Percutaneous Endoscopic Lumbar Discectomy via Transforaminal Approach Combined with Interlaminar Approach for L4/5 and L5/S1 Two-Level Disc Herniation
Disclosure: There were no any potential conflicts of interest among all authors.
Abstract
Objective
The purpose of the present study was to discuss a new surgical strategy that combines percutaneous endoscopic transforaminal discectomy (PETD) with percutaneous endoscopic interlaminar discectomy (PEID) for L4/5 and L5/S1 two-level disc herniation.
Methods
This was a retrospective study. A total of 19 patients with L4/5 and L5/S1 two-level lumbar disc herniation (LDH) who underwent percutaneous endoscopic lumbar discectomy (PELD) in our hospital from January 2015 to June 2016 were retrospectively examined. The average age of these 19 patients was 42.21 ± 14.88 years old, including 12 men and 7 women. One experienced surgeon who had carried out more than 3000 lumbar surgeries performed PELD for these patients. During the PELD surgery, the transforaminal approach was adopted for L4/5 level disc herniation and the interlaminar approach was adopted for L5/S1 level disc herniation. The demographic data, operation time (min), fluoroscopy times, hospital stay (days), and complications were recorded and analyzed. The visual analogue scale (VAS), Oswestry disability index (ODI) scores, and the modified MacNab criteria were used to evaluate the surgical outcomes. MRI was conducted to evaluate the radiographic improvement.
Results
All patients underwent PELD via the transforaminal approach combined with the interlaminar approach successfully and achieved satisfactory efficacy. The follow-up points were 3, 12, and 18 months. The average hospital stay (days) and the average follow up (months) were 3.32 ± 0.98 and 18.63 ± 3.84, respectively. The operation time and fluoroscopy times were 85.79 ± 12.90 min and 39.05 ± 4.59 times, respectively. The fluoroscopy times (frequency) for L4/5 and L5/S1 were 26.95 ± 6.41 and 12.11 ± 3.49 (t = 7.00, P < 0.05). Furthermore, there was no significant difference for fluoroscopy times between male and female patients (t = 0.89, P = 0.99). The preoperative back pain (VAS-Back) and the last follow-up VAS-Back were 5.58 ± 2.01 and 2.37 ± 1.01, respectively (t = 7.14, P < 0.05). The preoperative leg pain (VAS-Leg) and the last follow-up VAS-Leg were 7.00 ± 1.56 and 1.63 ± 1.01, respectively (t = 20.97, P < 0.05). There were significant differences between preoperative VAS-Back and the last follow-up VAS-Back in men (t = 4.61, P < 0.05) and women (t = 6.57, P < 0.05). In addition, there was significant differences between preoperative VAS-Leg and the last follow-up VAS-Leg in men (t = 13.48, P < 0.05) and women (t = 26.87, P < 0.05). There were significant differences between preoperative ODI scores (44.84 ± 10.82%) and the last follow-up ODI scores (11.12 ± 5.80%) (t = 10.92, P < 0.05). Preoperative ODI scores and the last follow-up ODI scores were significantly different for men (t = 8.80, P < 0.05) and women (t = 6.63, P < 0.05). All patients received significant pain relief and functional improvement after the surgery. Except for two cases of postoperative dysesthesia and one dural tear, no severe complications occurred. The dysesthesia symptoms of these two patients disappeared within 1 week with the application of dexamethasone and neurotrophic drugs and the dural tear case also recovered well as the dural laceration was small. No poor results were reported and 89.47% of patients achieved excellent or good recovery.
Conclusion
Percutaneous endoscopic lumbar discectomy via the transforaminal approach combined with the interlaminar approach under epidural anesthesia can treat L4/5 and L5/S1 two-level disc herniation safely and effectively.
