A Femoral Neck Osteotomy for the Patients with Ankylosing Spondylitis and Thoracolumbar Kyphosis Combined with Hip Flexion Contracture
Xin Yang and Qiwei Wang contributed equally to this study and share first authorship.
Abstract
Objective
The surgical treatment of patients with ankylosing spondylitis and severe thoracolumbar kyphosis combined with hip flexion contracture is very difficult for all the surgeons. The femoral neck osteotomy (FNO) is the first step to break the ice. The evaluation of a new modified FNO method is very important to improve the curative effect.
Methods
Five male patients with nine bone-fused hips who underwent the new femoral neck osteotomy were included from October 2021 to March 2022. The FNO was designed that the saw blade was manipulated from the lateral femoral neck base to the inferior part of the femoral head, keeping Pauwels' angle less than 30° on the coronal plane. On the transverse plane, the angle between the saw blade and the coronal plane was more than 15°. On the sagittal plane, the saw blade cut through the femoral neck. They accepted pedicle subtraction osteotomy (PSO) after FNO according to the patient’ recovery. Then, 2 weeks later, the patients underwent total hip arthroplasty (THA). The visual analogue scale (VAS), Harris hip score (HHS) and passive hip flexion-extension range of motion (ROM) were used to evaluate hip function. The data were analyzed by paired t-test.
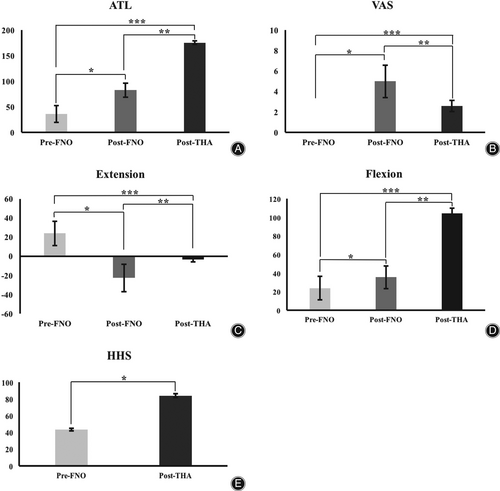
Results
The average operation time and blood loss of FNO, the average interval between FNO and THA were collected. The average angle of the trunk and lower limb (ATL) was 36.33° ± 16.36° pre-FNO, 82.89° ± 13.51° post-FNO and 175.22° ± 3.42° post-THA. The average VAS scores were 0 pre-FNO, 5 ± 1.58 post-FNO and 2.6 ± 0.55 post-THA. The average HHS was 43.56 ± 1.59 preoperatively and 83.89 ± 2.21 postoperatively. The average hip extension ROM was 23.89° ± 12.69° pre-FNO, −22.67° ± 14.18° post-FNO and − 3.33° ± 2.50 post-THA°. The average hip flexion ROM was 23.89° ± 12.69° pre-FNO, 35.56° ± 12.11° post-FNO and 104.44° ± 5.27° post-THA. The differences among them were significant (p < 0.05). Only one hip (11.11%) displaced completely after FNO.
Conclusion
A new modified FNO was developed, which can provide osteotomy with a certain degree of stability and greater ease for performing PSO and THA.
Introduction
Surgeons often experience difficulty operating on patients with ankylosing spondylitis who have thoracolumbar kyphosis combined with hip fusion. Pedicle subtraction osteotomy (PSO) is usually performed to correct the thoracolumbar kyphosis, and total hip arthroplasty (THA) is used to improve the function of the hip.1, 2 The research shows that spinal alignment correction before THA could reduce the spinopelvic alignment-related THA complications.3 So it is suggested that PSO is finished before THA. The PSO in the prone position is suggested to be the best choice for achieving an optimal therapeutic effect.1 But patients with severe thoracolumbar kyphosis combined with hip flexion contracture commonly referred to as having “the folding man” position, could not keep the prone position. There is no article to report the standard treatment procedure for those patients.
