 0.45 ± 0.38 | 0.79 ± 0.22 | 0.82 ± 0.15 | 72.30 ± 10.72 | 81.37 ± 7.07 | 82.26 ± 9.13 | |
| p-value | 0.659 | 0.080 | 0.801 | 0.774 | 0.325 | 0.566 | |
| ISST2I | None | 0.53 ± 0.41 | 0.89 ± 0.06 | 0.92 ± 0.04 | 77.00 ± 8.58 | 84.67 ± 6.22 | 86.28 ± 5.22 |
| Fuzzy | 0.70 ± 0.33 | 0.77 ± 0.21 | 0.84 ± 0.13 | 72.89 ± 14.29 | 81.33 ± 7.16 | 81.15 ± 8.44 | |
| Clearly | 0.37 ± 0.35 | 0.63 ± 0.27 | 0.75 ± 0.14 | 69.18 ± 10.07 | 76.94 ± 9.24 | 81.21 ± 9.95 | |
| p-value | 0.140 | 0.008* | 0.000* | 0.263 | 0.065 | 0.170 | |
| Occupancy rate (CT) | ≤ 50% | 0.70 ± 0.24 | 0.82 ± 0.14 | 0.86 ± 0.12 | 72.30 ± 12.33 | 82.23 ± 5.07 | 83.16 ± 7.00 |
| > 50% | 0.25 ± 0.32 | 0.56 ± 0.30 | 0.77 ± 0.14 | 67.42 ± 8.06 | 75.67 ± 12.13 | 80.80 ± 12.66 | |
| p-value | 0.001* | 0.005* | 0.037* | 0.169 | 0.100 | 0.475 | |
| Occupancy rate (MRI) | ≤ 50% | 0.70 ± 0.30 | 0.86 ± 0.09 | 0.88 ± 0.08 | 74.27 ± 13.39 | 83.53 ± 5.11 | 84.09 ± 7.44 |
| > 50% | 0.39 ± 0.37 | 0.62 ± 0.28 | 0.74 ± 0.16 | 70.33 ± 10.02 | 76.79 ± 9.76 | 79.53 ± 9.50 | |
| p-value | 0.025* | 0.001* | 0.001* | 0.271 | 0.020* | 0.100 | |
- Note: Bold fonts indicate the part of the p-value < 0.05.
- Abbreviations: ISST2I, increased signal on Sagittal T2-weighted images; mJOA, modified Japanese Orthopaedic Association score; QoL, quality of life.
- * Statistically significant at p < 0.05.
As shown in Tables 5 and 6, each reported problem (percentage) by the patients was assessed in terms of their demographic and clinical characteristics. In the mobility dimension, more problems were observed in the 60+ age group (75.5%), Frankel B/C (66.7%), no relief or even worsening of symptoms (62.5%), comorbid diabetes mellitus (75.0%), hypertension (61.9%), the main symptom was numbness and pain with activity limitation (63.2%), intraoperative blood loss > 450 mL (61.5%), Intraoperative dural tears (80.0%), axial CT ossification type is bridging (66.0%), occupancy rate (CT) > 50% (71.8%), occupancy rate (MRI) > 50% (69.1%), ISST2I clear (72.9%). In the self-care dimension, more problems were reported in the 60+ age group (57.1%), multiple operations (50.0%), Frankel B/C (46.2%), no relief or even worsening of symptoms (52.5%), comorbid diabetes mellitus (55.6%), hypertension (45.2%), duration of symptoms > 24 months (42.1%), intraoperative blood loss > 450 mL (42.3%), bridging type of axial CT ossification (48.0%), occupancy rate (CT) > 50% (56.4%), occupancy rate (MRI) > 50% (52.7%), ISST2I clear (50.0%). In the usual activities dimension, more problems were declared in the 60+ age group (87.8%); the main symptom was activity limitation (66.7%), occupancy rate (CT) > 50% (74.4%), occupancy rate (MRI) > 50% (81.8%), ISST2I clear (77.1%). In the pain/discomfort dimension, more problems were observed in single operation (91.9%), compression of lower thoracic vertebral segments (95.0%), no relief or even worsening of symptoms (93.6%), overweight (93.2%), main symptoms are numb/pain (90.0%), intraoperative blood loss > 450 mL (73.1%), axial CT ossification type is bilateral and bridging (92.1%, 92.0%), ISST2I clear (91.7%). Finally, in the anxiety/depression dimension, more problems were reported by > 60 years old patients (81.6%), diabetes (86.1%), duration of symptoms > 24 months (68.4%), intraoperative blood loss > 450 mL (69.2%), dural tears (92.0%), occupancy rate (MRI) > 50% (80.0%), occupancy rate (CT) > 50% (79.5%), ISST2I clear (77.1%).