Introduction
Symptomatic lumbar disc herniation (LDH) is one of the main reasons for low back pain and leg pain and presents a heavy economic and health burden to patients and society1. Generally, spinal surgery is necessary when conservative treatment for LDH fails. The surgical treatments mainly include conventional open surgery, microsurgery, and endoscope-assisted surgery. Even with good results, for conventional open surgery and microsurgery, subsequent damage and complications can occur2, 3.
Endoscopes have been used since the early 1980s to observe the intervertebral space after completing open surgery4. As a typical endoscope-assisted spinal surgery, percutaneous endoscopic lumbar discectomy (PELD) has development significantly over the past two decades. Yeung and Hoogland reported the Yeung endoscopic spine system (YESS) and the transforaminal endoscopic spine system (TESSYS) techniques, respectively. The two techniques are collectively referred to as percutaneous endoscopic transforaminal discectomy (PETD)5, 6. As a crucial and challenged step in PETD, puncture is difficult to achieve in some L5/S1 level disc herniation cases, which leads to surgical failure7. In 2006, Ruetten introduced percutaneous endoscopic interlaminar discectomy (PEID)2. PEID uses a posterior approach, passing through the lamina and ligamentum flavum, which can, consequently, cause dural laceration and other complications8. PELD mainly including PETD and PEID. PELD has become the most popular minimally invasive spine surgery (MISS) for LDH9. Many researches have confirmed that PELD has equivalent effectiveness to conventional surgery and has advantages such as smaller incision, lower blood loss, more rapid recovery, shorter hospital stay, less risk of iatrogenic instability, and less postoperative pain10. However, the inclusion criteria for patients for PELD is strict and limited at the primary application stage. The indication spectrum of PELD has been expanded extensively in recent 10 years due to the introduction of techniques such as foraminoplasty and corresponding instruments like high-speed endoscopic drills, flexible curved forceps, and endoscopic trephines8.
Today, multiple-level LDH is common due to changes in study and work habits. Normally, two-level disc herniation can be treated by conventional lumbar laminectomy11. With the development of MISS and associated surgical instruments, two-level disc herniation can also be resected through the transforaminal approach with just one portal skin incision12. However, the puncture trajectory might not be the best for each level and so that massive bone resection is inevitable. Excessive resection of bone structures might decrease the integrity of the spinal structure and increase the risk of bleeding and iatrogenic lumbar instability13. For patients who have a high iliac crest, a hypertrophic transverse process, or a severely narrowed L5/S1 foramen, the transforaminal approach might not succeed in removing L4/5 and L5/S1 discs with just one portal skin incision because of the bony barriers in the puncture trajectory. For LDH with a narrowed foramen, foraminoplasty has been applied to resect the partial ventral bone of the superior articular process to enlarge the foramen; this approach was first introduced by Knight et al.14. Although foraminoplasty can achieve an extensive surgical view, it may also cause excess bone resection, neural injury, and postoperative complications like incomplete decompression15. To address this, percutaneous bichannel endoscopic surgery was first proposed by Kambin in 1987 to overcome the limited surgical view of PELD. Two skin incisions have been made for endoscopic and instrumental portals, respectively, but for single-level herniation16, 17.
The theory of bichannel surgery inspired our study of the transforaminal approach combined with the interlaminar approach for two-level LDH. Wu et al. conducted a study to describe the two-level PELD technique in the transforaminal approach for single-level highly migrated disc herniation and to investigate its clinical outcomes, which verified the feasibility of two-level PETD18. Owens et al. carried out a study of 2262 cases to determine whether patients with LDH with substantial back pain improve with decompression alone. Approximately half of the patients (1159 cases) underwent two-level discectomy and achieved good pain relief19. Even though the puncture trajectory could be designed separately for the two levels, this would significantly extend the length of the operation and increase radiation exposure. In addition to the transforaminal approach, the interlaminar approach is another well-developed endoscopic technique for LDH surgery3. The interlaminar approach has advantages in the treatment of L5/S1 level disc herniation because it bypasses the blockade of the iliac crest and reduces the difficulty of puncture10, 20. Because this technique involves approaching the herniated disc through the spinal canal, it increases the risk of dural laceration, epidural fibrosis, hematoma formation, and scar tissue formation21, 22. As for L4/5 and L5/S1 two-level herniation, it is difficult to resect two herniated discs through one single laminar interspace. Separate approaches to L4/5 and L5/S1 laminar spaces would increase the damage to the spinal canal and risks of related complications. PETD and PEID have specific indications and advantages for single-level LDH, respectively. Neither PETD nor PEID is a good option for two-level LDH. A combination of the transforaminal approach and the interlaminar approach to treat two-level LDH could make full use of their advantages, which could be a good strategy.