Femoral neck osteotomy (FNO) could be used to avoid femoral nerve and vessel injury when performing two-stage THA for patients with severe hip contracture.4 But removal of a segment of femoral neck is needed to preform the femoral supracondylar bone traction.4 The FNO technique is reported to correct the deformity of proximal femur, such as coxa valga and varus femoral neck.5 Femoral neck rotational osteotomy is reported to be a modified method for treating necrotic femoral heads.6 The femoral neck lengthening osteotomy is suggested to preserve hips with Perthes and Perthes-like deformities.7 But they all use internal fixation to keep the osteotomy stable. So, to preserve the bone volume of hip and reduce the internal fixation, we designed a new stable FNO to improve the hip flexion contracture and help the patient maintain the prone surgery position. We named it modified Pauwels' FNO because we obtained the idea from the concept of Pauwels' classification of femoral neck fractures. We designed our FNO to resolve the typical complications of unstable femoral neck osteotomy, including severe postoperative hip pain, complete displacement and limb shortening, end wear of the osteotomy and hip bone loss.
Our research objectives are as follows: (i) to provide a new modified FNO method to treat these patients with severe deformity; (ii) to evaluate the safety and effect of the new FNO; and (iii) to evaluate the therapeutic effect of these patients after THA.
Methods
Patient Introduction
We had five male patients with nine bone-fused hips who agreed to undergo the new modified FNO from October 2021 to March 2022. The inclusion criteria were: (i) the patients had ankylosing spondylitis; (ii) the patients had severe thoracolumbar kyphosis combined with hip flexion contracture and could not keep in the prone position; and (iii) the patients needed the PSO and THA operations. The exclusion criteria were: (i) the patients needed only PSO or THA; (ii) the patients could keep in the prone position; and (iii) the patients could not tolerate surgery. All patients had ankylosing spondylitis and severe thoracolumbar kyphosis combined with hip flexion contracture (Figure 1). The patients had an average age of 45 years, ranging from 32 to 54 years. Four patients underwent one-stage bilateral FNO, and the other patient only underwent left hip surgery. The surgical plans were made preoperatively by spine and joint surgeons together for all the patients. They underwent PSO in the prone position after FNO. Then, 2 weeks later, the patients underwent THA. Bilateral THA was performed in two stages due to the body condition of the patients. The FNO and THA were performed by the same surgical team. This study was approved by the Ethics Committee of Peking University First Hospital (No. 2022-414-002).
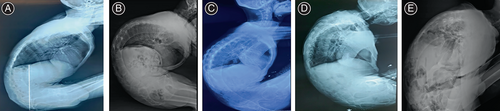
Considering thoracolumbar kyphosis and pelvic tilt, the degree of hip flexion contracture is very difficult to evaluate with physical examination in patients with ankylosing spondylitis who have severe thoracolumbar kyphosis combined with hip flexion contracture. There are no articles which report the classification of the severity of thoracolumbar kyphosis combined with hip flexion contracture. Therefore, we defined the angle of the trunk and lower limb (ATL) as the angle between the axillary midline and the lateral body surface projection of the femoral bone in the supine position (Figure 2). In this way, it can be evaluated from physical examinations and suggest the severity of thoracolumbar and hip deformity. When the ATL was less than 60°, we defined the patient as having the severe type of thoracolumbar kyphosis combined with hip flexion contracture and referred to the patient as having “the folding man” position. These patients needed FNO, PSO and THA. When the ATL was between 60° and 120°, we defined the patient as the “moderate type.” These patients needed only PSO and THA. The “light type was referred to the condition in patients with an ATL greater than 120°, who might just need THA. Some patients had the same ATLs on both sides, while in others they were different. We performed the operation on the side that had a smaller ATL.
