Minimally Invasive Percutaneous Leverage Reduction in the Treatment of Pediatric Salter–Harris IV and V Distal Femoral Physeal Fractures
Wen Shu and ZiXuan Ou These authors contributed equally to this study and should be considered co-first authors.
Haobo Zhong and Xin Tang contributed equally to this study.
Abstract
Objective
Distal femoral physeal fractures (DFPF) are rare but severe injuries in children, and there is no consensus on treatments for Salter–Harris (S–H) IV and V type of DFPF yet. This study aimed to introduce a minimally invasive technique using percutaneous leverage reduction combined with Kirschner wires fixation in treating pediatric DFPF with S–H IV and V type of injury and evaluate the clinical results.
Methods
From July 2008 to June 2018, the authors' institute (Union Hospital, Tongji Medical College) retrospectively reviewed all patients diagnosed with pediatric DFPF. They were divided into two groups according to received treatment: children in the minimally invasive technique group were treated with a minimally invasive percutaneous leverage reduction technique, and the traditional technique group included the other children who received the conventional open reduction with internal fixation (ORIF). The surgical and clinical results of the two groups were collected and analyzed. The independent sample t-test analysis and the chi-square test were applied to compare continuous and categorical variables.
Results
A total of 14 pediatric patients were recruited, including five females and nine males with DFEF. All eight patients in the minimally invasive technique group and four of the six patients in the ORIF group were treated successfully. One patient in the minimally invasive technique group opted for conservative treatment due to his good functional recovery, while the other two patients in the ORIF group needed further surgery because of the limb length discrepancy. There was a difference in surgery duration (p < 0.001), intraoperative fluoroscopy numbers (p = 0.006), intraoperative blood loss (p < 0.001), radiological union time (p = 0.003) and knee flexion angle (p < 0.001) between two groups. Patients in the minimally invasive technique group all received total knee society (KSS) scores, while the average scores in the ORIF group were lower (100.00 vs. 97.67).
Conclusion
The minimally invasive technique is better than conventional ORIF in terms of surgery duration, intraoperative blood loss, radiological union time, knee flexion angle and average KSS score. This percutaneous leverage reduction technique might be a good alternative for treating S–H IV and V DFPF in children.
Introduction
Distal femoral physeal fractures (DFPF) are rare in the pediatric population, accounting for 1% of all fractures and 6% to 9% of physeal injuries.1-3 Despite the low incidence of such fractures, children who suffered DFPF are at high risk of limb length discrepancy or angular deformity. The risk might be high because the distal femoral epiphysis has the most significant potential for longitudinal growth of any long bone, contributing 70% of femoral growth and 35% of overall lower limb length growth.4 A fracture of the distal femoral epiphysis may affect the popliteal artery as the femoral artery passes medially above the epiphysis through the adductor canal and travels in the popliteal fossa. Swelling, pain and limited joint movement also usually occur after the fracture. Therefore, choosing an appropriate treatment for DFPF is challenging for pediatric orthopedic surgeons.5, 6
The Salter–Harris (S–H) classification system, ranging from type I to V based on the mechanism of injury and the relationship of the fracture line to the growth plate, is clinically used for DFPF.7, 8 Type IV and V fractures refer to an intra-articular fracture involving the epiphysis, physis, metaphysis and compression on the growth plate respectively.9 These two types of physeal fractures are currently recommended for surgical treatments to achieve satisfactory reduction. Open reduction internal fixation (ORIF) is the most commonly used surgical treatment. However, ORIF might affect the blood supply to the epiphysis, resulting in premature physeal closure and even growth arrest.10 Closed reduction and percutaneous pinning (CRPP) is another treatment option for type IV and V fractures, which has the advantage of less trauma and blood loss.11, 12 Patients with pediatric DFPF undergoing closed reduction surgery had superior functional results to patients who received ORIF in long-term follow-up.13 However, CRPP is hard to perform and achieve satisfactory reduction, especially in severely displaced fractures such as S–H IV and V injuries. The treatment methods of these two types of pediatric DFPF remain controversial. In order to achieve satisfactory reduction but avoiding the shortcomings of the ORIF technique, we introduced a minimally invasive technique. This technique not only showed advantage in achieving satisfactory reduction compare with CRPP, but also would be better than conventional ORIF in terms of surgery duration and clinical outcome.