To our knowledge, there is no research exploring the feasibility of PETD combined with PEID for L4/5 and L5/S1 two-level disc herniation. The current study aimed to: (i) discuss the feasibility of PETD combined with PEID; (ii) explore the security and efficacy of the new surgical strategy; and (iii) introduce the early experience of PELD via the transforaminal approach combined with the interlaminar approach for L4/5 and L5/S1 two-level disc herniation.
Materials and Methods
Inclusion and Exclusion Criteria
This study was approved by the institutional review board of our hospital and informed consent was obtained from all individual participants included in the study.
The current study retrospectively analyzed 19 patients who underwent PELD in our department because of L4/5 and L5/S1 two-level disc herniation from January 2015 to June 2016. All patients enrolled met the following inclusion criteria: (i) low back pain and sciatica history, (ii) imaging findings confirming L4/5 and L5/S1 two-level disc herniation, and (iii) failure of standard conservative treatment for at least 3 months. The exclusion criteria were: (i) radiographic findings were not consistent with patients' symptoms or signs, (ii) more than two levels of disc herniation, (iii) far lateral L5/S1 disc herniation, (iv) lumbar instability, severe spinal canal stenosis, cauda equina syndrome, or other spinal diseases, and (v) other severe underlying diseases.
Surgical Procedure
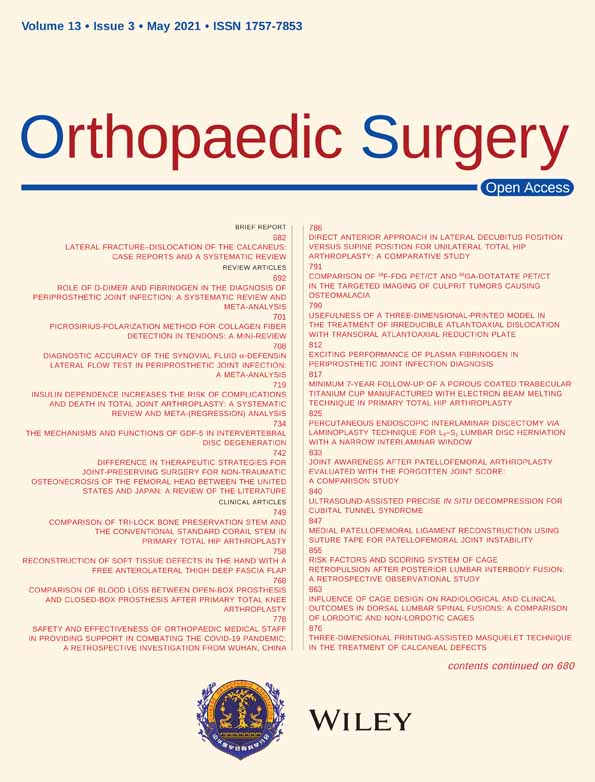
The surgical diagrams of PETD combined with PEID for L4/5 and L5/S1 two-level disc herniation are shown in Fig. 1. PETD for L4/5 was first conducted followed by PEID for L5/S1.