Design of the New Modified Femoral Neck Osteotomy
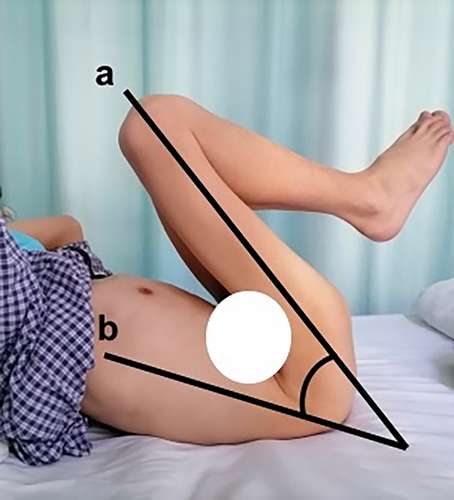
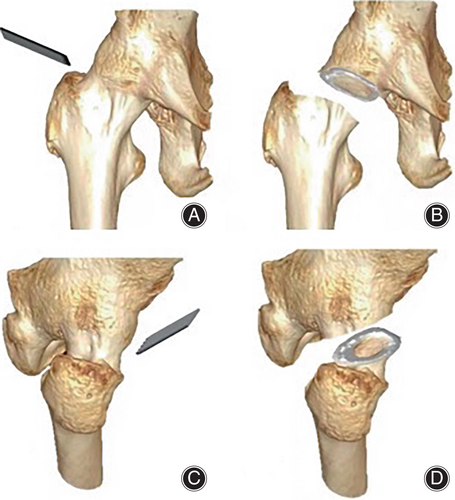
Standard FNO without internal fixation is similar to a femoral neck fracture. If the fracture is unstable, problems such as continuous severe hip pain, completed displacement, limb shortening and deformity will be barriers to performing THA. Therefore, we attempted internal fixation with three 7.3-mm hollow screws after transverse FNO in one patient. Because of hip osteoporosis and body postural changes in the patient, the internal fixation loosened. Furthermore, the postoperative hip pain was severe, and increased the difficulty in providing postoperative care. The screws were shown to cause bony defects in the acetabulum and femoral neck on CT scan and resulted in many difficulties in performing the THA. Therefore, we attempted to improve the FNO method to avoid these problems. Pauwels' classification is used to classify the stability of femoral neck fractures and is continuously improved.8 The angle between the fracture and horizontal lines is known as Pauwels' angle; if the angle is less than 30°, the fracture is considered a stable type I fracture, in which the problems of hip pain, complete displacement, limb shortening and deformity are not prominent.9 Therefore, we designed the coronal plane of the FNO to be in accordance with a Pauwels' angle less than 30°. The saw blade was manipulated from the lateral femoral neck base to the inferior part of the femoral head, as the a' osteotomy line in Figure 3A.
All patients had bone-fused hips and received posterolateral approach. FNO must be designed to allow the surgeon to conveniently perform THA; anteversion of the acetabulum is an important factor in this design. Therefore, on the transverse plane, the saw blade was manipulated from the back part of the femoral neck base to the front part of the proximal femoral neck to protect the acetabulum. The saw blade was required to keep an angle less than 15 degree with the coronal plane, consistent with acetabular anteversion, as the b' osteotomy line in Figure 3B. On the sagittal plane, the saw blade cut through the anterior-inferior and posterior-superior cortical bone of the femoral neck to avoid splitting the proximal femoral shaft and acetabulum. After our FNO, the ends were the anterior-inferior and posterior-superior cortical bone of the femoral neck (Figures 4 and 5).
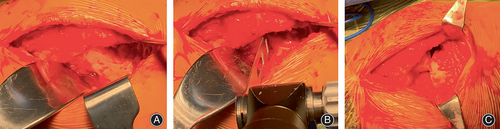
Postoperative Therapy
After the new modified FNO, all the patients received patient control vein analgesia and oral analgesics (one tablet of oxycodone-acetaminophen three times and one tablet of tramadol hydrochloride twice per day) to relieve the postoperative hip pain as routine. Continuous limb skin traction with two-kilogram weight was performed to improve the ATL until ATL was larger than 60°. PSO was then performed after FNO according to the patient recovery. The interval time was about 1 to 2 weeks. And ~2 weeks later, THA followed (Figure 6).Our criteria for the next operation were: the hemoglobin was over 80 g/L and the albumin was over 28 g/L in blood test. THA was performed by the previous posterolateral incision of FNO.
