Postoperative Prevalence and Risk Factors for Serum Hypokalemia in Patients with Primary Total Joint Arthroplasty
Pin Pan and Zitao Zhang contributed equally to this research and share joint first authorship.
Abstract
Objective
Regular monitoring of serum potassium after a total joint arthroplasty (TJA) is a form of routine examination that can help detect abnormal serum potassium levels and reduce the incidences of adverse events that may occur on account of postoperative hypokalemia. Previous studies rarely discussed hypokalemia after joint replacement. In the present study, our primary goal was to investigate the incidence and possible risk factors of hypokalemia after a total hip and knee replacement procedure was performed.
Methods
This study included patients who underwent a unilateral total knee or hip arthroplasty in our department between April 2017 and March 2018. Serum potassium levels pre and post operation were collected and retrospectively analyzed. The differences in age, gender, body mass index (BMI), history of diseases, red blood cell (RBC), hemoglobin, hematocrit, glomerular filtration rate, ejection fraction, blood glucose, urine creatinine, urea nitrogen, intraoperative blood loss, operation time, drainage, preoperative potassium, surgery type, were compared between those patients diagnosed with hypokalemia and their non-hypokalemia at different times post surgery. Thereafter, the risk factors of postoperative hypokalemia patients were analyzed using statistical procedure multiple logistic regression model.
Results
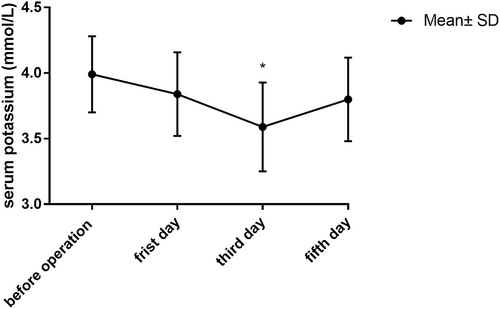
The risk of hypokalemia after TJA was 53.1%, while, that on the first, third, and fifth day after operation was 12.5%, 40.7%, and 9.6% respectively. The serum potassium level on the first, third, and fifth postoperative days was 3.84 ± 0.32, 3.59 ± 0.34, and 3.80 ± 0.32 mmol/l, respectively. However, the level on the third day appeared to be the lowest (p = 0.015) of them all. The independent risk factors for hypokalemia after a total hip and knee replacement were the level of preoperative serum potassium concentration (p = 0.011), preoperative red blood cells counts (p = 0.027), and history of diabetes (p = 0.007).
Conclusion
Regular monitoring of serum potassium concentration should be performed post TJA. We need to pay more attention to the patient's preoperative potassium levels along with their red blood cell counts especially in patients diagnosed with type 2 diabetes mellitus.
Introduction
Total joint arthroplasty (TJA) is a mature surgical technique. In the United States, studies have confirmed that by the year 2030 there will be ~572,000–635,000 primary hip replacements and 1.26–3.48 million primary knee replacement procedures performed.[1-3] However, these procedures bring with them some inevitable health complications and risk factors including but not limited to postoperative anemia,[4] prosthesis related infections,[5] deep venous thrombosis (DVT),[6] joint dislocation,[7] electrolyte imbalances,[8-10] vascular and nerve damage, among others.[11] Serum potassium is one of the most crucial electrolytes. Patients with moderate hypokalemia often present with symptoms such as weakness, fatigue, and constipation. When serum potassium concentration is less than 2.0 mmol/L, paralysis will occur, which ultimately may impair respiratory function.[12] In patients diagnosed with myocardial ischemia, heart failure, or left ventricular hypertrophy, it has been suggested that even mild to moderate hypokalemia can increase the risk of developing arrhythmias.[12, 13] In addition, hypokalemia can also cause longer durations of hospital stay and slow down recovery and ultimately raise the medical expenditures.[14-16]
There are only a few studies that have reported levels of serum potassium following an orthopaedic surgical procedure. Research has shown that the prevalence of hypokalemia after orthopaedic surgery is 25.2%.[10] A study has shown one patient with postoperative moderate hypokalemia (serum potassium 2,8 mmol/l) undergoing cardiac arrest (ventricular fibrillation).[17] Previous studies have reported that some of the possible risk factors for the occurrence of hypokalemia after a joint replacement procedure may include the patient's levels of preoperative serum potassium, if they may or may not have been diagnosed with type 2 diabetes.[8-10] However, conclusions about which factors induce hypokalemia after a joint replacement procedure are still vague, and the attitudes towards the necessity of detection of concentration of serum potassium are different.[8-10]
Therefore, the aims of this study were as follows: (i) to analyze the incidences and tendencies of hypokalemia after TJA; (ii) to explore the risk factors for hypokalemia after TJA.