Patient Preparation
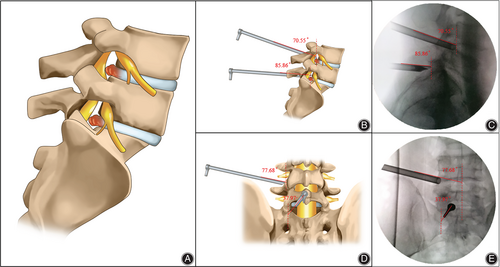
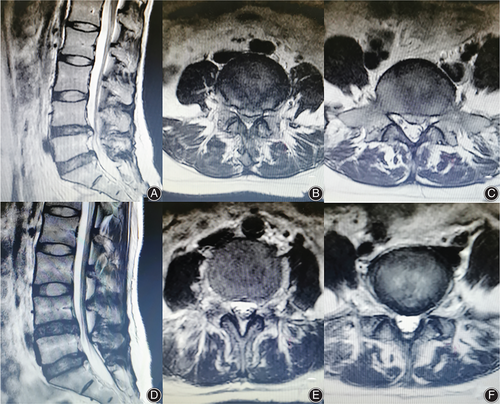
All patients enrolled were confirmed as having L4/5 and L5/S1 two-level disc herniation by preoperative images (Fig. 2A–C) and were hospitalized for the surgery. They were treated by the same medical team. One experienced surgeon who had carried out more than 3000 lumbar surgeries performed PELD for these 19 patients. First, patients were placed on a radiolucent operating table in a prone position under epidural anesthesia. The anesthesia effect should be controlled carefully to preserve motor function and only block sensation during the surgery. The vital signs of patients were monitored during the operation. Then, a grid-like surface locator was used for the surface location (Fig. 2D). The rough shape of anatomical structures, like pedicles and the iliac crest, could be drawn on the skin with the help of intraoperative X-rays (Fig. 2E–G).
Percutaneous Endoscopic Transforaminal Discectomy for L4/5 Level
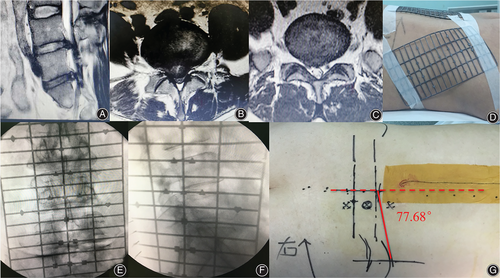
The transforaminal approach was routinely adopted for L4/5 level disc herniation. The puncture trajectory of this level was designed according to preoperative imaging findings and surface location. Then, a puncture needle was inserted into the target, the superior articular process of L5. A crucial procedure, satisfactory puncture is difficult to achieve and may require several attempts and fluoroscopy sometimes. After the confirmation of the ideal position of the puncture needle by X-ray, skin incision and soft tissue dilation were performed. Keeping the guidewire in position, foraminoplasty was performed by bone drill to enlarge the intervertebral foramen. The working cannula was then introduced. Discography was routinely performed to identify the herniated disc. After the confirmation of the ideal position by X-ray, the endoscopic system was introduced through the working cannula. Disc forceps were used to remove the herniated disc (Fig. 3A), and bipolar probes were used to coagulate bleeding points. The decompression was considered sufficient when all the herniated mass had been removed (Fig. 3B), and pulsation of the dural sac was confirmed under endoscopic view.