This study aimed to: (i) introduce a minimally invasive technique that combined percutaneous leverage reduction with Kirschner wires fixation in treating S–H IV and V pediatric DFPF; and (ii) compare and evaluate the clinical results between the novel technique and the traditional ORIF technique.
Methods
From July 2008 to June 2018, patients diagnosed with distal femoral physeal fractures (DFPF) in the authors' institute (Union Hospital, Tongji Medical College) were retrospectively reviewed. The demographic and clinical data were recorded from medical records, including the patient's age, gender, AO/OTA classification, S–H classification, and operation-related information.
The inclusion criteria were: (i) patients' age less than 15 years; (ii) diagnosed as S–H IV and V type of physeal injury and confirmed on radiographs; (iii) having a follow-up period of at least 24 months; and (iv) receiving the minimally invasive percutaneous leverage reduction technique or conventional ORIF technique. Patients with: (i) systemic disease or medical condition that cannot tolerate anesthesia; (ii) congenital anomalies of the femur or previous fractures of the femur; and (iii) incomplete medical records were excluded.
All the patients were divided into two groups according to the treatment they received: the minimally invasive technique group or the conventional ORIF group. The ethical review board of the corresponding author's institution approved the study (IORG0003571). All legal guardians of the patients gave informed consent to participate in this study and chose one surgical approach after explaining the pros and cons and potential complications of the two methods. All patients’ operations were performed by the same surgical team.
Surgical Techniques
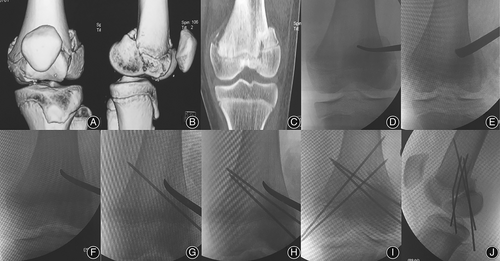
All surgeries were performed under general anesthesia with patients in the supine position, and the operating field was routinely disinfected and covered with sterile towels. Orthopedic traction bed was lacking in the authors' institute (Union Hospital, Tongji Medical College) and all surgeries were performed by the same surgeon. In the minimally invasive technique group, a medium-sized vascular clamp was used to separate the soft tissue through a 1.5 cm lateral skin incision. The clamp is located at the distal femoral fracture block and the metaphysis junction. Then a 1.8 cm wide periosteal stripper was placed through the previous soft tissue channel, and inserted into the metaphyseal fracture junction under fluoroscopy (Figure 1D,E). With continuous traction by assistants, the periosteal stripper was pried back to the compression displacement stress to achieve reduction (Figure 1F). The metaphyseal fracture and epiphyseal line should all get reduction under fluoroscopy. With the continuous prying force of the periosteal stripper and traction to maintain the reduction, a 1.5–2.0 mm Kirschner wire was inserted into the distal end of the lateral condylar block under fluoroscopy, through the fracture line and fixed into metaphysis. Another three 1.5–2.0 mm Kirschner wires, two from the medial and one from the lateral on the distal end of the femur condylar, were applied under fluoroscopy (Figure 1G–J). In order to share the soft tissue tension stress and maintain the reduction, an external fixator was placed over the knee joint but away from the fracture area. The Kirschner wires were bent and left outside the skin. After reconfirmation by fluoroscopy, the incision was sutured and covered by a clean dressing.
Patients in the ORIF group got open reduction and Kirschner wire fixation, as described by Edmunds and Nade.14 The distal lateral femoral approach was used to separate the iliotibial bundle and lateral femoral muscle gap to reveal the supracondylar region of the femur. The incision was lengthened toward the distal parapatellar area to reveal the femoral condyles, and the medial and lateral femoral condyles were aligned under direct vision. The proximal end of the femoral metaphyseal could be held with bone-holding forceps to reduce the fracture. After the femoral and joint surface was reduced by traction, four to six 1.5–2.0 mm Kirschner wires were driven from the medial and lateral femoral condyles toward the metaphysis to fix the fracture. After satisfactory reduction was confirmed by C-arm fluoroscopy, the Kirschner wires were bent and buried under the skin. The incision was sutured and protected with a sterile dressing. Finally, an external fixator was placed over the knee joint and away from the fracture area to maintain the reduction effect.