Methods
Patients
This study was approved by the Institutional Review Board of Nanjing Drum Tower Hospital (No. 2012029). Patients meeting the following inclusion criteria were included: (i) patients with bilateral TJA during the research period, only the first procedure was included exclusively; (ii) with intact radiographic and clinical data at pre and post operation. We excluded patients diagnosed with serum hypokalemia prior to surgery (normal laboratory potassium value is defined as (3.5–5.5 mmol/ Liter),[12] (Mild hypokalemia: 3 to 3.5 mmol/ Liter, Moderate hypokalemia: 2.5 to 3 mmol/ Liter, Severe hypokalemia: less than 2.5 mmol/Liter).[13] Patients who underwent primary TJA in our department were screened between April 1, 2017 and March 31, 2018. Eventually, 160 patients met the study's inclusion criteria and were therefore recruited for the study.
Parameters
Parameters such as demographic and clinical data for the participants were collected from their medical records. Furthermore, additional data including age, sex, body mass index (BMI), comorbidities, history of prior surgical procedures, use of any anticoagulant drugs, cardiac ejection fraction, intraoperative blood loss, amount of blood transfusions, operation time, and the amount of postoperative drainage were also obtained. Additionally, laboratory concentration such as blood type, preoperative blood glucose, creatinine, glomerular filtration rate, hemoglobin, hematocrit, and serum potassium (K+) before surgery and the first, third, and fifth day post surgical procedures were also included in the analysis of data for this study protocol. Patients were then divided into two groups: (1) patients with normal postoperative serum potassium and (2) patients with abnormal postoperative serum potassium concentration.
Statistical Analysis
All statistical analyses were carried out using Statistical Package for the Social Sciences, version 20.0 (SPSS Inc., Chicago, IL). The independent t-test was used to examine differences in continuous variables between groups. The chi-square or Fisher's precision test was used to compare differences in categorical variables. The multivariate logic model was utilized for identifying the risk factors of hypokalemia. All baseline differences between the two groups were entered into the logistic regression model. The alpha level for all analyses was set to p < 0.05.
Results
General Data
The demographic data of the 160 enrolled subjects is shown in Table 1. There were 37 men and 123 women with an average age of 66.02 ± 10.11 years old. Fifty-two patients had primary hip arthroplasty and 108 patients had primary knee arthroplasty. Preoperative potassium was 3.99 ± 0.29 mmol/L. The lowest level of serum potassium after TJA reported was 3.59 ± 0.34 mmol/L on the third day following surgery (Figure 1, Table 2). There was a significant difference in serum potassium on the third day and the first or fifth day after operation (p = 0.027). However, no statistical differences appeared to be found between the levels on the first day and the fifth day after operation. The incidence of postoperative hypokalemia was 12.5%, 40.7%, and 9.6% on the first, third, and fifth days, respectively. Most of the patients suffered mild hypokalemia postop. The result shows that less than 10% of the patients with moderate and severe hypokalemia (Table 3).
| Variables | No. of patients (N = 160) |
|---|---|
| Age (years) (mean ± SD) | 66.02 ± 10.11 |
| Gender (female) (%) | 123 (76.8%) |
| BMI (kg/m2) (mean ± SD) | 25.5 ± 4.16 |
| Hypertension (%) | 84 (52.5%) |
| Diabetes mellitus (%) | 26 (16.2%) |
| Heart disease (%) | 28 (17.5%) |
| Smoking history (%) | 7 (4.4%) |
| Surgery type (TKA) (%) | 108 (67.5%) |
| Preoperative potassium (mmol/L) | 3.99 ± 0.29 |
| RBC, 109/L | 4.37 ± 0.52 |
| Hb, g/L (mean ± SD) | 128.48 ± 19.83 |
| HCT (%) | 41.00 ± 26.22 |
| Blood glucose (mmol/L) | 5.86 ± 1.70 |
| Urine creatinine (μmol/L) | 56.08 ± 14.73 |
| Urea nitrogen (mmol/L) | 5.78 ± 1.32 |
| eGFR (ml/min/1.73 m2) | 113.54 ± 28.94 |
| EF (%) | 60.11 ± 2.94 |
| Intraoperative blood loss, ml | 234.78 ± 193.84 |
| Operation time, min (mean ± SD) | 60.11 ± 2.94 |
| Drainage (ml) | 237.66 ± 193.84 |
- Abbreviations: BMI, body mass index; EF, ejection fraction; eGFR, glomerular filtration rate; Hb, hemoglobin; HCT, hematocrit; RBC, red blood cell; SD, standard deviation; TKA, total knee arthroplasty.