| Variable | Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % of any problem | p-value | % of any problem | p-value | % of any problem | p-value | % of any problem | p-value | % of any problem | p-value | ||
| Sex | Female | 50.9 | 0.721 | 38.2 | 0.194 | 63.6 | 0.870 | 87.3 | 0.476 | 60.0 | 0.753 |
| Male | 47.6 | 27.0 | 65.1 | 82.5 | 57.1 | ||||||
| Age (years) | ≤ 60 | 30.4 | <0.001 | 14.5 | <0.001 | 47.8 | <0.001 | 84.1 | 0.805 | 42.0 | <0.001 |
| > 60 | 75.5 | 57.1 | 87.8 | 85.7 | 81.6 | ||||||
| Number of operations | 1 | 45.3 | 0.175 | 25.6 | 0.012 | 62.8 | 0.548 | 91.9 | 0.001 | 54.7 | 0.167 |
| > 1 | 59.4 | 50.0 | 68.8 | 65.6 | 68.8 | ||||||
| Compressed Segments | Upper/Mid | 57.9 | 0129 | 42.1 | 0.525 | 57.9 | 0.799 | 47.4 | 0.003 | 68.4 | 0.297 |
| Lower | 40.0 | 28.3 | 65.0 | 95.0 | 51.7 | ||||||
| Series | 59.0 | 33.3 | 66.7 | 87.2 | 64.1 | ||||||
| Number of compressed segments | ≤ 3 | 46.1 | 0.365 | 34.2 | 0.530 | 68.4 | 0.221 | 86.8 | 0.567 | 56.6 | 0.574 |
| > 3 | 54.8 | 28.6 | 57.1 | 81.0 | 61.9 | ||||||
| Frankel grade | B/C | 66.7 | 0.007 | 46.2 | 0.023 | 71.8 | 0.239 | 82.1 | 0.682 | 69.2 | 0.096 |
| D | 40.5 | 25.3 | 60.8 | 86.1 | 53.2 | ||||||
| Remission of symptoms | No/Worse | 62.5 | 0.038 | 52.5 | 0.001 | 75.0 | 0.085 | 93.6 | <0.001 | 70.0 | 0.069 |
| Yes | 42.3 | 21.8 | 59.0 | 67.5 | 52.6 | ||||||
| Complications | Diabetes | 75.0 | <0.001 | 55.6 | 0.001 | 75.0 | 0.111 | 63.9 | <0.001 | 86.1 | <0.001 |
| Hypertension | 61.9 | 0.039 | 45.2 | 0.024 | 66.7 | 0.703 | 71.4 | 0.003 | 69.0 | 0.083 | |
| BMI | Normal | 36.4 | 0.032 | 25.0 | 0.197 | 47.7 | 0.004 | 70.5 | 0.001 | 54.5 | 0.504 |
| Overweight | 56.8 | 36.5 | 74.3 | 93.2 | 60.8 | ||||||
| Duration of symptoms | ≤ 24 | 45.9 | 0.465 | 23.0 | 0.026 | 60.7 | 0.379 | 83.6 | 0.722 | 49.2 | 0.034 |
| > 24 | 52.6 | 42.1 | 68.4 | 86.0 | 68.4 | ||||||
| Main symptoms | Numb/pain | 30.0 | 0.006 | 12.5 | 0.005 | 47.5 | 0.018 | 90.0 | <0.001 | 50.0 | 0.264 |
| Immobility | 47.6 | 42.9 | 66.7 | 38.1 | 71.4 | ||||||
| Above | 63.2 | 42.1 | 75.4 | 98.2 | 59.6 | ||||||