Percutaneous Endoscopic Interlaminar Discectomy for L5/S1
For L5/S1, puncture could be a huge challenge using the transforaminal approach because of the bony obstacles. In this study, the interlaminar approach was routinely adopted for L5/S1 level disc herniation. According to preoperative imaging findings and surface location, a puncture needle was inserted into the lesion side of the L5/S1 laminar interspace. The following procedures were skin incision and serial dilation. The working cannula was rotated along the dilator and ideal position was confirmed by X-ray (Figs 1C, E and 3C). For some cases with narrowed interlaminar space, the placement of the working cannula was difficult, and a perfect angle of puncture played an important role. The endoscopic system was then introduced through the working cannula. To expose the ligamentum flavum clearly under endoscopic view, soft tissues like muscle and fascia should be removed using grasping forceps, and bleeding points should be coagulated carefully using bipolar probes. The working cannula was rotated forward into the spinal canal, which was opened by partial resection of ligamentum flavum. Anatomy structures like nerve roots and the dural sac could be exposed by irrigation and removing epidural fat. After the identification of the herniated mass, the oblique opening of the working cannula could be used to tract nerve roots and the dural sac by rotation. Then, the extruded tissue should be removed completely with disc forceps. The decompression was considered sufficient when the mobility of the nerve root and the pulsation of the dural sac were confirmed under endoscopic view (Fig. 3D, E).
Closing the Skin Incision
After the satisfactory decompression achieved by PETD combined with PEID. One stitch was typically enough to close each skin incision. All patients received MRI examination om the third day after surgery.
Outcome Measures
The demographic data, operation time, fluoroscopy times, hospital stay, and complications were recorded and analyzed. All patients were followed up in the outpatient department for at least 12 months after their operation. The 10-point visual analogue scale (VAS) was used to assess back pain (VAS-Back) and leg pain (VAS-Leg). VAS-Back and VAS-Leg were recorded on the day before surgery and at 1-day, 3-month, and last follow up after the surgery. Oswestry disability index (ODI) scores and modified MacNab criteria were adopted as functional evaluation methods. ODI scores and modified MacNab criteria were recorded on the day before surgery and at the last follow up after the surgery.
Demographic Data
The demographic data, including age and gender of the 19 patients, were recorded.
Operation Time
The operation time was from anesthesia to incision closure.
Fluoroscopy Times
Fluoroscopy times (frequency) were recorded using a C-arm fluoroscopy machine to evaluate the radiation exposure.
Hospital Stay
Hospital stay was calculated from the first day in the hospital to the day of discharge.
Complications
Complications like postoperative bleeding, neural injury, dysesthesia, dural laceration, and scar tissue formation were recorded after the surgery.
Visual Analogue Scale
The VAS is the most commonly used questionnaire for quantification of pain. It is a continuous scale comprised of a horizontal or vertical line, usually 10 cm in length. For pain intensity, the scale is most commonly anchored by “no pain” (score of 0) and “pain as bad as it could be” (score of 10). A score of 0 is considered no pain, 1–3 mild pain, 4–6 moderate pain, and 7–10 severe pain.
Oswestry Disability Index
The ODI is a principal condition-specific outcome measure used in the management of spinal disorders and to assess patient progress in routine clinical practice. The ODI score system includes 10 sections: pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling. For each section of six statements, the total score is 5. Intervening statements are scored according to rank. If more than one box is marked in each section, the highest score is taken. If all 10 sections are completed, the score is calculated as follows: total scored out of total possible score × 100. If one section is missed (or not applicable) the score is calculated as follows: (total score/(5 × number of questions answered)) × 100%. A score from 0% to 20% is considered mild dysfunction, 21% to 40% moderate dysfunction, 41% to 60% severe dysfunction, and 61% to 80% is considered disability; patients with a score of 81% to 100% are either long-term bedridden or exaggerating the impact of pain on their life.
Modified MacNab Criteria
The modified MacNab criteria were used to evaluate the efficacy of surgery. The modified MacNab criteria include four grades: excellent, good, fair, and poor. Excellent: symptoms disappear completely, with a return to original work and life; good: mild symptoms, with slightly limited activity, and no impact on work and life; fair: symptoms are relieved, activities are limited, affecting normal work and life; poor: there is no difference before and after treatment, with symptoms possibly aggravated.