| First day | Third day | Fifth day | Total | |
|---|---|---|---|---|
| Mean ± SD (mmol/L) | 3.84 ± 0.32 | 3.59 ± 0.34 | 3.80 ± 0.32 | 3.74 ± 0.35 |
| New hypokalemia (total) | 20 (160) | 57 (140) | 8 (83) | 85 (160) |
| Percentage | 12.5% | 40.7% | 9.6% | 53.1% |
- Abbreviation: SD, standard deviation.
| Degree of hypokalemia | Hypokalemia | Percentage of total (%) | Percentage of hypokalemia (%) |
|---|---|---|---|
| Mild | 78 | 48.75 | 91.76 |
| Moderate | 5 | 3.13 | 5.88 |
| Severe | 2 | 1.25 | 2.35 |
Logistic Regression
Univariate logistic regression analysis showed that five factors were associated with postoperative hypokalemia including age (p = 0.010), diabetes mellitus (p = 0.013), preoperative red blood cell count (p = 0.024), preoperative serum potassium level (p = 0.008), and preoperative cardiac ejection fraction (p = 0.033) (Table 4). Combined with multivariate logistic regression analysis, age and cardiac ejection fraction were not found to be independent risk factors for postoperative hypokalemia (p = 0.778 and 0.069, respectively). Preoperative serum potassium concentration was found to be an independent factor of hypokalemia after TJA (p = 0.011). Patients with lower preoperative serum potassium concentration were 5.9 times more likely to postoperatively develop hypokalemia than those with higher preoperative serum potassium. Diabetes was also considered to be an independent risk factor that affected postoperative hypokalemia (p = 0.007). Patients without diabetes were 25.5% less likely to develop postoperative hypokalemia than their counterparts, suggesting that diabetes was an effective independent risk factor. Preoperative erythrocytes were also the independent influencing factor of hypokalemia after TJA (p = 0.027, Table 5).
| Variable | No hypokalemia (n = 75) | Hypokalemia (n = 85) | p value | Statistic-value |
|---|---|---|---|---|
| Age, years (mean ± SD) | 68.2 ± 8.7 | 64.1 ± 11.0 | 0.010* | −3.229 |
| Female gender (%) | 59 (47.9) | 64 (52.1) | 0.614 | 0.157 |
| BMI, kg/m2 (mean ± SD) | 25.3 ± 4.0 | 25.7 ± 4.3 | 0.577 | −0.563 |
| Diabetes (%) | 36 (42.9) | 48 (57.1) | 0.013* | 5.720 |
| Hypertension (%) | 108 (46.2) | 14 (36.8) | 0.284 | 1.171 |
| Heart disease (%) | 16 (57.1) | 12 (42.9) | 0.231 | 1.209 |
| Smoking history (%) | 2 (28.6) | 5 (21.4) | 0.321 | 0.842 |
| History of thrombosis | 10 (13.3) | 13 (15.3) | 0.724 | 0.147 |
| History of anticoagulant | 10 (13.3) | 7 (8.2) | 0.296 | 1.102 |
| History of other medication | 20 (26.6) | 14 (16.5) | 0.116 | 2.583 |
| Surgical history | 19 (25.3) | 13 (15.3) | 0.113 | 2.591 |
| Surgery type (TKA) (%) | 53 (49.1) | 55 (50.1) | 0.422 | 0.731 |
| Preoperative potassium (mmol/L) | 4.1 ± 0.24 | 3.9 ± 0.27 | 0.008* | −3.890 |