| Duration of surgery | ≤ 200 min | 44.1 | 0.271 | 25.4 | 0.117 | 62.7 | 0.702 | 88.1 | 0.308 | 50.8 | 0.094 |
| > 200 min | 54.2 | 39.0 | 66.1 | 81.4 | 66.1 | ||||||
| Intraoperative blood loss | ≤ 450 mL | 39.4 | 0.017 | 24.2 | 0.038 | 62.1 | 0.561 | 93.3 | 0.002 | 50.0 | 0.036 |
| > 450 mL | 61.5 | 42.3 | 67.3 | 73.1 | 69.2 | ||||||
| Dural tears | Yes | 80.0 | 0.001 | 60.0 | 0.854 | 88.0 | 0.725 | 84.0 | 0.907 | 92.0 | <0.001 |
| No | 40.9 | 53.8 | 68.1 | 84.9 | 49.5 | ||||||
| Follow-up time | ≤ 70.8 month | 54.3 | 0.369 | 41.3 | 0.092 | 69.6 | 0.352 | 89.1 | 0.292 | 52.2 | 0.269 |
| > 70.8 month | 45.8 | 26.4 | 61.1 | 81.9 | 62.5 | ||||||
| Operation | Preop. | 79.7 | <0.001 | 50.0 | <0.001 | 84.7 | <0.001 | 81.4 | 0.516 | 66.9 | 0.166 |
| Postop. | 49.2 | 32.2 | 64.4 | 84.7 | 58.5 | ||||||
- Note: Bold fonts indicate the part of the p-value < 0.05.
| Variable | Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % of any problem | p-value | % of any problem | p-value | % of any problem | p-value | % of any problem | p-value | % of any problem | p-value | ||
| Type of ossification (CT) | Unilateral | 43.3 | 0.005 | 36.7 | <0.001 | 53.3 | 0.073 | 63.3 | 0.001 | 60.0 | 0.009 |
| Bilateral | 31.6 | 7.9 | 57.9 | 92.1 | 39.5 | ||||||
| Bridging | 66.0 | 48.0 | 76.0 | 92.0 | 72.0 | ||||||
| Type of ossification (MRI) | Round | 46.2 | 0.563 | 36.5 | 0.371 | 63.5 | 0.849 | 80.8 | 0.286 | 59.6 | 0.823 |
| Beak-shaped | 51.5 | 28.8 | 65.2 | 87.9 | 57.6 | ||||||
| Occupancy rate (MRI) | ≤ 50% | 31.7 | <0.001 | 14.3 | <0.001 | 49.2 | <0.001 | 82.5 | 0.476 | 39.7 | <0.001 |
| > 50% | 69.1 | 52.7 | 81.8 | 87.3 | 80.0 | ||||||
| Occupancy rate (CT) | ≤ 50% | 38.0 | 0.001 | 20.3 | <0.001 | 59.5 | 0.113 | 86.1 | 0.567 | 48.1 | 0.001 |
| > 50% | 71.8 | 56.4 | 74.4 | 82.1 | 79.5 | ||||||
| ISST2I | None | 24.1 | <0.001 | 17.2 | 0.003 | 41.4 | 0.006 | 72.4 | 0.074 | 37.9 | 0.002 |
| Fuzzy | 39.0 | 22.0 | 65.9 | 85.4 | 51.2 | ||||||
| Clearly | 72.9 | 50.0 | 77.1 | 91.7 | 77.1 | ||||||
- Note: Bold fonts indicate the part of the p-value < 0.05.
- Abbreviation: ISST2I, increased signal on Sagittal T2-weighted images.