Statistical Analysis
In this study, SPSS (version 21.0, IBM, Chicago, IL, USA) was used to perform all statistical analyses. Results were presented as mean ± SD. t-tests were used to compare the continuous variables, such as operating time, fluoroscopy times, and VAS-Back, VAS-Leg, and ODI scores. P < 0.05 was regarded as statistically significant.
Results
Follow-up
In all 19 patients, PETD combined with PEID surgery was successfully completed. All patients were followed up (time points: 3, 12, and 18 months) for at least 12 months, with an average follow up of 18.63 ± 3.84 months.
General Results
This study reviewed 12 men and 7 women who underwent PELD for L4/5 and L5/S1 two-level disc herniation. The average age of these patients was 42.21 ± 14.88 years old (range, 18–67 years old). This combined approach took an average operation time of 85.79 ± 12.90 min and average fluoroscopy times of 39.05 ± 4.59 times. The fluoroscopy times during the interlaminar approach for L5/S1 level disc herniation were lower than for the transforaminal approach for L4/5 level disc herniation (t = 7.00, P < 0.05). The fluoroscopy times needed for the transforaminal approach was 26.95 ± 6.41 times, while the number needed for the interlaminar approach was 12.11 ± 3.49 times (Table 1). Furthermore, there was no significant difference for fluoroscopy times between women and men (t = 0.89, P = 0.99).
| Variables | Results |
|---|---|
| Gender (male : female) | 12:7 |
| Age (years old) | 42.21 ± 14.88 |
| Conservative time (months) | 9.68 ± 8.54 |
| Operation time (min) | 85.79 ± 12.90 |
| Fluoroscopy times (frequency) | 39.05 ± 4.59 |
| L4/5 level | 26.95 ± 6.41 |
| L5/S1 level | 12.11 ± 3.49 |
| Hospital stay (days) | 3.32 ± 0.98 |
| Follow up (months) | 18.63 ± 3.84 |
| Complications (cases) | |
| Postoperative dysesthesia | 2 |
| Dural tear | 1 |
Radiographic Improvement
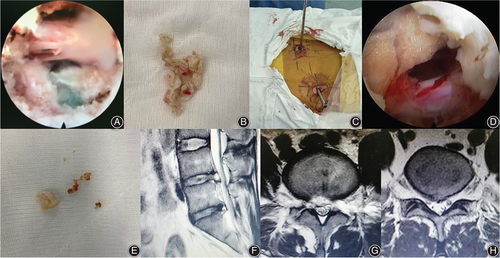
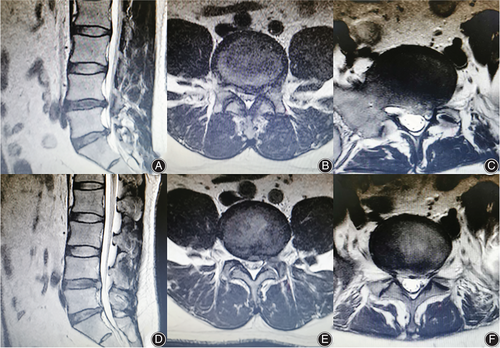
On the postoperative MRI (Day 3), no compression of the nerve was observed, and it was evident that the protruded disc tissue had been removed sufficiently. Sufficient space surrounding the nerve was observed through the postoperative MRI. Combined with the significant pain relief after the surgery, the postoperative MRI (Day 3) revealed satisfactory decompression (Fig. 3F–H). MRI improvement in another two cases is shown in Figs 4 and 5.