Measurement Method
The operation time of and blood loss during FNO and the interval between the FNO and the first THA were collected. A visual analogue scale (VAS) was used to evaluate the hip pain. The ATL was used to describe the deformity and effect of surgery. The Harris hip score (HHS) and passive hip flexion-extension range of motion (ROM) were used to evaluate hip function. The VAS, ATL and ROM were evaluated before FNO, 10 days after FNO and before PSO, and 14 days after THA. The HHS was evaluated before FNO and 14 days after THA.
Statistical Analysis
All data are presented as the mean ± SD. The data were analyzed by paired t-test using SPSS 20.0 (SPSS Inc., Chicago, IL, USA) statistical software. Statistical significance was set at p < 0.05.
Results
The Operation time and Blood Loss
For single-sided FNO, the operation time was 60 min, and blood loss was 200 ml. For bilateral FNO, the average operation time 153.75 ± 37.79 min (including the time of posture change and skin disinfection), and blood loss was 450.00 ± 57.74 ml (Table 1). The average interval between FNO and the first and second THA were 37.20 ± 15.42 and 48.75 ± 18.89 days, respectively (Table 2).
| Patient number | Gender | Age (yrs) | Femoral neck osteotomy | ||
|---|---|---|---|---|---|
| Operation side | Operation time (min) | Blood loss (ml) | |||
| 1 | M | 32 | B | 150 | 400 |
| 2 | M | 56 | B | 143 | 500 |
| 3 | M | 54 | B | 116 | 400 |
| 4 | M | 37 | L | 60 | 200 |
| 5 | M | 46 | B | 206 | 500 |
- Abbreviations: B, bilateral; FNO, femoral neck osteotomy; L, left; M, male; min, minutes; ml, milliliters; yrs, years.
| Patient number | Total hip arthroplasty | |||
|---|---|---|---|---|
| Operation side | Operation time (min) | Blood loss (ml) | Interval from FNO (days) | |
| 1 | L | 120 | 300 | 40 |
| R | 156 | 900 | 50 | |
| 2 | R | 185 | 3000 | 49 |
| L | 178 | 1000 | 70 | |
| 3 | R | 176 | 1500 | 38 |
| L | 178 | 2500 | 51 | |
| 4 | L | 120 | 800 | 48 |
| 5 | R | 173 | 1300 | 11 |
| L | 170 | 800 | 24 | |
- Abbreviations: L, left; min, minutes; ml, milliliters; R, right; THA; total hip arthroplasty.
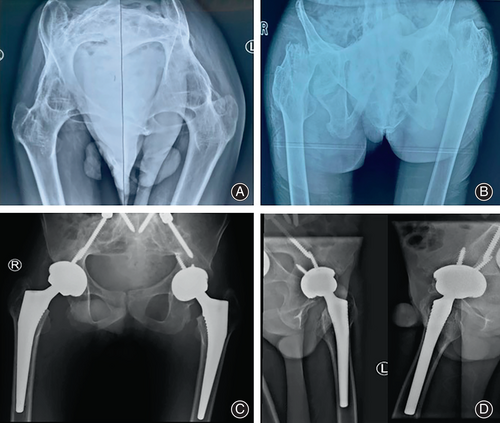
The Clinical Effect Evaluation
Only one hip (11.11%) displaced completely (Figure 7); the other eight hips displaced partially after FNO (Table 2). The ATLs were 13°–65° (average 36.33° ± 16.36°) pre-FNO, 60°–105° (average 82.89° ± 13.51°) post-FNO and 170°–180° (average 175.22° ± 3.42°) post-THA, and the differences among them were significant (p < 0.05) (Table 3 and Figure 8). The VAS scores were 0 (average 0) pre-FNO, 3–7 (average 5 ± 1.58) post-FNO and 2–3 (average 2.6 ± 0.55) post-THA, and the differences between them were significant (p < 0.05) (Table 3 and Figure 8). The hip extension ROMs were 5°–40° (average 23.89° ± 12.69°) pre-FNO, −35°–0° (average −22.67° ± 14.18°) post-FNO and −5°–0° (average −3.33° ± 2.50°) post-THA (Table 3). The hip flexion ROMs were 5°–40° (average 23.89° ± 12.69°) pre-FNO, 15°–50° (average 35.56° ± 12.11°) post-FNO and 95°–110° (average 104.44° ± 5.27°) post-THA, and the differences between them were significant (p < 0.05) (Table 3 and Figure 8).The HHS scores were 42–46 (average 43.56 ± 1.59) preoperatively and 80–87 (average 83.89 ± 2.21) postoperatively, and the difference was significant (p < 0.05) (Table 3 and Figure 8).