Regression Analysis
In the logistic regression model, after the dependent variable for each domain was dichotomized, the relevant variables (as referred to in the statistical analysis in the methods section) were analyzed with the regression model. To make the results easier to understand, only those variables that were significantly related to any of the domains in EQ-5D-5 L are reported in Table 7. Indeed age (OR = 22.288, CI: 3.328–95.250), diabetes (OR = 7.003 CI: 1.148–42.724), the main symptom is activity limitation (OR = 3.2 CI: 0.8–12.1), mJOA scores (OR = 3.746 CI: 0.532–26.369), dural tears (OR = 20.560 CI: 14.960–82.497) in mobility dimension, age (OR = 87.951, CI: 2.318–152.959), activity limitation (OR = 19.643, CI: 2.650–145.297), mJOA scores (OR = 201.857 CI: 2.855–171.854) in the self-care dimension showed a significant correlation with the QoL, while age (OR = 13.308, CI: 1.944–48.370) and BMI (OR = 5.976, CI: 1.231–29.016), mJOA scores (OR = 16.532 CI: 1.819–150.209) in the usual activities and diabetes (OR = 13.021, CI: 1.526–111.128), occupancy rate (MRI) (OR = 22.813, CI: 2.270–229.276), mJOA scores (OR = 10.592 CI: 0.832–134.862), dural tears (OR = 24.503 CI: 1.621–370.389), showed a significant correlation in the anxiety/depression dimension.
| Characteristic | B | SE | p-value | Odds ratio | CI 95% (Exp B) | |
|---|---|---|---|---|---|---|
| Mobility | Age group | 3.176 | 0.944 | 0.001 | 22.288 | 3.328–95.250 |
| Dural tears | 3.023 | 1.337 | 0.024 | 20.560 | 14.960–82.497 | |
| Diabetes | 1.946 | 0.923 | 0.035 | 7.003 | 1.148–42.724 | |
| Activity limitation | 1.789 | 0.682 | 0.039 | 2.956 | 0.577–15.141 | |
| ISST2I | 2.609 | 1.065 | 0.014 | 13.590 | 1.687–98.448 | |
| mJOA | 1.150 | 0.794 | 0.048 | 3.746 | 0.532–26.369 | |
| Self-care | Age group | 5.236 | 2.243 | 0.020 | 87.951 | 2.318–152.959 |
| Activity limitation | 7.583 | 3.372 | 0.025 | 19.643 | 2.650–145.297 | |
| mJOA | 5.308 | 2.173 | 0.015 | 201.857 | 2.855–171.854 | |
| Usual activities | Age group | 2.588 | 0.981 | 0.008 | 13.308 | 1.944–48.370 |
| BMI | 1.788 | 0.806 | 0.027 | 5.976 | 1.231–29.016 | |
| mJOA | 2.805 | 1.126 | 0.013 | 16.532 | 1.819–150.209 | |
| Anxiety/depression | Diabetes | 2.567 | 1.094 | 0.019 | 13.021 | 1.526–111.128 |
| Occupancy rate (MRI) | 3.127 | 1.177 | 0.008 | 22.813 | 2.270–229.276 | |
| mJOA | 2.360 | 1.298 | 0.039 | 10.592 | 0.832–134.862 | |
| Dural tears | 3.199 | 1.386 | 0.021 | 24.503 | 1.621–370.389 | |
| EQ-5D-5L Value set | Age group | 9.841 | 4.786 | 0.040 | 18.785 | 1.585–22.260 |
| Occupancy rate (MRI) | 2.720 | 1.998 | 0.003 | 15.178 | 1.302–61.719 | |
| ISST2I | 11.450 | 4.158 | 0.006 | 62.699 | 17.097–140.028 | |
| mJOA | 3.997 | 2.263 | 0.007 | 54.410 | 16.460–90.985 | |
| BMI | 6.998 | 3.165 | 0.027 | 84.036 | 2.193–329.605 |
- Abbreviations: BMI, body mass index; ISST2I, increased signal on Sagittal T2-weighted Images; mJOA, modified Japanese Orthopaedic Association score; TOLF, thoracic ossification of the ligamentum flavum.