| RBC, 109/L | 4.3 ± 0.46 | 4.4 ± 0.56 | 0.024* | −2.011 |
| Hb, g/L (mean ± SD) | 129.48 ± 12.83 | 127.60 ± 24.44 | 0.551 | −0.583 |
| HCT (%) | 38.7 ± 4.4 | 43.1 ± 3.6 | 0.290 | −1.101 |
| Blood glucose (mmol/L) | 5.48 ± 1.13 | 5.18 ± 1.29 | 0.122 | −1.471 |
| Urine creatinine (μmol/L) | 56.98 ± 15.52 | 55.29 ± 13.67 | 0.467 | −0.781 |
| Urea nitrogen (mmol/L) | 6.08 ± 1.56 | 5,68 ± 1.76 | 0.134 | −1.290 |
| eGFR (ml/min/1.73 m2) | 110.34 ± 26.24 | 116.36 ± 30.35 | 0.184 | −1.172 |
| EF (%) | 59.6 ± 2.7 | 60.6 ± 3.0 | 0.033* | −1.771 |
| Operation time, min (mean ± SD) | 99.1 ± 26.1 | 103.6 ± 21.8 | 0.245 | −1.120 |
| Drainage (%) | 60 (80) | 66 (77.6) | 0.717 | −0.173 |
| Blood transfusion | 7 (9.3) | 7 (8.2) | 0.816 | 0.104 |
- Abbreviations: BMI, body mass index; EF, ejection fraction; eGFR, glomerular filtration rate; Hb, hemoglobin; HCT, hematocrit; RBC, red blood cell; SD, standard deviation; TKA, total knee arthroplasty
- * p < 0.05 was considered statistically significant.
| Variables | p-value | OR | 95% CI |
|---|---|---|---|
| Potassium | 0.011* | 5.997 | 1.502–23.934 |
| Diabetes | 0.007* | 0.255 | 0.095–0.688 |
| RBC | 0.027* | 0.417 | 0.193–0.903 |
| Constant | 0.412 | 107.674 | - |
- Abbreviations: 95% CI, confidence interval; OR, odds ratio; RBC, red blood cell
- * p < 0.05 was considered statistically significant.
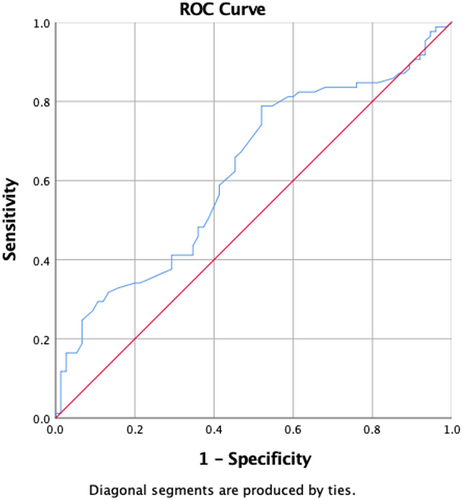
Receiver Operating Characteristics
In the receiver operating characteristics (ROC) analysis for the risks of postoperative hypokalemia, the area under the curve (AUC) was 0.62 ((95% CI 0.7–0.9), p = 0.008) and when the cut-off value of preoperative potassium was set at 4.0 mmol/L, the sensitivity and specificity of postoperative hypokalemia were 78.8% and 48.0%, respectively (Figure 2, Table 6).
| Preoperative potassium | ||||
|---|---|---|---|---|
| Area | Std. Errora | Asymptotic Sig.b | Asymptotic 95% confidence interval | |
| Lower bound | Upper bound | |||
| 0.621 | 0.044 | 0.008* | 0.534 | 0.708 |
- a Under the nonparametric assumption
- b Null hypothesis: true area = 0.5
- * p < 0.05 was considered statistically significant.
Discussion
Summary of Results
In this retrospective study, 85 of 160 enrolled patients developed postoperative hypokalemia within 5 days of surgery and the rate of postoperative hypokalemia on the third day appeared to be the highest. Multivariate analysis showed that preoperative potassium, red blood cell count, and type 2 diabetes were independent risk factors for developing hypokalemia. In the ROC (receiver operating characteristic curve) analysis, the cut-off value of preoperative potassium was set at 4.0 mmol/L, and the sensitivity and specificity of preoperative potassium value in predicting postoperative hypokalemia were 78.8% and 48.0%, respectively.