Postoperative Care and Follow-up
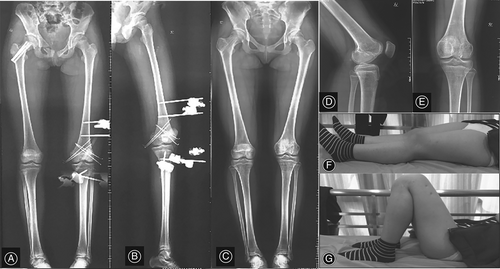
After surgery, the operated lower limb was fixed in plaster at 30° of flexion position. The patients were discharged from the hospital 48 h of post-operation, and their guardians performed daily needle disinfection nursing. After 4 weeks post-operation, the plaster and external fixator were removed, and functional exercise including flexion and knee extension was started. Weight-bearing was allowed after 12 weeks post-operation. Kirschner wires were removed in the clinic at 8 weeks post-operation in the minimally invasive technique group but in the operation room at 6 to 9 months after surgery in the ORIF group. X-ray examination and clinical evaluation were performed 4, 8, 12 weeks, 6, 12, and 24 months after surgery (Figure 2). Clinical outcomes such as union time, knee range of movement (ROM), bilateral limb length differences, and valgus deformity were recorded. The Knee Society Score (KSS) is assessed by a team which was not involved in the treatment of these patients. The radiological standard of fracture healing was defined as blurred fracture lines with continuous callus passing through the fracture lines on X-ray examination.15 Complications such as vascular injury, common peroneal nerve palsy, fracture displacement, and angular deformity were also recorded during the follow-up to skeletal maturity.
Statistical Analysis
SPSS 22.0 statistical software (SPSS Inc., Chicago, Il. USA) was used to analyze all variables. X ± SD was applied to present continuous variables. The independent sample t-test analysis and the chi-square test were used to compare continuous and categorical variables. The level of statistical significance was determined at p < 0.05.
Results
General Results
A total of 14 children, including nine males and five females, were enrolled in this study. The first six patients accepted ORIF treatment before we could perform the minimally invasive technique, while the others were treated with the minimally invasive technique after this technique introduced in our institute (Union Hospital, Tongji Medical College). According to AO/OTA, there were 5, 5, and 3 children classified as B1, B2, or B3 type fractures respectively. There were 10 SH4 and 3 SH5 injuries according to the S–H classification. Only one 12-year-old girl whose was a B1 + B3 fracture and SH4 + SH5 injury (Table 1). There were no significant differences in age, sex, AO/OTA, and S–H classification between the two groups.
| Variables | The minimally invasive technique group | The open reduction internal fixation (ORIF) group | Statistic value. | p-value |
|---|---|---|---|---|
| No. of patients | 8 | 6 | - | |
| Age (year) | 10.75 ± 2.19 | 9.67 ± 1.63 | 1.015 | 0.330 |
| Gender (male/female) | 5/3 | 4/2 | 0.026* | 0.872 |
| AO/OTA classification | 1.478 | 0.687 | ||
| B1 | 3 | 2 | - | |
| B2 | 3 | 2 | - | |
| B3 | 1 | 2 | - | |
| B1 + B3 | 1 | 0 | - | |
| Salter–Harris classification | 1.478 | 0.478 | ||
| SH4 | 6 | 4 | - | |
| SH5 | 1 | 2 | - | |
| SH4 + SH5 | 1 | 0 | - |
- * Significance.