In terms of overall QoL, age (OR = 18.785 CI: 1.585–22.260), occupancy rate (MRI) (OR = 15.178 CI: 1.302–61.719), ISST2I (OR = 62.699 CI: 17.097–140.028), mJOA scores (OR = 54.410 CI: 16.460–90.985), BMI (OR = 84.036 CI: 2.193–329.605) showed a significant correlation.
Discussion
To our best knowledge, the EQ-5D-5L questionnaire is used for the first time in this study to investigate the QoL of TOLF patients after posterior laminectomy. The results showed that the QoL of TOLF patients after surgery was generally satisfactory; however, lower preoperative mJOA scores, advanced age, activity limitation, comorbid diabetes mellitus, high BMI, ISST2I, intraoperative dural tears, and high rate of spinal canal occupancy remained non-negligible risk factors for lower QoL.
QoL Situations
We showed a mean QoL score of 0.71 ± 0.28 and a mean VAS score of 78.88 ± 10.21 at the final follow-up, compared to preoperative, QoL (0.44 ± 0.37) and VAS scale (62.31 ± 14.28) are significantly improved. However, given that EQ-5D value sets are different by country and region and that there is variation between different versions of the studies in the same area, meanwhile, the relatively subjective results of EQ-VAS scores are influenced by the length of follow-up, it is essential to take this variation into account when referring to or comparing QoL scores, especially the VAS score results, and to interpret the results more cautiously.
Preoperatively, we found that the majority of patients reported moderate to severe difficulties with mobility, usual activities, anxiety/depression, and pain/discomfort; however, at the time of the final follow-up, most patients were significantly improved and did not report any difficulties or reported only minor difficulties in some dimensions, but problems in usual activities, pain/discomfort, and mobility are more common above the moderate level than in other dimensions. Many studies have reported that numbness/pain in both lower extremities and impaired mobility are often the main symptoms of patients with TOLF at the time of presentation and that sensory and motor deficits in the lower extremities are often the main challenges faced by patients with TOLF.17 Our study also confirmed that most patients continued to have moderate to severe problems with mobility, pain/discomfort, despite successful surgery to relieve spinal cord compression long afterward; however, surgical release of spinal cord compression remains the only effective treatment that provides opportunities for patients to recover neurological function and improve QoL.
Risk Factors
Age and Preoperative mJOA Score
In our study, QoL and VAS are significantly lower in patients with more severe neurological impairment, in advanced age, and patients with no relief or even worsening of symptoms at hospital discharge. Severe neurological impairment of the spinal cord is irreversible. The mJOA score provides a general indication of the extent of spinal cord injury by assessing sensory and motor function in both lower limbs; Zhang et al.8 classified 165 postoperative TOLF patients into four grades of excellent (75%–100%), good (50%–74%), mediocre (25%–49%), and poor (0%–24%) by recover rate and analyzed the associated risk factors and found that low preoperative mJOA score was an independent risk factor for poor prognosis, Consistent with our findings. However, despite the fact that patients with lower mJOA scores had poorer QoL, patients with the same degree of neurological impairment still showed a significant improvement in QoL after surgery compared with the preoperative period; therefore, we recommend that patients with severe neurological impairment should still be operated aggressively. Whether the neurological impairment is mild or moderate, the QoL is significantly poorer in seniors, and the majority of older patients have difficulties with pain/discomfort, usual activities, and anxiety/depression dimensions, in line with results reported in other studies.1 A retrospective study by Yamada et al.18 61 patients with TOLF who underwent surgery found no statistically significant association between the previously mentioned factors with poor prognosis. However, age showed a significant correlation. In another study, Wu et al.19 assigned a TOLF score of 1 to patients <50 years old, 2 to patients 50–60 years old, and 3 to patients > 60 years old and showed that younger patients have better spinal cord plasticity, more metabolically active organ systems, better cognitive function abilities and shorter recovery times. In terms of QoL, older patients, who tend to be affected by multiple illnesses, social and family support aspects, are more sensitive to sensory-motor dysfunction and often tend to report poorer QoL. At the time of discharge, the patient