Visual Analogue Scale
All patients received significant pain relief after the surgery and the change in the VAS trend at every follow-up time point is presented in Table 2. The VAS-Back changed from 5.58 ± 2.01 before the operation to 4.05 ± 1.08 1 day after the surgery (t = 3.62, P < 0.05). At the last follow up, the average VAS-Back score of these patients reduced from 5.58 ± 2.01 to 2.37 ± 1.01 (t = 7.14, P < 0.05). The VAS-Leg score changed from 7.00 ± 1.56 before the operation to 3.58 ± 1.30 1 day after the surgery (t = 7.53, P < 0.05). The average VAS-Leg score reduced from 7.00 ± 1.56 to 1.63 ± 1.01 (t = 20.97, P < 0.05). Furthermore, for men, the VAS-Back decreased from 5.17 ± 2.13 before the operation to 2.25 ± 1.14 at the last follow up (t = 4.61, P < 0.05) and the VAS-Leg decreased from 6.83 ± 1.85 to 1.50 ± 1.00 (t = 13.48, P < 0.05). For women, the VAS-Back decreased from 6.29 ± 1.70 before the operation to 2.57 ± 0.79 at the last follow up (t = 6.57, P < 0.05) and the VAS-Leg decreased from 7.29 ± 0.95 to 1.86 ± 1.07 (t = 26.87, P < 0.05).
| Variables | Preoperative | One day postoperative | Three months postoperative | Last follow-up |
|---|---|---|---|---|
| VAS-Back | 5.58 ± 2.01 | 4.05 ± 1.08* | 2.74 ± 1.05* | 2.37 ± 1.01* |
| VAS-Leg | 7.00 ± 1.56 | 3.58 ± 1.30* | 2.11 ± 0.94* | 1.63 ± 1.01* |
| ODI scores | 44.84% ± 10.82% | — | — | 11.12% ± 5.80%* |
- * Represents a statistical difference from preoperative data (P < 0.05)
- ODI, Oswestry disability index; visual analogue scale; VAS-Back, visual analogue scale score for back; VAS-Leg, visual analogue scale score for leg.
Oswestry Disability Index
The functional improvement of the patients was satisfactory. All ODI data is shown in Table 2. At the last follow up, the average ODI scores improved from 44.84 ± 10.82% to 11.12 ± 5.80% (t = 10.92, P < 0.05). For male patients, the average ODI scores decreased from 48.50 ± 10.59% preoperatively to 18.00 ± 6.50% at the last follow up (t = 8.80, P < 0.05). For female patients, the average ODI scores decreased from 38.57 ± 9.64% preoperatively to 13.71 ± 3.15% at the last follow up (t = 6.63, P < 0.05).
Modified MacNab Criteria
No poor result was reported and 89.47% of patients achieved an excellent or good recovery (Table 3).
| Variables | Cases | Percentage |
|---|---|---|
| Excellent | 4 | 21.05 |
| Good | 13 | 68.42 |
| Fair | 2 | 10.53 |
| Poor | 0 | — |
Complications
There were two cases of postoperative dysesthesia. The dysesthesia symptom of these two patients disappeared in 1 week with the application of dexamethasone and neurotrophic drugs. There was one case of dural tear at L5/S1 level. The dural laceration was too small to repair, and the patient recovered well. No recurrence was observed during the follow up (Table 1).
Discussion
Percutaneous Endoscopic Transforaminal Discectomy and Percutaneous Endoscopic Interlaminar Discectomy have Specific Advantages for Single-Level Lumbar Disc Herniation and Their Combination Could Treat Two-Level Lumbar Disc Herniation Well
Over the past two decades, PELD has progressed tremendously. The transforaminal approach is the most frequently used PELD technique because of its advantages such as local anesthesia, less damage to bone structure, and its minimally invasive approach to the spinal canal3, 23. Two levels of adjacent herniated discs could be removed using the transforaminal approach with one portal skin incision12. However, under certain conditions, like a high iliac crest, two separated transforaminal puncture trajectories are necessary to remove L4/5 and L5/S1 discs. A transforaminal puncture at L5/S1 level could be difficult and time-consuming for patients with a high iliac crest and a hypertrophic transverse process24, 25. In such cases, the interlaminar approach might be a good option as it bypasses the blockade of the iliac crest and the transverse process10. However, this technique invades into the spinal canal and retracts the nerve root and the dural sac. Compared with the transforaminal approach, there is increased risk of epidural fibrosis, nerve irritation, and other complications during the interlaminar approach21, 22. The combination of the transforaminal approach and the interlaminar approach could make full use of their advantages.