Clinical and Radiological Outcomes
The follow-up results showed that the two groups differed significantly in surgery duration, number of intraoperative fluoroscopies, intraoperative blood loss, and knee flexion angle (Table 2). Patients in the minimally invasive technique group had less surgery duration than children in the ORIF group (47.25 ± 2.12 vs. 57.17 ± 2.56; p < 0.001). During operation, patients in the ORIF group needed fewer fluoroscopy numbers (p = 0.006), but patients in the minimally invasive technique group were with less intraoperative bleeding (11.88 ± 2.59 vs. 45.83 ± 7.36; p < 0.001). Patients in the minimally invasive technique group all got total scores in KSS, while the scores of patients in the ORIF group were lower (100.00 vs. 97.67).
| Variables | The minimally invasive technique group | The ORIF group | Statistic value. | p-value |
|---|---|---|---|---|
| Surgery duration (min) | 47.25 ± 2.12 | 57.17 ± 2.56 | −7.930 | <0.001* |
| Follow-up time (month) | 34.88 ± 6.75 | 50.17 ± 17.45 | −2.035 | 0.087 |
| Number of intraoperative fluoroscopies | 7.467 | 0.006* | ||
| <15 | 0 | 4 | - | |
| ≥15 | 8 | 2 | - | |
| Intraoperative blood loss (mL) | 11.88 ± 2.59 | 45.83 ± 7.36 | −10.812 | <0.001* |
| Radiological healing time (week) | 9.88 ± 1.13 | 12.00 ± 0.89 | −3.799 | 0.003* |
| KSS postoperative score | 100.00 ± 0.00 | 97.67 ± 2.42 | 2.360 | 0.065 |
| Range of movement (°) | ||||
| Flexion | 134.63 ± 3.93 | 123.33 ± 6.06 | 4.244 | <0.001* |
| Extension | 4.38 ± 3.20 | 4.17 ± 2.04 | 0.139 | 0.892 |
| Bilateral limb length difference >2 cm (%) | 1 (12.5) | 2 (33.3) | 0.884 | 0.347 |
| Valgus deformity >5 (%) | 0 (0) | 2 (33.3) | 3.111 | 0.078 |
| Re-operation | 0/8 | 2/6 | 3.111 | 0.078 |
- Abbreviations: KSS, knee society score; ORIF, open reduction internal fixation.
- * Significance.
In addition, patients in the minimally invasive technique group achieved union radiologically earlier (9.88 ± 1.13 vs. 12.00 ± 0.89; p = 0.003), and their knee flexion angle showed a better range also (134.63 ± 3.93 vs. 123.33 ± 6.06; p < 0.001). The two groups have no significant difference between follow-up time (34.88 ± 6.75 vs. 50.17 ± 17.45 months; p = 0.087), knee extension angle, bilateral limb length difference, and valgus deformity.
Complications
There were no infections, neurovascular damage, septic arthritis, popliteal artery injury or compartment syndrome observed in all patients. After skeletal maturity (14–17 years old with the average of 15.8 years old), there was one case with bilateral limb length difference >2 cm but with valgus deformity angle <2° in the minimally invasive technique group. Due to good functional recovery, their caregivers chose an insole to maintain balance without lengthening surgery. In the ORIF group, two patients underwent orthopedic osteotomy to correct the varus or valgus deformity and lengthen the shortened limbs.
Discussion
Pediatric DFPF are rare in the clinic and usually caused by direct violence.5, 6, 16 Distal femur epiphysis has the most significant longitudinal growth potential in long bones, providing 35%–40% of the length of lower limbs. Pediatric DFPF might lead to an unequal length of lower limbs in adults.17 This kind of injury might bring complications such as degenerative osteoarthritis, angulation deformity, knee stiffness, popliteal artery injury and compartment syndrome.18, 19 Orthopedic surgeons should be cautious in treating these kinds of injuries. The goal of DFPF treatment should include trying to maintain anatomical alignment, recovery of the physis and joint line, therefore reducing the risk of growth arrest. Many treatments were currently reported for pediatric DFPF, including conservative and surgical techniques.18, 20, 21 Conservative methods include skin traction and manual reduction, with an extra-knee splint or plaster external fixation.22 However, none of these non-surgical methods could guarantee a satisfactory reduction of the injured epiphysis, which might result in growth arrest. Conservative management of non-displaced fractures is usually acceptable, but surgical treatment is recommended for displaced S–H fractures.23 The appropriate surgical techniques for S–H IV and V injuries remain controversial.