was physically examined, and if there was no significant improvement in sensory or motor function from the preoperative period is defined as no relief of symptoms. The lack of relief or even worsening of symptoms represents a limited recovery of spinal cord function, and more patients have difficulty with both usual activities and pain/discomfort dimensions in the distant postoperative period, especially pain/discomfort, with a problem feedback rate of 93.6%. Previous studies have indicated that approximately 60%–80% of spinal cord injury patients have long-term chronic pain with implications for QoL and neurological recovery.20 Long-term and comprehensive pain management is essential to improve QoL. The analysis of the regression model revealed that the age and mJOA score variables are significantly correlated with mobility, self-care, usual activities, and EQ-5D-5L value set, which represents overall QoL, the mJOA score also correlates with anxiety/depression dimensions. Older or severe neurological impairment patients have lower QoL than younger or mild neurological impairment patients in each of these dimensions. And age also has the highest correlation with the self-care dimension. So we still need to focus on older patients and those with severe spinal cord neurological impairment. This is because these patients may still have difficulties with, for example, self-care long after successful surgical decompression.
Gender and BMI
We also found that QoL was significantly higher in men than women in patients with severe neurological impairment; it is possible that women tend to have a higher propensity to express health-related problems. However, gender did not show a significant correlation with any of the dimensions in the regression model, and similar to the results of other studies, gender was not associated with overall QoL outcomes.
In our study, no patient had a BMI of less than 18.5, 44 had BMI in the normal range, and 74 were overweight. Meanwhile, in patients with severe and moderate neurological injuries, overweight patients had a significantly lower QoL. Tang et al.21 reported that OLF formation was associated with high BMI and that the size and progression of the ossified mass were associated with high BMI and smoking. High BMI is not only associated with TOLF but is also more likely to be comorbid with a variety of other chronic diseases, affecting patients' QoL in many ways. In regression analyses, high BMI is highly correlated with both the Usual activities dimension and overall QoL, similar to the results of other studies.22, 23 Therefore, for overweight as well as obese patients, there is an obligation to inform the patient that the long-term QoL after surgery may still be less satisfactory.
Follow-up Time
Previous retrospective studies on postoperative neurological recovery in TOLF patients have rarely been analyzed concerning follow-up time.18, 24 Similarly, few studies have focused on the long-term QoL of TOLF patients after surgery; in a study of long-term QoL after posterior decompression via an uni-or bilateral approach in patients with degenerative thoracic spinal stenosis, Siller et al.25 reported that 645 patients with surgery for degenerative spondylotic myelopathy within 6 years were followed up for an average of 35.1 months and did not suggest that differences in length of follow-up were significantly correlated with QoL. Our study showed that, grouped by a mean follow-up time of 70.8 months, the difference between the relatively longer and relatively shorter follow-up groups was not statistically significant on the EQ-5D-5L value set, and a difference was found only on the EQ-VAS. The EQ-VAS scores represent the patient's perspective and are strongly subjective. In contrast, most of the set of utility value sets represent society's research perspective (i.e., the value of this state of health as judged by the general population) and are relatively objective; similarly, mJOA scores are strongly correlated with EQ-5D-5L value sets results, and we, therefore, consider that patients' outcomes in the five dimensions as well as in overall QoL are primarily influenced by neurological functioning. According to other reports, neurological recovery in thoracic spondylotic myelopathy is slow, peaking 9–12 months after surgery, and the rate of neurological recovery tends to stabilize after 1 year.26 Therefore, we believe that the QoL outcomes of patients evaluated by the EQ-5D-5L scale are relatively objective and less affected by the duration of follow-up; however, the EQ-VAS results, which are strongly subjective, should be analyzed with caution. For the times of operation and the duration of symptoms, statistically significant differences were observed only on the EQ-VAS, which is less informative.