Early Experience of Percutaneous Endoscopic Lumbar Discectomy via Transforaminal Approach Combined with Interlaminar Approach for L4/5 and L5/S1 Two-Level Disc Herniation
For the patients with L4/5 and L5/S1 two-level disc herniation enrolled in the present study, the transforaminal approach was adopted for the upper level disc. The puncture strategy, which was quite familiar for spinal surgeons who were good at minimally invasive spine surgery, could be easily designed and successfully performed26, 27. As access to this level was less challenging, an ideal position of the puncture needle could be achieved with low-dose radiation exposure. The working cannula could be smoothly placed without massive osseous resection. In addition, operations under the endoscopic system were convenient as the working cannula could be introduced in an ideal direction for better exposure of the herniated level. For L5/S1 disc herniation, the interlaminar approach was chosen in this study. Because the puncture requirement in the interlaminar approach was relatively low, the puncture needle could be easily inserted with low-dose radiation exposure too. Because the working cannula was introduced into the lesion side of the laminar interspace directly, operating on the herniated mass under the endoscopic system was not difficult. In the current study, no severe complications occurred, and all patients received immediate pain relief after the surgery. The functional improvement was satisfactory. Indeed, 89.47% of patients had an excellent or good recovery at the last follow up. The surgical strategy introduced in the current study was safe and effective.
Comparison Between Percutaneous Endoscopic Lumbar Discectomy and Percutaneous Endoscopic Interlaminar Discectomy
Both the transforaminal approach and the interlaminar approach could treat LDH successfully28. A randomized controlled study with 2 years of follow up proved that PELD via both the transforaminal approach and the interlaminar approach could achieve an equal treatment effect to the microsurgical technique for LDH3. By reviewing LDH patients who received PELD more than 10 years previously, a retrospective study demonstrated that the long-term outcomes of PELD via both the transforaminal approach and the interlaminar approach were good too29. Nevertheless, there are still differences between the two techniques. According to a randomized controlled study, the interlaminar approach showed advantages in operation time and fluoroscopy times over the transforaminal approach in PELD for L5/S1 disc herniation. The treatment efficiency between the two approaches was similar10. Another retrospective study demonstrated that the transforaminal approach would be better for shoulder type, centrally located, and recurrent disc herniation. The interlaminar approach might be a better choice for axillary type and migrated discs30.
The anesthesia strategy was another issue to consider when choosing PELD with the transforaminal approach combined with the interlaminar approach. For the transforaminal approach, local anesthesia was normally recommended because it reduced the risk of exiting nerve root injury31. General anesthesia, which is normally adopted for the interlaminar approach10, 30, has been applied in the transforaminal approach before32. However, it might not be a wise choice because of the increased risk of neural injury during the transforaminal approach. Even though local anesthesia could be applied in the interlaminar approach too33, the anesthesia effect might not be satisfactory for a two-level surgery. Epidural anesthesia, which could be controlled to preserve motor function and only block sensation by adjusting the anesthetic dosage used34, was chosen in this study. The anesthesia effect was good and no anesthesia-associated complications occurred.
Limitations
There are several limitations of this study. First, this is a retrospective study with a small sample size. Large-scale studies are necessary to further evaluate the surgical effect of this strategy. Second, there is no comparison with other surgical techniques. The current study introduced an effective and safe strategy for the treatment of L4/5 and L5/S1 two-level disc herniation, but further efforts should be devoted to finding an ideal treatment for L4/5 and L5/S1 two-level disc herniation
Conclusion
Percutaneous endoscopic lumbar discectomy via the transforaminal approach combined with the interlaminar approach under epidural anesthesia can treat L4/5 and L5/S1 two-level disc herniation safely and effectively.