| Patient number | Operation side | ATL (°) | VAS | HHS | ROM(°) | Complete displacement after FNO (Y/N) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Extension | Flexion | |||||||||||||||
| Pre-FNO | Post-FNO | Post-THA | Pre-FNO | Post-FNO | Post-THA | Pre-FNO | Post-THA | Pre-FNO | Post-FNO | Post-THA | Pre-FNO | Post-FNO | Post-THA | |||
| 1 | L | 38 | 90 | 175 | 0 | 3 | 3 | 44 | 85 | 30 | −22 | −5 | 30 | 40 | 100 | N |
| R | 40 | 86 | 178 | 44 | 87 | 35 | −11 | 0 | 35 | 40 | 105 | N | ||||
| 2 | L | 43 | 85 | 170 | 0 | 4 | 2 | 42 | 80 | 10 | −32 | −5 | 10 | 20 | 95 | N |
| R | 35 | 80 | 176 | 42 | 84 | 5 | −40 | −5 | 5 | 15 | 100 | Y | ||||
| 3 | L | 50 | 90 | 178 | 0 | 6 | 3 | 45 | 82 | 40 | 0 | 0 | 40 | 50 | 110 | N |
| R | 65 | 105 | 180 | 45 | 85 | 35 | −5 | −5 | 35 | 50 | 110 | N | ||||
| 4 | L | 28 | 85 | 175 | 0 | 5 | 2 | 46 | 86 | 30 | −27 | 0 | 30 | 40 | 110 | N |
| 5 | L | 13 | 60 | 170 | 0 | 7 | 3 | 42 | 82 | 15 | −32 | −5 | 15 | 30 | 105 | N |
| R | 15 | 65 | 175 | 42 | 84 | 15 | −35 | −5 | 15 | 35 | 105 | N | ||||
- Abbreviations: ATL, the angle of the trunk and lower limb; FNO, femoral neck osteotomy; HHS, the Harris hip score; L, left; N, no; R, right; ROM, the range of motion; THA, total hip arthroplasty; VAS, the visual analogue scale; Y, yes.
There was only one hip which got complete displacement after our FNO, because of the therapy for pleural effusion and pneumonia after PSO surgery in the respiratory intensive care unit (RICU). There were no complications such as vessel and nerve injury, bone fracture and prosthetic dislocation during the entire treatment process.
Discussion
To ensure the safety of the patients and obtain the good effect of treatment, we modified the FNO to be a stable osteotomy to avoid the complications for the patients with ankylosing spondylitis and severe thoracolumbar kyphosis combined with hip flexion contracture. Our modified FNO proved to provide ease for performing PSO and THA. The efficacy and safety of our modified FNO also been evaluated.
The Importance of the Standard PSO
For the patients with ankylosing spondylitis and severe thoracolumbar kyphosis, the standard PSO is recommended to be performed in the prone position with the patient placed on a table that allows extension, which can aid in the corrective effect of the osteotomy. After pedicle and vertebral body resection, the surgeon needs to adjust the bed to correct and close the osteotomy. The flexing and extending functions of the operating room tables are conducted by remote control, where they are often labeled “reflex.” The surgeon can use this function to elevate the trunk and legs of the patient at the same time and push the spine down manually. This maneuver not only closes the osteotomy but also allows greater correction of the sagittal plane deformity through the osteotomy.1 Some surgeons have performed PSO in the lateral position to avoid the difficulties associated with the patient's body position.10 This article reported only two such cases. The surgeon needed two off-table staff to push the shoulders and pelvis of the patient to extend the lumbar slowly and simultaneously. This manipulation might not take the X-ray or CT scan between the lumbar extension and the internal fixation. The effect of kyphosis correction requires more cases to be evaluated and compared with prone position surgery.