Dural Tears
In surgery-related data, a significantly lower QoL was found in patients with mild/moderate nerve injuries with dural tears only. Tang et al.27 concluded that dural tears are an important risk factor for postoperative neurological complications and predict postoperative neurological recovery. In our study, all 18 patients (15.3%) with neurological deterioration in the immediate postoperative period had intraoperative dural tears. Dural adhesions are common in patients with TOLF and are one of the most critical factors leading to dural tears, the most extreme manifestation of which is dural ossification (DO). Adhesions and ossification are produced by chronic and severe compression, so that dural tears indicate not only surgical complications but also long-term damage to the neural tissue. Muthukumar et al.28 suggested that the comma sign and the tram-track sign on the bone window of axial CT scans could identify dural ossification; Zhai et al.29 found that cerebrospinal fluid cross-sectional area is valuable in diagnosing DO. Baker et al.30 concluded that revision surgery, advanced age, degenerative disease are important risk factors for dural tears. These factors contribute to early recognition of DO and remind intraoperative efforts to reduce dural tears through more careful manipulation. However, these dural changes suggest a more demanding surgical technique with a higher risk of neurological complications. In regression analyses, dural tears were significantly associated with the mobility, anxiety/depression dimensions and not with overall Qol. In a retrospective study of postoperative satisfaction in 57 TOLF patients, DO and dural tearing were significant factors in patient dissatisfaction with postoperative outcomes.31 We consider that cerebrospinal fluid leakage from dural tears often results in prolonged hospitalization and increased treatment costs, while the adverse experience of increased surgical complications adds to the patient's anxiety about the condition. Therefore, more attention needs to be paid to patients with dural tears, not only to avoid neurological complications as much as possible but also to provide more comfort and education to patients to ease their anxiety about their health status.
Imaging Information
In terms of imaging performance, our findings indicate that QoL and VAS are significantly lower in patients with severe and moderate nerve injury who exhibit a bridging pattern on axial CT scans than in both unilateral and bilateral patterns; on sagittal MRI scans; however, the difference between round and beak shapes is not significant, and past studies have shown that the unilateral type has a better postoperative recovery outcome, with the bilateral and bridging types being important independent risk factors for poor prognosis.8 We believe that the shape of the bridging ossified mass often results in extensive compression of the posterior aspect of the spinal cord, which can have a greater impact on spinal cord neurological function.
In addition, QoL and VAS are significantly lower in patients with > 50% spinal canal occupancy on both CT and MRI than in patients with ≤ 50% occupancy, which is consistent with some previous studies that concluded that spinal canal occupancy on MRI showed a significant correlation with anxiety/depression aspects in regression models.32 Therefore, we still need to care more for patients with severe spinal canal occupancy.
Meanwhile, ISST2I showed significant differences in QoL in patients with moderate/mild neurological injury, with significantly lower QoL in patients with strongly and clear increased spinal cord signal, and showed significant correlation with the mobility dimension in regression models. It with intramedullary signal alterations, non-specific neuronal cell death, gliosis, spinal cord white and gray matter edema, Wallerian degeneration, and demyelination.33 Most scholars agree that intramedullary signal alterations mark irreversible pathological changes in the spinal cord and are of great value in assessing postoperative prognosis,15 which is consistent with our results.
It is also worth noting that patients reported mild to severe problems most frequently in the dimension of pain/discomfort out of the five dimensions, so proper pain management in the long-term postoperative period and symptomatic medication remains important. At the same time, we found that patients with preoperative activity limitations reported more difficulties in mobility and self-care dimensions, and there was a correlation. Similar to our results, Tang et al.27 reported that the preoperative walking score is a good predictor of postoperative activity function. The walking score is a simple system for evaluating mobility, which is the most bothersome symptom affecting patients' daily functioning, and the recovery of mobility is affected by a variety of factors, especially in patients with severe neurological impairments, where recovery of mobility is usually limited. Therefore, patients with severe mobility limitations should be adequately informed preoperatively that they may still have mobility and self-care difficulties in the distant postoperative period. However, this concept can only be validated by prospective studies.