Technique Innovation and Features
In this study, a novel minimally invasive percutaneous leverage reduction technique was adopted. A total of 14 pediatric patients with DFEF, eight were treated with minimally invasive technique and the others with ORIF were recruited. Surgical and clinical results in this study showed that minimally invasive technique is better than conventional ORIF in terms of surgery duration, intraoperative blood loss, radiological union time, knee flexion angle and average KSS score. However, it still needs to be emphasized that the S–H type IV and V DFPF were intra-articular fractures after all, and “zero incision” is not emphasized in the treatment. Open reduction surgery is still a possible option. An external fixator was used in this study to maintain the reduction because the reduction was prone to loosen if only Kirschner wire fixation was used.
Standard surgical methods include CRPP and ORIF.24 Compared with open reduction, the closed reduction might avoid the effect of blood supply and secondary injury to the physeal with better functional recovery of the knee joint, but usually could not achieve a satisfactory reduction.25 Differing from the traditional closed reduction technique, the periosteal stripper in our minimally invasive percutaneous leverage reduction technique was used for additional reduction. Although in manual reduction it is difficult to pull apart the compressed bone mass in pediatric DFPF, the periosteal stripper can achieve a satisfactory reduction. The most significant advantage of ORIF is that this technique could achieve the anatomical reduction of the fracture. The minimally invasive technique in this study showed better clinical results compared with ORIF. The results showed that minimally invasive reduction with shorter operation duration and less intraoperative blood loss than the ORIF. In addition, this technique also has less impact on postoperative ROM of the knee joint and can achieve faster imaging union in this study. Although the proportion of people with bilateral limb size larger than 2 cm and valgus deformity greater than 5° in the ORIF group was larger than that in the closed reduction group, there was no statistical difference due to the small number of participants. These results were consistent with previous literature and showed minimally invasive percutaneous leverage reduction techniques are superior to ORIF.13, 26 This technique also has disadvantages compared with ORIF, such as increasing the risk of X-ray exposure because of more intraoperative fluoroscopy.
However, ORIF might affect the blood supply of the epiphysis and lead to growth arrest. It should be noted that secondary injury to the epiphysis by the periosteal stripper could be avoided. The periosteal stripper should avoid direct contact with the compressed epiphysis. Stress could be conducted on the epiphysis line by reducing the metaphyseal fracture block to achieve reduction of the epiphysis. This study used vascular forceps to separate the soft tissue, which avoided the effect of soft tissue dissection on physeal blood flow in open reduction.27
Limitations and Prospect of this Study
It is undeniable that there are some limitations in this single-center retrospective study. The small sample size limits the statistical power, and the need for more randomization is another shortcoming. Further study with more patients in different institutes are needed in the future. Despite these limitations, this study demonstrated that the minimally invasive percutaneous leverage reduction might be an alternative in treating pediatric S–H type IV and V DFPF and showed good clinical results.
Conclusions
In summary, the minimally invasive technique is better than conventional ORIF in terms of shorter surgery duration, less intraoperative blood loss, faster radiological union time, better knee flexion angle and average KSS score. This percutaneous leverage reduction technique might be a good alternative for treating S–H IV and V DFPF in children.
Conflict of Interest Statement
The authors declare no conflict of interest.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Although the data were collected anonymized and centrally, all guardians of patients signed written informed consent for participate. The Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG No: IORG0003571) gave a final APPROVAL on 20/11/2019 for the study Retrospective Research of Surgical Methods in the Treatment of Fractures and malformation in Children in Children which is conducted by Xin Tang at Department of Orthopedic Surgery, Union Hospital of Tongji Medical College, Huazhong University of Science and Technology.
Author Contributions
Wen Shu and QiYuan Feng were involved in data collection and follow-up assessments. Xin Tang and Wen Shu were responsible for literature search and study design, Haobo Zhong and ZiXuan Ou drafted the manuscript. Xin Tang finalized the manuscript.
Funding Information
This research received no external funding.
Authorship Declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and all authors are in agreement with the manuscript.
Open Research
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.