The Benefit of our FNO for General Situation
Patients whose ATL was less than 60°, that is, those with the severe type of the condition, usually had cardiopulmonary and gastrointestinal dysfunction. Patients who had ankylosing spondylitis have been reported to have more comorbidities than normal patients, such as congestive heart failure, peripheral vascular disease and chronic obstructive pulmonary disease, and increased complications following THA.3 Therefore, increasing the ATL can improve the function of those organs and enhance the tolerance of patients to different follow-up surgeries. The new FNO is very beneficial for these patients, especially for those with “the folding man” position. After this surgery, we treated the cardiopulmonary and gastrointestinal dysfunctions to avoid complications of the cardiopulmonary and gastrointestinal systems after PSO and THA.
FNO is usually used to correct hip deformities.5 Zeng reported performing femoral osteotomy for stage I and THA 2 weeks later for stage II to treat patients with ankylosing spondylitis with severe hip contracture. Among his procedures, he removed a segment of the femoral neck and corrected the joint contracture. The results revealed that the two-stage treatment group had better function and fewer complications than the control group, who had undergone traditional THA alone.4 But the longer the two stage THA interval was, the greater the incidence of complications such as postoperative hip pain, complete displacement and limb shortening, end wear of osteotomy and hip bone loss. Our patients needed not only the two-stage THA, but also the PSO before the THA. So the interval time between FNO and THA was much longer than that of two-stage THA as the article reported. So to decrease the incidence of complications, we modified the FNO. There was no need to remove a segment of the femoral neck after osteotomy; our FNO required the preservation of all the cortical bone of the femoral neck to maintain stability and protect the acetabulum.
From our results regarding the operation time and blood loss, our FNO was shown to be a simple surgery. We regularly performed bilateral FNO as needed, and PSO could follow several days or a week later. As stated above, our FNO allows the surgeon to more easily perform PSO and THA and is also advantageous for delivering general anesthesia. One of our patients, whose left and right ATLs were 13° and 15° separately, had difficulty tolerating general anesthesia, and so endotracheal intubation was performed between the two legs. After FNO, the ATL was improved significantly, general anesthesia for PSO and THA became easier, and the overall safety of the surgical procedures increased.
The Benefit of our FNO for THA
Bone-fused hips pose difficulties for THA. From body position and skin disinfection to incision design and operation manipulation, all the steps can have different problems because different patients will present with different fused hip positions.11 Some patients have fused hips with flexion contracture, abduction and external rotation simultaneously and thus can only maintain the supine position and not the lateral or prone position for PSO and THA. In these cases, the THA operation may require an anterior hip approach.12 Some patients have a fused position with hip flexion contracture, adduction and internal rotation simultaneously, causing both knees to touch each other and thus require knee skin disinfection for THA. Some patients even require an anterior incision for neck osteotomy in the supine position followed by THA via a posterior approach.11 Idulhaq et al.13 reported a patient who had a fused hip with a 90° flexion deformity who underwent partial osteotomy of the neck anteriorly from the intermuscular interval exposure between the gluteus medius and tensor fascia lata, and then the remaining neck was osteotomized from the posterior aspect through the posterolateral approach. In the THA operation, there are many problems to be resolved. The fused hip cannot be dislocated before femoral neck dissection. It is hard to identify the margins of the femoral head and acetabulum.14 The bone stock is poor, so acetabular cup protrusion and femoral shaft fracture can easily occur.15 The soft tissue is tight in all directions, so the femoral vessel and nerve injury during surgery are not rare for patients with hip flexion contracture.16 Our patients who had severe thoracolumbar kyphosis and hip flexion contracture had much more difficulties than those who had only bone-fused hips. Due to less activity volume, they had worse bone quality. During the THA, we not only took care of the hip, but also avoid the spine fracture and loosen of pedicle screws. Because of the thoracolumbar kyphosis, the contracture of soft tissue was much more severe, so the range of soft tissue release in THA required much larger. We should take care of the femoral vessels and nerves, as well as the sciatic nerve. After our FNO, the hips were granted a certain degree of activity, and those problems were greatly alleviated.