Overall, patients with more severe nerve injuries, higher age, and thorough surgical decompression showing no relief or even worsening of symptoms, high BMI, presence of intraoperative dural tears, CT axial ossification type showing bridging, strongly and clear increased spinal cord signal, and vertebral canal occupancy greater than 50% had a lower overall QoL. Among them, age, dural tear, comorbid diabetes mellitus, presence of activity limitation, ISST2I, preoperative mJOA score, BMI, and vertebral canal occupancy rate have significant correlations with their corresponding dimensions and are predictive. Age, vertebral canal occupancy rate, ISST2I, preoperative mJOA score, and BMI are closely correlated with, and predictive of, overall QoL. In contrast, no statistically significant differences are seen in the number of operations, compressed segments, Frankel grade, comorbid hypertension, duration of symptoms, duration of surgery, intraoperative blood loss, or MRI sagittal ossification patterns, and no significant correlation with QoL was found.
Limitation and Strengths
This is the first study to use the EQ-5D-5L questionnaire to investigate the postoperative QoL of TOLF patients, filling a gap in the postoperative QoL situation of TOLF patients. At the same time, we analyzed the risk factors associated with poor QoL, which helps surgeons predict the prognosis of patients before surgery.
There are still some limitations in this study: this is a single-center study, so our findings are not representative of all TOLF patients in the region. Relevant demographic and clinical characteristics, and imaging data, were retrospectively collected from the patient's case histories and medical records, which are subject to some bias because they are past data. We ended up with only 118 of 181 TOLF patients who underwent posterior laminectomy entered this study through the inclusion–exclusion criteria; for some variables, a larger sample size is still required. Although in the present study, we initially analyzed the effect of differences in follow-up time on QoL and only found relatively subjective EQ-VAS results to be more strongly influenced by follow-up time and interpreted the EQ-VAS results more cautiously; however, only QoL data from regular follow-up can more accurately exclude the interference of follow-up time, which was a shortcoming of this our study. Also, as this is a retrospective study, the associations we observed are not necessarily causal, and the results still need to be analyzed with caution.
Conclusion
QoL after posterior laminectomy in TOLF patients is generally satisfactory, with most patients reporting no difficulties or only minor difficulties in some dimensions; however, problems with usual activities, pain/discomfort and mobility are more common above the moderate level than in other dimensions. The QoL of TOLF patients after surgery is influenced by age, preoperative mJOA score, symptom relief at hospital discharge, BMI, intraoperative dural tears, type of ossification on axial CT scan, ISST2I, and spinal canal occupancy rate. Meanwhile, preoperative mJOA score, age, comorbid diabetes, presence of activity limitation, BMI, dural tears, ISST2I, and spinal canal occupancy rate (MRI) are significantly correlated with the corresponding dimensions and are predictive, age, vertebral canal occupancy rate, ISST2I, preoperative mJOA score, and BMI are in turn closely correlated with, and predictive of, overall QoL. Therefore, preoperative communication should focus on the key factors affecting postoperative QoL in TOLF patients. In the distant postoperative period, there is still a need to focus on patient mobility and pain/discomfort management to better manage patients after posterior laminectomy for TOLF, and ultimately to work toward improving QoL in postoperative TOLF patients.
Conflict of Interest Statement
The authors confirm that they have no conflict of interest with respect to the manuscript content or funding.
Ethics Statement
This retrospective study was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The ethics committee of West China Hospital, Sichuan University approved this study (No. 2023241).
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Junhu Li, Zhipeng Deng and Linnan Wang. The first draft of the manuscript was written by Junhu Li and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding Information
No funding was received for conducting this study.
Authorship Declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors and all authors are in agreement with the manuscript.
Informed Consent
The information relating to the patients are completely anonymized and the submission does not include images that may identify the person.