Checking Point after TJA
The previous study has thought postoperative basic metabolic panel should not be routinely tested in patients unless they have medical comorbidities, and their potassium is below 4 mmol/L.[9] Halawi et al. provided evidence that routine postoperative laboratory testing is not necessary for modern-day primary unilateral THA. The decisions to analyze serum potassium levels post joint replacement procedures are still in their infancy. In the present study, 53.1% of patients developed serum hypokalemia within 5 days postoperative with slight, moderate, and severe hypokalemia accounting for 48.75%, 3.13%, and 1.25%, respectively. And the level of serum potassium decreased from pre-operational until the third-day post surgery and then reflected a slight increase. Thus, we proposed that serum potassium should be checked on the third day after TJA in order to prevent the development of severe hypokalemia (serum potassium, <2.5 mmol per liter).
Reasons for Hypokalemia after TJA
It is believed that the occurrence of postoperative hypokalemia is related to a variety of factors, including an acute shift of potassium from the extracellular compartment to cells, inadequate intake and abnormal losses of potassium.[18] By multivariate regression analysis, we found that the independent risk factors for hypokalemia after TJA were diabetes and preoperative serum potassium level, which was similar to the report of Mohamad et al.[10] Kildow[10] also regarded diabetes as an important predictor for the feedback system regulating potassium and insulin levels. The increase of extracellular potassium concentration stimulates the release of insulin and causes cells to absorb potassium.[12, 19] Normally, higher extracellular potassium levels can potentially increase the release of endogenous insulin by inhibiting ATP-sensitive potassium channels within the pancreatic B-cells.[20] In diabetics, it has been observed that low insulin levels could lead to the elimination of glucose from the kidneys which can in turn increase the delivery of sodium to the distal nephron and increase potassium excretion.[21] Diabetes often requires the use of pharmacological interventions such as oral hypoglycemic drug use or subcutaneous insulin injections in comparison to patients without a diagnosis of type 2 diabetes. It appears that diabetics tend to have larger fluctuations of serum potassium concentration which could lead to abnormal potassium ion distribution, which is likely the cause of postoperative low potassium.[18] In the present study, patients with diabetes mellitus showed a significant increase in postoperative hypokalemia, thus confirming previous findings.
Our study also first found that preoperative red blood cell count is also a risk factor impacting postoperative hypokalemia, which may be related to intraoperative and postoperative loss of red blood cells and fluids. Thus, we recommend additional prospective studies to rule out such clinical variations.
Hypokalemia Treatment
In addition, two patients in this study developed severe hypokalemia after surgery. The main symptoms of the two patients were severe discomfort of the precordial region, muscular weakness, and constipation. Potassium solution, diluted with saline water with concentration 0.3% was pumped into the patient's body by intravenous micropump, and the speed of potassium supplement was adjusted (potassium supplement speed 150 ml/h or less), according to central venous pressure of the patients during the period, when the serum potassium concentration rises to 3 mmol/liter instead of oral potassium supplement. If we did not carry out serum potassium monitoring, serious complications could have occurred and the previous study had already reported that early potassium monitoring could offer a helpful tool to correct hypokalemia postoperative.[22] We believe that two patients with diabetes, lower preoperative serum potassium concentration, and lower preoperative red blood cell counts were the causes of postoperative hypokalemia, which is consistent with the results of this study.
Limitations
This study, however, has several limitations. First, this is a single-center study with a relatively small sample size. Second, this was a retrospective study, there are still other confounders not introduced into the analysis due to the retrospective nature of this study. Hence, prospective studies with a multicenter and a large sample are urgently required.
Conclusions
Routine monitoring of serum potassium should be performed on account of patients presenting with the highest risk of hypokalemia on the third day post joint replacement procedures. We need to pay more attention to patients’ preoperative potassium levels and red blood cell counts, especially in those patients diagnosed with type 2 diabetes.
Acknowledgment
This work was supported by the National Science Foundation of China (81871832), Key Program of NSFC (81730067), Major Project of NSFC (81991514), by Jiangsu Provincial Key Medical Center Foundation, Jiangsu Provincial Medical Outstanding Talent Foundation, Jiangsu Provincial Medical Youth Talent Foundation and Jiangsu Provincial Key Medical Talent Foundation, the Fundamental Research Funds for the Central Universities (14380493, 14380494).
Conflict of Interest Statement
The authors have no conflict of interest to declare. This study was approved by the University Institutional Review Board.
Ethics Statement
We give permission to reproduce copyrighted materials or signed patient consent forms. The manuscript submitted does not contain information about medical device(s)/drug(s). No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author Contribution
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and all authors are in agreement with the manuscript.