The Efficacy and Safety of our FNO
Postoperative hip pain, complete displacement and limb shortening, end wear of the osteotomy, and hip bone stock maintenance may be the main problems after FNO. Our modified FNO addresses these problems, as it is designed to maintain the stability of the two ends of the osteotomy. The results revealed that the postoperative hip pain was well controlled following administration of analgesics. The patients could sit on the bed, and the ATL was improved and the soft tissue in the front of the thigh was stretched through skin traction. The complete displacement rate was very low; only one right hip displaced completely, which occurred following admission to the RICU for pleural effusion and pneumonia after PSO surgery. In the RICU, this patient had to lie on his side and required repeated turning over for pulmonary care. Therefore, the right hip of this patient displaced completely but his left hip had partial displacement until THA. After PSO, we performed skin traction on the leg on which THA was planned. The soft tissue was stretched to maintain the limb length and decrease the risk of arteria femoralis and nervus femoralis injury. After our FNO, the ends were the anterior–inferior and posterior–superior cortical bone of the femoral neck. The finding in THA revealed little end wear of the osteotomy and good maintenance of hip bone stock. We did not use internal fixation after FNO because this did not produce beneficial effects for one patient treated prior to this study in controlling the postoperative hip pain and maintaining the hip bone stock due to loosening of the internal fixation. It is difficult to maintain the stability of the osteotomy with internal fixation because of osteoporosis and low limb movement.
THA was performed on those patients like old femoral neck fractures. The results revealed that THA on the hip that had completely displacement of osteotomy was of longer duration and resulted in much more blood loss than THA on the other hips. Therefore, we think our new modified FNO method, which can maintain a stable osteotomy, is beneficial for those patients and surgeons.
Surgical Tips
The narrow saw blade was suggested to do the FNO. Before the osteotomy, the planned osteotomy line should be marked on the femoral neck bone by electrotome. After the osteotomy, osteotome could be used to make sure the femoral neck was truncated totally.
Limitations and Strengths
One limitation of our proposed procedure is the need for an additional operation before PSO and THA, similar to two-stage THA. Therefore, the patients need more time to be admitted to the hospital. However, FNO, even bilateral, does not have a high operation time or blood loss. Additionally, these patients were young or middle aged and thus had a rapid recovery from the osteotomy. Compared to the difficulties caused by severe thoracolumbar kyphosis and hip flexion contracture, we consider FNO to be much easier. Therefore, this method should be very useful in the treatment of these patients.
In our study, we concentrated to treat these cases within half a year. We gained considerable experience and the total effect was evaluated in a short period. The result proved the effect of our FNO. So we should promote the method to help more patients.
Conclusions
We proposed a new modified FNO to improve the treatment of patients with ankylosing spondylitis who have severe thoracolumbar kyphosis combined with hip flexion contracture. This FNO can improve the ATL and provide osteotomy of a certain level of stability. The effect of FNO can provide greater ease for performing PSO and THA, and avoid the injury of blood vessels and nerves.
Author Contributions
Xin Yang and Qiwei Wang finished conceptualization, data curation, investigation, and writing the original draft. Yu Wang and Yongping Cao finished conceptualization, project administration, resources and supervision. Zhichao Meng, Heng Liu, Hao Wu, Talante Juma and Liping Pan helped to finish data curation, formal analysis, investigation and reviewing and editing the article. All authors reviewed the article.
Funding Information
This work was supported by Capital's Funds for Health Improvement and Research (CFH 2020-2-4076).
Conflict of Interest Statement
The authors declare no conflicts of interest.
Declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and all authors are in agreement with the manuscript.
Ethics Statement
This study was approved by the Ethics Committee of Peking University First hospital. The number is No. 2022–414-002. All methods were carried out in accordance with relevant guidelines and regulations. All informed consent were obtained from all subjects and/or their legal guardian(s).